Biology:Monoamine oxidase inhibitor
| Monoamine oxidase inhibitor | |
|---|---|
| Drug class | |
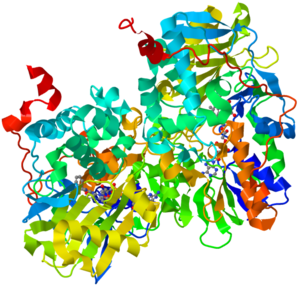 Ribbon diagram of human monoamine oxidase B, from PDB: 1GOS | |
| Class identifiers | |
| Synonyms | MAOI, RIMA |
| Use | Treatment of major depressive disorder, atypical depression, Parkinson's disease, and several other disorders |
| ATC code | N06AF |
| Mechanism of action | Enzyme inhibitor |
| Biological target | Monoamine oxidase enzymes: MAO-A and/or MAO-B |
| External links | |
| MeSH | D008996 |
Monoamine oxidase inhibitors (MAOIs) are a class of drugs that inhibit the activity of one or both monoamine oxidase enzymes: monoamine oxidase A (MAO-A) and monoamine oxidase B (MAO-B). They are best known as effective antidepressants, especially for treatment-resistant depression and atypical depression.[1] They are also used to treat panic disorder, social anxiety disorder, Parkinson's disease, and several other disorders.
Reversible inhibitors of monoamine oxidase A (RIMAs) are a subclass of MAOIs that selectively and reversibly inhibit the MAO-A enzyme. RIMAs are used clinically in the treatment of depression and dysthymia. Due to their reversibility, they are safer in single-drug overdose than the older, irreversible MAOIs,[2] and weaker in increasing the monoamines important in depressive disorder.[3] RIMAs have not gained widespread market share in the United States.
Medical uses
MAOIs have been found to be effective in the treatment of panic disorder with agoraphobia,[4] social phobia,[5][6][7] atypical depression[8][9] or mixed anxiety disorder and depression, bulimia,[10][11][12][13] and post-traumatic stress disorder,[14] as well as borderline personality disorder,[15] and obsessive–compulsive disorder (OCD).[16][17] MAOIs appear to be particularly effective in the management of bipolar depression according to a retrospective-analysis from 2009.[18] There are reports of MAOI efficacy in OCD, trichotillomania, body dysmorphic disorder, and avoidant personality disorder, but these reports are from uncontrolled case reports.[19]
MAOIs can also be used in the treatment of Parkinson's disease by targeting MAO-B in particular (therefore affecting dopaminergic neurons), as well as providing an alternative for migraine prophylaxis. Inhibition of both MAO-A and MAO-B is used in the treatment of clinical depression and anxiety.
MAOIs appear to be particularly indicated for outpatients with dysthymia complicated by panic disorder or hysteroid dysphoria.[20]
Newer MAOIs such as selegiline (typically used in the treatment of Parkinson's disease) and the reversible MAOI moclobemide provide a safer alternative[19] and are now sometimes used as first-line therapy.
Side effects
Hypertensive crisis
People taking MAOIs generally need to change their diets to limit or avoid foods and beverages containing tyramine, which is found in products such as cheese, soy sauce, and salami.[21] If large amounts of tyramine are consumed, they may develop a hypertensive crisis, which can be fatal.[22] Examples of foods and beverages with potentially high levels of tyramine include cheese, Chianti wine, and pickled fish.[23] Excessive concentrations of tyramine in blood plasma can lead to hypertensive crisis by increasing the release of norepinephrine (NE), which causes blood vessels to constrict by activating alpha-1 adrenergic receptors.[24] Ordinarily, MAO-A would destroy the excess NE; when MAO-A is inhibited, however, NE levels get too high, leading to dangerous increases in blood pressure.
