Classification of distal radius fractures
There are a number of ways to classify distal radius fractures. Classifications systems are devised to describe patterns of injury which will behave in predictable ways, to distinguish between conditions which have different outcomes or which need different treatments. Most wrist fracture systems have failed to accomplish any of these goals and there is no consensus about the most useful one.
At one extreme, a stable undisplaced extra-articular fracture has an excellent prognosis. On the other hand, an unstable, displaced intra-articular fracture is difficult to treat and has a poor prognosis without operative intervention.[citation needed]
Eponyms such as Colles', Smith's, and Barton's fractures are discouraged.[by whom?]
Anatomy
An anatomic description of the fracture is the easiest way to describe the fracture, determine treatment, and assess stability.[according to whom?]
- Articular incongruity
- Volar or dorsal tilt
- Radial inclination
- Radial length and ulnar variance
- Comminution of the fracture (the amount of crumbling at the fracture site)
- Open (compound fracture) vs. closed injury
- Associated ulnar styloid fracture
- Associated soft tissue injuries
Articular incongruity
The articular joint's surface must be smooth for it to function properly. Irregularity may result in radiocarpal arthritis, pain, and stiffness. More than 1 mm of incongruity places the patient at a high risk for post-traumatic arthritis. Significant articular incongruity typically occurs in young patients after high energy injuries. If the surface is very irregular and cannot be reconstructed, then the only option may be a fusion of the joint.
Volar vs dorsal tilt
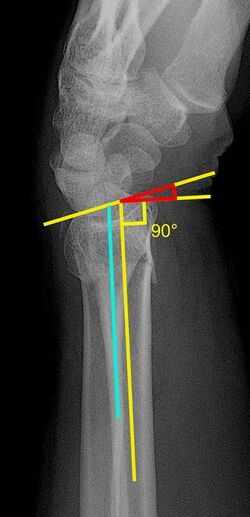
A dorsal tilt of a distal radius fracture is shown in red in image at right. The angulation goes between:[1]
- A line drawn between the distal ends of the articular surface of the radius on a lateral X-ray.
- A line that is perpendicular to the diaphysis of the radius.
Sometimes, the diaphysis of the radius is hard to distinguish from the ulna, and a line between them (turquoise line in image) may be used instead.[2]
The angle normally has volar tilt of 11° to 12°. The most common fracture pattern usually demonstrates malalignment of this angle and collapse in a dorsal direction. A dorsal tilt of 0° (11° - 12° deviation from normal anatomic position) causes a substantial risk of developing pain and impaired function.[3] After closed reduction, a residual dorsal tilt of a maximum of 5° (16° - 17° deviation) is regarded as the maximal residual angle for a satisfactory result.[3]
Radial inclination
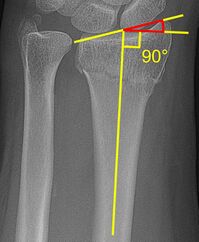
The radial inclination of a distal radius fracture is shown in red in image at right. The angle is measured between:[4][5]
- A line drawn between the distal ends of the articular surface of the radius on a AP view of the wrist.
- A line that is perpendicular to the diaphysis of the radius.
Radial inclination is normally 21-25°.[6]
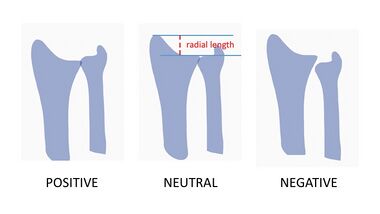
Radial length and ulnar variance
Radial length is an important consideration in distal radius fractures. Radial length should be between 9-12mm.[7] Distal radius fractures typically result in loss of length as the radius collapses from the loading force of the injury. With increasing relative lengthening of the uninjured ulna (positive ulnar variance), ulnar impaction syndrome may occur. Ulnar impaction syndrome is a painful condition of excessive contact and wear between the ulna and the carpus with an associated is a degenerative tear of the TFCC.
