Risk ratio
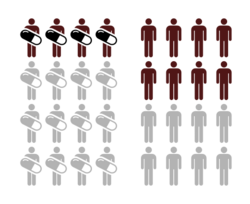
In epidemiology, risk ratio (RR) or relative risk is the ratio of the probability of an outcome in an exposed group to the probability of an outcome in an unexposed group. It is computed as [math]\displaystyle{ I_e / I_u }[/math], where [math]\displaystyle{ I_e }[/math] is the incidence in the exposed group, and [math]\displaystyle{ I_u }[/math] is the incidence in the unexposed group.[1] Together with risk difference and odds ratio, risk ratio measures the association between the exposure and the outcome.[2]
Statistical use and meaning
Risk ratio is used in the statistical analysis of the data of experimental, cohort and cross-sectional studies, to estimate the strength of the association between treatments or risk factors, and outcome.[2][3] For example, it is used to compare the risk of an adverse outcome when receiving a medical treatment versus no treatment (or placebo), or when exposed to an environmental risk factor versus not exposed.
Assuming the causal effect between the exposure and the outcome, values of RR can be interpreted as follows:
- RR = 1 means that exposure does not affect the outcome;
- RR < 1 means that the risk of the outcome is decreased by the exposure;
- RR > 1 means that the risk of the outcome is increased by the exposure.
Usage in reporting
Risk ratio is commonly used to present the results of randomized controlled trials.[4] This can be problematic, if risk ratio is presented without the absolute measures, such as absolute risk, or risk difference.[5] In the case when the base rate of the outcome is low, large or small values of risk ratio may not translate to significant effect, and the importance of the effect to the public health can be overestimated. Equivalently, in the case when the base rate of the outcome is high, values of the risk ratio close to 1 may still result in a significant effect and can be underestimated. Thus, presentation of both absolute and relative measures is recommended.[6]
Inference
Risk ratio can be estimated from a 2x2 contingency table:
| Group | ||
|---|---|---|
| Experimental (E) | Control (C) | |
| Events (E) | EE | CE |
| Non-events (N) | EN | CN |
The point estimate of the risk ratio is
- [math]\displaystyle{ RR = \frac{EE/(EE + EN)}{CE/(CE + CN)} = \frac{EE(CE + CN)}{CE(EE + EN)}. }[/math]
The sampling distribution of the [math]\displaystyle{ \log(RR) }[/math]is approximately normal,[7] with standard error
- [math]\displaystyle{ SE(\log(RR)) = \sqrt{\frac{EN}{EE(EE + EN)} + \frac{CN}{CE(CE + CN)}}. }[/math]
The [math]\displaystyle{ 1 - \alpha }[/math] confidence interval for the [math]\displaystyle{ \log(RR) }[/math] is then
- [math]\displaystyle{ CI_{1 - \alpha}(\log(RR)) = \log(RR)\pm SE(\log(RR))\times z_\alpha, }[/math]
where [math]\displaystyle{ z_\alpha }[/math] is the standard score for the chosen level of significance[8][9]. To find the confidence interval around the RR itself, the two bounds of the above confidence interval can be exponentiated.[8]
In regression models, the exposure is typically included as a indicator variable along with other factors that may affect risk. The risk ratio is usually reported as calculated for the mean of the sample values of the explanatory variables.
Comparison to the odds ratio
Risk ratio is different from the odds ratio, although it asymptotically approaches it for small probabilities of outcomes. If EE is substantially smaller than EN, then EE/(EE + EN) [math]\displaystyle{ \scriptstyle\approx }[/math] EE/EN. Similarly, if CE is much smaller than CN, then CE/(CN + CE) [math]\displaystyle{ \scriptstyle\approx }[/math] CE/CN. Thus, under the rare disease assumption
- [math]\displaystyle{ RR = \frac{EE(CE + CN)}{CE(EE + EN)} \approx \frac{EE \cdot CN}{EN \cdot CE} = OR. }[/math]
In epidemiological research, the odds ratio is commonly used for case-control studies, as the risk ratio cannot be estimated.[10][failed verification]
In fact, the odds ratio has much broader use in statistics, since logistic regression, often associated with clinical trials, works with the log of the odds ratio, not risk ratio. Because the record of the odds ratio is estimated as a linear function of the explanatory variables, the estimated odds ratio for 70-year-olds and 60-year-olds associated with the type of treatment would be the same in logistic regression models where the outcome is associated with drug and age, although the risk ratio might be significantly different. In cases like this, statistical models of the odds ratio often reflect the underlying mechanisms more efficiently.
Since risk ratio is a more intuitive measure of effectiveness, the distinction is important especially in cases of medium to high probabilities. If action A carries a risk of 99.9% and action B a risk of 99.0% then the risk ratio is just over 1, while the odds associated with action A are more than 10 times higher than the odds with B.