RIMAs are displaced from MAO-A in the presence of tyramine,[25] rather than inhibiting its breakdown in the liver as general MAOIs do. Additionally, MAO-B remains free and continues to metabolize tyramine in the stomach, although this is less significant than the liver action. Thus, RIMAs are unlikely to elicit tyramine-mediated hypertensive crisis; moreover, dietary modifications are not usually necessary when taking a reversible inhibitor of MAO-A (i.e., moclobemide) or low doses of selective MAO-B inhibitors (e.g., selegiline 6 mg/24 hours transdermal patch).[24][26][27]
Drug interactions
The most significant risk associated with the use of MAOIs is the potential for drug interactions with over-the-counter, prescription, or illegally obtained medications, and some dietary supplements (e.g., St. John's wort, tryptophan). It is vital that a doctor supervise such combinations to avoid adverse reactions. For this reason, many users carry an MAOI-card, which lets emergency medical personnel know what drugs to avoid (e.g. adrenaline [epinephrine] dosage should be reduced by 75%, and duration is extended).[23]
Tryptophan supplements can be consumed with MAOIs, but can result in transient serotonin syndrome.[28]
MAOIs should not be combined with other psychoactive substances (antidepressants, painkillers, stimulants, including prescribed, OTC and illegally acquired drugs, etc.) except under expert care. Certain combinations can cause lethal reactions; common examples including SSRIs, tricyclics, MDMA, meperidine,[29] tramadol, dextromethorphan,[30] whereas combinations with LSD, psilocybin, or DMT appear to be relatively safe.[31][citation needed] Drugs that affect the release or reuptake of epinephrine, norepinephrine, serotonin or dopamine typically need to be administered at lower doses due to the resulting potentiated and prolonged effect. MAOIs also interact with tobacco-containing products (e.g. cigarettes) and may potentiate the effects of certain compounds in tobacco.[32][33][34] This may be reflected in the difficulty of smoking cessation, as tobacco contains naturally occurring MAOI compounds in addition to the nicotine.[32][33][34]
While safer than general MAOIs, RIMAs still possess significant and potentially serious drug interactions with many common drugs; in particular, they can cause serotonin syndrome or hypertensive crisis when combined with almost any antidepressant or stimulant, common migraine medications, certain herbs, or most cold medicines (including decongestants, antihistamines, and cough syrup).[citation needed]
Ocular alpha-2 agonists such as brimonidine and apraclonidine are glaucoma medications which reduce intraocular pressure by decreasing aqueous production. These alpha-2 agonists should not be given with oral MAOIs due to the risk of hypertensive crisis.[35]
Withdrawal
Antidepressants including MAOIs have some dependence-producing effects, the most notable one being a discontinuation syndrome, which may be severe especially if MAOIs are discontinued abruptly or too rapidly. The dependence-producing potential of MAOIs or antidepressants in general is not as significant as benzodiazepines, however. Discontinuation symptoms can be managed by a gradual reduction in dosage over a period of days, weeks or sometimes months to minimize or prevent withdrawal symptoms.[36]
MAOIs, as with most antidepressant medication, may not alter the course of the disorder in a significant, permanent way, so it is possible that discontinuation can return the patient to the pre-treatment state.[37] This consideration complicates prescribing between an MAOI and an SSRI, because it is necessary to clear the system completely of one drug before starting another. One physician organization recommends the dose to be tapered down over a minimum of four weeks, followed by a two-week washout period.[38] The result is that a depressed patient will have to bear the depression without chemical help during the drug-free interval. This may be preferable to risking the effects of an interaction between the two drugs.[38]
Mechanism of action
MAOIs act by inhibiting the activity of monoamine oxidase, thus preventing the breakdown of monoamine neurotransmitters and thereby increasing their availability. There are two isoforms of monoamine oxidase, MAO-A and MAO-B. MAO-A preferentially deaminates serotonin, melatonin, epinephrine, and norepinephrine. MAO-B preferentially deaminates phenethylamine and certain other trace amines; in contrast, MAO-A preferentially deaminates other trace amines, like tyramine, whereas dopamine is equally deaminated by both types.
