Medicine:Cherry-red spot
| Cherry-red spot | |
|---|---|
| Medical diagnostics | |
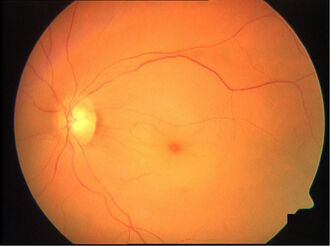 Typical central retinal artery occlusion with cherry-red spot, retinal oedema and narrowing of the vessels. |
A cherry-red spot is a finding in the macula of the eye in a variety of lipid storage disorders and in central retinal artery occlusion.[1] It describes the appearance of a small circular choroid shape as seen through the fovea centralis. [2] Its appearance is due to a relative transparency of the macula; storage disorders cause the accumulation of storage material within the cell layers of the retina, however, the macula, which is relatively devoid of cellular layers, does not build up this material, and thus allows the eye to see through the macula to the red choroid below.[3]
The sign was first described by Warren Tay, founding member of the British Ophthalmological Society, in 1881, with reference to a patient with Tay–Sachs disease.
The cherry red spot is seen in central retinal artery occlusion, appearing several hours after the blockage of the retinal artery occurs.[4] The cherry red spot is seen because the macula receives its blood supply from the choroid, supplied by the long and short posterior ciliary arteries, while the surrounding retina is pale due to retinal artery infarction.[5] It is also seen in several other conditions, classically Tay–Sachs disease, but also in Niemann–Pick disease, Sandhoff disease, and mucolipidosis.
Differential diagnosis of cherry-red spot at macula
- Metabolic Storage Diseases:,[6][7]
- Congenital developmental diseases (e.g., Leber's congenital amaurosis)
- Hereditary/ Familial:
- Vascular (e.g., central retinal artery occlusion)
- Drugs:
- Poisoning:
- Blunt ocular trauma
See also
- Lipid storage disease
References
- ↑ General Practice Notebook
- ↑ Medical Dictionary
- ↑ Suvarna JC, Hajela SA. Cherry-red spot. J Postgrad Med 2008;54:54-7.
- ↑ Rakel, Robert E., Textbook of Family Medicine, 7th ed, Chapter 53
- ↑ ""USMLE First AID 2010 page 417
- ↑ Hereditary Ocular Disease, University of Arizona
- ↑ Fenichel's Clinical Pediatric Neurology: A Signs and Symptoms Approach, 2013;127 ff
 |