In statistical modelling, approaches like poisson regression (for counts of events per unit exposure) have risk ratio interpretations: the estimated effect of an explanatory variable is multiplicative on the rate and thus leads to a risk ratio. Logistic regression (for binary outcomes, or counts of successes out of a number of trials) must be interpreted in odds-ratio terms: the effect of an explanatory variable is multiplicative on the odds and thus leads to an odds ratio.
Bayesian interpretation
We could assume a disease noted by [math]\displaystyle{ D }[/math], and no disease noted by [math]\displaystyle{ \neg D }[/math], exposure noted by [math]\displaystyle{ E }[/math], and no exposure noted by [math]\displaystyle{ \neg E }[/math]. Risk ratio can be written as
- [math]\displaystyle{ RR = \frac {P(D\mid E)}{P(D\mid \neg E)} = \frac {P(E\mid D)/P(\neg E\mid D)}{P(E)/P(\neg E)}. }[/math]
This way the risk ratio can be interpreted in Bayesian terms as the posterior ratio of the exposure (i.e. after seeing the disease) normalized by the prior ratio of exposure.[11] If the posterior ratio of exposure is similar to that of the prior, the effect is approximately 1, indicating no association with the disease, since it didn't change beliefs of the exposure. If on the other hand, the posterior ratio of exposure is smaller or higher than that of the prior ratio, then the disease has changed the view of the exposure danger, and the magnitude of this change is the risk ratio.
Numerical example
| Example of risk reduction | |||
|---|---|---|---|
| Experimental group (E) | Control group (C) | Total | |
| Events (E) | EE = 15 | CE = 100 | 115 |
| Non-events (N) | EN = 135 | CN = 150 | 285 |
| Total subjects (S) | ES = EE + EN = 150 | CS = CE + CN = 250 | 400 |
| Event rate (ER) | EER = EE / ES = 0.1, or 10% | CER = CE / CS = 0.4, or 40% | |
| Equation | Variable | Abbr. | Value |
|---|---|---|---|
| CER - EER | absolute risk reduction | ARR | 0.3, or 30% |
| (CER - EER) / CER | relative risk reduction | RRR | 0.75, or 75% |
| 1 / (CER − EER) | number needed to treat | NNT | 3.33 |
| EER / CER | risk ratio | RR | 0.25 |
| (EE / EN) / (CE / CN) | odds ratio | OR | 0.167 |
| (CER - EER) / CER | preventable fraction among the unexposed | PFu | 0.75 |
See also
References
- ↑ Dictionary of Epidemiology (6th ed.). Oxford University Press. pp. 245, 252. doi:10.1093/acref/9780199976720.001.0001. ISBN 978-0-19-939006-9. http://www.oxfordreference.com/view/10.1093/acref/9780199976720.001.0001/acref-9780199976720.
- ↑ 2.0 2.1 "Proportions, odds, and risk". Radiology 230 (1): 12–9. January 2004. doi:10.1148/radiol.2301031028. PMID 14695382.
- ↑ Riegelman, Richard K. (2005). Studying a study and testing a test: how to read the medical evidence (5th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 389. ISBN 978-0-7817-4576-5. OCLC 56415070.
- ↑ "Reporting of attributable and relative risks, 1966-97". Lancet 351 (9110): 1179. April 1998. doi:10.1016/s0140-6736(05)79123-6. PMID 9643696.
- ↑ "Relative risk versus absolute risk: one cannot be interpreted without the other". Nephrology, Dialysis, Transplantation 32 (suppl_2): ii13-ii18. April 2017. doi:10.1093/ndt/gfw465. PMID 28339913.
- ↑ "CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials". BMJ 340: c869. March 2010. doi:10.1136/bmj.c869. PMID 20332511.
- ↑ "Standard errors, confidence intervals, and significance tests". StataCorp LLC. https://www.stata.com/support/faqs/stat/2deltameth.html.
- ↑ 8.0 8.1 Szklo, Moyses; Nieto, F. Javier (2019). Epidemiology : beyond the basics (4th. ed.). Burlington, Massachusetts: Jones & Bartlett Learning. pp. 488. ISBN 9781284116595. OCLC 1019839414. https://www.worldcat.org/oclc/1019839414.
- ↑ Katz, D.; Baptista, J.; Azen, S. P.; Pike, M. C. (1978). "Obtaining Confidence Intervals for the Risk Ratio in Cohort Studies". Biometrics 34 (3): 469–474. doi:10.2307/2530610. http://www.jstor.org/stable/2530610.
- ↑ "When can odds ratios mislead? Odds ratios should be used only in case-control studies and logistic regression analyses". BMJ 317 (7166): 1155–6; author reply 1156–7. October 1998. doi:10.1136/bmj.317.7166.1155a. PMID 9784470.
- ↑ Statistical Methods in Medical Research (Fourth ed.). Blackwell Science Ltd. 2002. doi:10.1002/9780470773666. ISBN 978-0-470-77366-6.
External links