Reversibility
The early MAOIs covalently bound to the monoamine oxidase enzymes, thus inhibiting them irreversibly; the bound enzyme could not function and thus enzyme activity was blocked until the cell made new enzymes. The enzymes turn over approximately every two weeks. A few newer MAOIs, a notable one being moclobemide, are reversible, meaning that they are able to detach from the enzyme to facilitate usual catabolism of the substrate. The level of inhibition in this way is governed by the concentrations of the substrate and the MAOI.[39]
Harmaline found in Peganum harmala, Banisteriopsis caapi, and Passiflora incarnata is a reversible inhibitor of monoamine oxidase A (RIMA).[40]
Selectivity
In addition to reversibility, MAOIs differ by their selectivity of the MAO enzyme subtype. Some MAOIs inhibit both MAO-A and MAO-B equally, other MAOIs have been developed to target one over the other.
MAO-A inhibition reduces the breakdown of primarily serotonin, norepinephrine, and dopamine; selective inhibition of MAO-A allows for tyramine to be metabolised via MAO-B.[41] Agents that act on serotonin if taken with another serotonin-enhancing agent may result in a potentially fatal interaction called serotonin syndrome or with irreversible and unselective inhibitors (such as older MAOIs), of MAO a hypertensive crisis as a result of tyramine food interactions is particularly problematic with older MAOIs. Tyramine is broken down by MAO-A and MAO-B, therefore inhibiting this action may result in its excessive build-up, so diet must be monitored for tyramine intake.
MAO-B inhibition reduces the breakdown mainly of dopamine and phenethylamine so there are no dietary restrictions associated with this. MAO-B would also metabolize tyramine, as the only differences between dopamine, phenethylamine, and tyramine are two phenylhydroxyl groups on carbons 3 and 4. The 4-OH would not be a steric hindrance to MAO-B on tyramine.[42] Selegiline is selective for MAO-B at low doses, but non-selective at higher doses.
History
The knowledge of MAOIs began with the serendipitous discovery that iproniazid was a potent MAO inhibitor (MAOI).[43] Originally intended for the treatment of tuberculosis, in 1952, iproniazid's antidepressant properties were discovered when researchers noted that the depressed patients given iproniazid experienced a relief of their depression. Subsequent in vitro work led to the discovery that it inhibited MAO and eventually to the monoamine theory of depression. MAOIs became widely used as antidepressants in the early 1950s. The discovery of the 2 isoenzymes of MAO has led to the development of selective MAOIs that may have a more favorable side-effect profile.[44]
The older MAOIs' heyday was mostly between the years 1957 and 1970.[41] The initial popularity of the 'classic' non-selective irreversible MAO inhibitors began to wane due to their serious interactions with sympathomimetic drugs and tyramine-containing foods that could lead to dangerous hypertensive emergencies. As a result, the use by medical practitioners of these older MAOIs declined. When scientists discovered that there are two different MAO enzymes (MAO-A and MAO-B), they developed selective compounds for MAO-B, (for example, selegiline, which is used for Parkinson's disease), to reduce the side-effects and serious interactions. Further improvement occurred with the development of compounds (moclobemide and toloxatone) that not only are selective but cause reversible MAO-A inhibition and a reduction in dietary and drug interactions.[45][46] Moclobemide, was the first reversible inhibitor of MAO-A to enter widespread clinical practice.[47]
A transdermal patch form of the MAOI selegiline, called Emsam, was approved for use in depression by the Food and Drug Administration in the United States on 28 February 2006.[48]
List of MAO inhibiting drugs
Marketed MAOIs
- Nonselective MAO-A/MAO-B inhibitors
- Hydrazine (antidepressant)
- Isocarboxazid (Marplan)
- Hydracarbazine
- Phenelzine (Nardil, Nardelzine)
- Non-hydrazines
- Tranylcypromine (Parnate, Jatrosom)
- Hydrazine (antidepressant)
- Selective MAO-A inhibitors
- Bifemelane (Alnert, Celeport) (available in Japan)
- Methylthioninium chloride (Urelene blue, Provayblue, Proveblue)
- Moclobemide (Aurorix, Manerix, Moclamine)
- Pirlindole (Pirazidol) (available in Russia)
- Selective MAO-B inhibitors
- Rasagiline (Azilect)
- Selegiline (Deprenyl, Eldepryl, Emsam, Zelapar)
- Safinamide (Xadago)
Linezolid is an antibiotic drug with weak, reversible MAO-inhibiting activity.[49]
The antibiotic furazolidone also has MAO-inhibiting activity [50]
Methylthioninium chloride (methylene blue), the antidote indicated for drug-induced methemoglobinemia on the World Health Organization's List of Essential Medicines, among a plethora of other off-label uses, is a highly potent, reversible MAO inhibitor.[51]
The Food and Drug Administration (FDA) has approved these MAOIs to treat depression:[52]
- Isocarboxazid (Marplan)
- Phenelzine (Nardil)
- Selegiline (Emsam)
- Tranylcypromine (Parnate)
MAOIs that have been withdrawn from the market
- Nonselective MAO-A/MAO-B inhibitors
- Hydrazines
- Benmoxin (Nerusil, Neuralex)
- Iproclozide (Sursum)
- Iproniazid (Marsilid, Iprozid, Ipronid, Rivivol, Propilniazida)
- Mebanazine (Actomol)
- Nialamide (Niamid)
- Octamoxin (Ximaol, Nimaol)
- Pheniprazine (Catron)
- Phenoxypropazine (Drazine)
- Pivalylbenzhydrazine (Tersavid)
- Safrazine (Safra) (discontinued worldwide except for Japan)
- Non-hydrazines
- Caroxazone (Surodil, Timostenil)
- Hydrazines
- Selective MAO-A inhibitors
- Minaprine (Cantor)
- Toloxatone (Humoryl)
List of RIMAs
Marketed pharmaceuticals
- Moclobemide (Aurorix, Manerix, Moclamine)
Other pharmaceuticals
- Brofaromine (Consonar)
- Caroxazone (Surodil, Timostenil)
- Eprobemide (Befol)[53]
- Methylene blue
- Metralindole (Inkazan)
- Minaprine (Cantor)
- Pirlindole (Pirazidol)
Naturally occurring RIMAs in plants
Research compounds
- Amiflamine (FLA-336)
- Befloxatone (MD-370,503)
- Cimoxatone (MD-780,515)
- Esuprone
- Sercloremine (CGP-4718-A)
- Tetrindole
- CX157 (TriRima)
References
- ↑ Cristancho, Mario A. (20 November 2012). "Atypical Depression in the 21st Century: Diagnostic and Treatment Issues". Psychiatric Times. http://www.psychiatrictimes.com/major-depressive-disorder/atypical-depression-21st-century-diagnostic-and-treatment-issues. Retrieved 23 November 2013.
- ↑ "Moclobemide poisoning: toxicokinetics and occurrence of serotonin toxicity". British Journal of Clinical Pharmacology 56 (4): 441–450. 2003. doi:10.1046/j.1365-2125.2003.01895.x. PMID 12968990.
- ↑ "Neuroscience Education Institute > Activities > 2012CurbConsultPosted". http://www.neiglobal.com/Activities/2012CurbConsultPosted/tabid/328/Default.aspx.
- ↑ "Therapeutic response to phenelzine in patients with panic disorder and agoraphobia with panic attacks". The Journal of Clinical Psychiatry 48 (2): 55–9. February 1987. PMID 3542985.
- ↑ "Phenelzine vs atenolol in social phobia. A placebo-controlled comparison". Archives of General Psychiatry 49 (4): 290–300. April 1992. doi:10.1001/archpsyc.49.4.290. PMID 1558463.
- ↑ "Pharmacotherapy of social phobia. A controlled study with moclobemide and phenelzine". The British Journal of Psychiatry 161 (3): 353–60. September 1992. doi:10.1192/bjp.161.3.353. PMID 1393304.
- ↑ "Cognitive behavioral group therapy vs phenelzine therapy for social phobia: 12-week outcome". Archives of General Psychiatry 55 (12): 1133–41. December 1998. doi:10.1001/archpsyc.55.12.1133. PMID 9862558.
- ↑ "Treatment of atypical depression with cognitive therapy or phenelzine: a double-blind, placebo-controlled trial". Archives of General Psychiatry 56 (5): 431–7. May 1999. doi:10.1001/archpsyc.56.5.431. PMID 10232298.
- ↑ "Phenelzine v imipramine in atypical depression. A preliminary report". Archives of General Psychiatry 41 (7): 669–77. July 1984. doi:10.1001/archpsyc.1984.01790180039005. PMID 6375621.
- ↑ "Treatment of bulimia with phenelzine. A double-blind, placebo-controlled study". Archives of General Psychiatry 41 (11): 1105–9. November 1984. doi:10.1001/archpsyc.1983.01790220095015. PMID 6388524.
- ↑ "A double-blind placebo-controlled comparison of phenelzine and imipramine in the treatment of bulimia in atypical depressives". The International Journal of Eating Disorders 15 (1): 1–9. January 1994. doi:10.1002/1098-108X(199401)15:1<1::AID-EAT2260150102>3.0.CO;2-E. PMID 8124322.
- ↑ "A double-blind trial of phenelzine in bulimia". Journal of Psychiatric Research 19 (2–3): 485–9. 1985. doi:10.1016/0022-3956(85)90058-5. PMID 3900362.
- ↑ "Phenelzine vs placebo in 50 patients with bulimia". Archives of General Psychiatry 45 (5): 471–5. May 1988. doi:10.1001/archpsyc.1988.01800290091011. PMID 3282482.
- ↑ "A pilot study of phenelzine in the treatment of post-traumatic stress disorder". The British Journal of Psychiatry 150 (2): 252–5. February 1987. doi:10.1192/bjp.150.2.252. PMID 3651684.
- ↑ "Efficacy of phenelzine and haloperidol in borderline personality disorder". Archives of General Psychiatry 50 (5): 377–85. May 1993. doi:10.1001/archpsyc.1993.01820170055007. PMID 8489326.
- ↑ Vallejo, J.; Olivares, J.; Marcos, T.; Bulbena, A.; Menchón, J. M. (2 January 2018). "Clomipramine versus Phenelzine in Obsessive–Compulsive Disorder". British Journal of Psychiatry 161 (5): 665–670. doi:10.1192/bjp.161.5.665. PMID 1422616.
- ↑ Annesley, P. T. (29 January 2018). "Nardil Response in a Chronic Obsessive Compulsive". British Journal of Psychiatry 115 (523): 748. doi:10.1192/bjp.115.523.748. PMID 5806868.
- ↑ "Revisiting the effectiveness of standard antidepressants in bipolar disorder: are monoamine oxidase inhibitors superior?". Psychopharmacology Bulletin 42 (2): 64–74. 2009. PMID 19629023.
- ↑ 19.0 19.1 "Reversible and irreversible monoamine oxidase inhibitors in other psychiatric disorders". Acta Psychiatrica Scandinavica. Supplementum 360 (S360): 29–34. 1990. doi:10.1111/j.1600-0447.1990.tb05321.x. PMID 2248064.
- ↑ http://www.psycom.net/hysteroid.html "MAO inhibitors in mental disease: Their current status". Monoamine Oxidase Enzymes. 23. 1987. 121–38. doi:10.1007/978-3-7091-8901-6_8. ISBN 978-3-211-81985-2.
- ↑ Gillman, Peter Kenneth (September 2018). "A reassessment of the safety profile of monoamine oxidase inhibitors: elucidating tired old tyramine myths" (in en). Journal of Neural Transmission 125 (11): 1707–1717. doi:10.1007/s00702-018-1932-y. ISSN 0300-9564. PMID 30255284.
- ↑ "Practical guide for prescribing MAOIs: debunking myths and removing barriers". CNS Spectrums 17 (1): 2–10. March 2012. doi:10.1017/S109285291200003X. PMID 22790112. https://pubmed.ncbi.nlm.nih.gov/22790112/.
- ↑ 23.0 23.1 Mosher, Clayton James, and Scott Akins. Drugs and Drug Policy : The Control of Consciousness Alteration. Thousand Oaks, Calif.: Sage, 2007.[page needed]
- ↑ 24.0 24.1 Stahl, Stephen (2011). Case Studies: Stahl's Essential Psychopharmacology.
- ↑ "Meta-analysis of the reversible inhibitors of monoamine oxidase type A moclobemide and brofaromine for the treatment of depression". Neuropsychopharmacology 20 (3): 226–47. March 1999. doi:10.1016/S0893-133X(98)00075-X. PMID 10063483.
- ↑ FDA. "EMSAM Medication Guide". https://www.fda.gov/downloads/Drugs/DrugSafety/ucm088589.pdf.
- ↑ "The advent of a new generation of monoamine oxidase inhibitor antidepressants: pharmacologic studies with moclobemide and brofaromine". Clinical Neuropharmacology 16 (Suppl 2): S1–7. 1993. PMID 8313392.
- ↑ "The serotonin syndrome". The New England Journal of Medicine 352 (11): 1112–20. March 2005. doi:10.1056/NEJMra041867. PMID 15784664.
- ↑ Pharmacology from H.P. Rang, M.M. Dale, J.M. Ritter, P.K. Moore, year 2003, chapter 38
- ↑ "MHRA PAR Dextromethorphan hydrobromide, p. 12". http://www.mhra.gov.uk/home/groups/par/documents/websiteresources/con146863.pdf.
- ↑ Malcolm, B., & Thomas, K (2022). "Serotonin toxicity of serotonergic psychedelics". Psychopharmacology 239 (6): 1881–1891. doi:10.1007/s00213-021-05876-x. PMID 34251464.
- ↑ 32.0 32.1 "Monoamine oxidases and tobacco smoking". The International Journal of Neuropsychopharmacology 4 (1): 33–42. March 2001. doi:10.1017/S1461145701002188. PMID 11343627.
- ↑ 33.0 33.1 "Brain monoamine oxidase A inhibition in cigarette smokers". Proceedings of the National Academy of Sciences of the United States of America 93 (24): 14065–9. November 1996. doi:10.1073/pnas.93.24.14065. PMID 8943061. Bibcode: 1996PNAS...9314065F.
- ↑ 34.0 34.1 "Inhibition of monoamine oxidase B in the brains of smokers". Nature 379 (6567): 733–6. February 1996. doi:10.1038/379733a0. PMID 8602220. Bibcode: 1996Natur.379..733F.
- ↑ Kanski's Clinical Ophthalmology, 8th Edition (2016). Brad Bowling. ISBN:978-0-7020-5572-0 978-0-7020-5573-7 p. 332
- ↑ "Dependence potential of antidepressants compared to benzodiazepines". Progress in Neuro-Psychopharmacology & Biological Psychiatry 26 (5): 939–43. June 2002. doi:10.1016/S0278-5846(02)00209-9. PMID 12369270.
- ↑ "Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the prevention of relapse and recurrence in major depression". Journal of Consulting and Clinical Psychology 76 (3): 468–77. June 2008. doi:10.1037/0022-006X.76.3.468. PMID 18540740.
- ↑ 38.0 38.1 "Switching patients from phenelzine to other antidepressants". Royal Australian and New Zealand College of Psychiatrists. 2020-05-11. https://www.ranzcp.org/files/communications/medicine-alerts/phenelzine-switching-advice-_final-11052020.aspx.
- ↑ "Reversible inhibitors of monoamine oxidase-A (RIMAs): robust, reversible inhibition of human brain MAO-A by CX157". Neuropsychopharmacology 35 (3): 623–31. February 2010. doi:10.1038/npp.2009.167. PMID 19890267.
- ↑ Edward J. Massaro (2002). Handbook of Neurotoxicology. Humana Press. ISBN 9780896037960. https://books.google.com/books?id=2c2K-epbCDQC&pg=PA237.
- ↑ 41.0 41.1 "[Inhibitory monoamine oxidases of the new generation]" (in pl). Polski Merkuriusz Lekarski 3 (13): 1–4. July 1997. PMID 9432289.
- ↑ "Structural insights into the mechanism of amine oxidation by monoamine oxidases A and B". Archives of Biochemistry and Biophysics 464 (2): 269–76. August 2007. doi:10.1016/j.abb.2007.05.006. PMID 17573034.
- ↑ "Antidepressants: From MAOIs to SSRIs and more". Indian Journal of Psychiatry 53 (2): 180–2. April 2011. doi:10.4103/0019-5545.82567. PMID 21772661.
- ↑ "Current place of monoamine oxidase inhibitors in the treatment of depression". CNS Drugs 27 (10): 789–97. October 2013. doi:10.1007/s40263-013-0097-3. PMID 23934742.
- ↑ "Monoamine oxidase inhibitors. An update on drug interactions". Drug Safety 14 (4): 219–27. April 1996. doi:10.2165/00002018-199614040-00002. PMID 8713690.
- ↑ "Biochemistry and pharmacology of reversible inhibitors of MAO-A agents: focus on moclobemide". Journal of Psychiatry & Neuroscience 18 (5): 214–25. November 1993. PMID 7905288.
- ↑ "Moclobemide: a reversible inhibitor of monoamine oxidase type A". British Journal of Hospital Medicine 49 (7): 497–9. 1993. PMID 8490690.
- ↑ "FDA Approves Emsam (Selegiline) as First Drug Patch for Depression" (Press release). U.S. Food and Drug Administration. 28 February 2006. Archived from the original on 21 November 2009. Retrieved 19 November 2009.
- ↑ "Serotonin toxicity associated with the use of linezolid: a review of postmarketing data". Clinical Infectious Diseases 42 (11): 1578–83. June 2006. doi:10.1086/503839. PMID 16652315.
- ↑ A.M. Timperio; H.A. Kuiper & L. Zolla (February 2003). "Identification of a furazolidone metabolite responsible for the inhibition of amino oxidases". Xenobiotica 33 (2): 153–167. doi:10.1080/0049825021000038459. PMID 12623758.
- ↑ "Azure B, a metabolite of methylene blue, is a high-potency, reversible inhibitor of monoamine oxidase". Toxicology and Applied Pharmacology 258 (3): 403–9. February 2012. doi:10.1016/j.taap.2011.12.005. PMID 22197611.
- ↑ "An option if other antidepressants haven't helped" (in en). https://www.mayoclinic.org/diseases-conditions/depression/in-depth/maois/art-20043992.
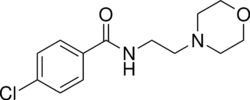
- ↑ "Antidepressant Befol Synthesized Via Interaction of 4-Chloro-N-(3-chloropropyl)benzamide with Morpholine". Pharmaceutical Chemistry Journal. 0091-150X 38 (7): 381–384. 1 July 2004. doi:10.1023/B:PHAC.0000048439.38383.5f.
- ↑ van Diermen, Daphne; Marston, Andrew; Bravo, Juan; Reist, Marianne; Carrupt, Pierre-Alain; Hostettmann, Kurt (2009-03-18). "Monoamine oxidase inhibition by Rhodiola rosea L. roots" (in en). Journal of Ethnopharmacology 122 (2): 397–401. doi:10.1016/j.jep.2009.01.007. ISSN 0378-8741. PMID 19168123. https://www.sciencedirect.com/science/article/pii/S037887410900021X.
 |