Melone classification
The system that comes closest to directing treatment has been devised by Melone. This system breaks distal radius fractures down into 4 components: radial styloid, dorsal medial fragment, volar medial fragment, and radial shaft. The two medial fragments (which together create the lunate fossa) are grouped together as the medial complex.[8]
| Type | Description | Note |
|---|---|---|
| I | No displacement of medial complex
|
Fracture is stable after closed reduction |
| II | Unstable depression fracture of lunate fossa ("die-punch")
|
|
| III | Type II fracture plus a 'spike' of the radius volarly | May impinge on median nerve |
| IV | Split fracture
|
Unstable |
| V | Explosion injuries
|
Often associated with diaphyseal comminution |
Frykman classification
Though the Frykman classification system has traditionally been used, there is little value in its use because it does not help direct treatment. This system focuses on articular and ulnar involvement. The classification is as follows:[9]
| Radius Fracture | Ulna Fracture | |
|---|---|---|
| Absent | Present | |
| Extra-articular | I | II |
| Intra-articular involving radiocarpal joint | III | IV |
| Intra-articular involving DRUJ (distal radio-ulnar joint) | V | VI |
| Intra-articular involving both radiocarpal & DRUJ | VII | VIII |
Universal classification
The Universal classification system is descriptive but also does not direct treatment. Universal codes are:[10]
| Type | Location | Displacement | Sub-type |
|---|---|---|---|
| I | Extra-articular | Undisplaced | |
| II | Extra-articular | Displaced | A: Reducible, stable
B: Reducible, unstable C: Irreducible |
| III | Intra-articular | Undisplaced | |
| IV | Intra-articular | Displaced | A: Reducible, stable
B: Reducible, unstable C: Irreducible D: Complex |
AO/OTA classification
Widely used system that includes 27 subgroups. Three main groups based on fracture joint involvement (A - extra-articular, B - partial articular, C - complete articular). Classification further defined based on level of comminution and direction of displacement. A qualification (Q) modifier can be added to classify associated ulnar injury.[8]
Fernandez classification
Simplified system developed in response to AO classification, intended to be based off injury mechanism with more treatment-oriented classifications (treatment suggestions not meant to be used as rigid guidelines but can be used to help decision making on a case-by-case basis)[11]
| Type | Description | Stability | Number of Fragments | Associated Lesions (see below) | Recommended Treatment |
|---|---|---|---|---|---|
| I | Bending fracture - metaphysis | Stable or unstable | 2 main fragments with variable metaphyseal comminution | Uncommon | Stable -> conservative
Unstable -> percutaneous pinning or external fixation |
| II | Shearing fracture - articular surface | Unstable | 2, 3, comminuted | Less uncommon | Open reduction with screw-plate fixation |
| III | Compression fracture - articular surface | Stable or unstable | 2, 3, 4, comminuted | Common |
|
| IV | Avulsion fracture, radiocarpal fracture, dislocation | Unstable | 2 (radial/ulnar styloids), 3, comminuted | Frequent
(especially ligamentous injury) |
Closed or open reudction with pin/screw fixation or tension wiring |
| V | Combined fracture (high-energy injury) - Often intra-articular and open | Unstable | Comminuted | Always present | Combined treatment |
Note: Associated Lesions include carpal ligament injury, nerve injury, tendon damage, and compartment syndrome
References
- ↑ Piva Neto, Antonio; Lhamby, Fabio Colla (2011). "Fixação das fraturas da extremidade distal do rádio pela técnica de kapandji modificada: avaliação dos resultados radiológicos". Revista Brasileira de Ortopedia 46 (4): 368–373. doi:10.1590/S0102-36162011000400004. ISSN 0102-3616.
- ↑ Paresh K Desai. "Colles fracture". https://radiopaedia.org/articles/colles-fracture. Retrieved 2016-12-18.
- ↑ 3.0 3.1 Page 347 in: William P. Cooney (2011). The Wrist: Diagnosis and Operative Treatment. Lippincott Williams & Wilkins. ISBN 9781451148268.
- ↑ Jack A Porrino Jr. (2015-10-20). "Distal Radial Fracture Imaging". http://emedicine.medscape.com/article/398406-overview. Retrieved 2016-12-18.
- ↑ Pankaj Kumar Mishra; Manoj Nagar; Suresh Chandra Gaur; Anuj Gupta (2016). "Morphometry of distal end radius in the Indian population: A radiological study". Indian Journal of Orthopaedics 50 (6). PMC 5122255. http://www.ijoonline.com/article.asp?issn=0019-5413;year=2016;volume=50;issue=6;spage=610;epage=615;aulast=Mishra.
- ↑ Page 783 in: Joshua Broder (2011). Diagnostic Imaging for the Emergency Physician. Elsevier Health Sciences. ISBN 9781437735871.
- ↑ 7.0 7.1 Adam, Greenspan (2015). Orthopedic imaging : a practical approach. Beltran, Javier (Professor of radiology) (Sixth ed.). Philadelphia. ISBN 9781451191301. OCLC 876669045.
- ↑ 8.0 8.1 Court-Brown, Charles; Heckman, James D.; McKee, Michael; McQueen, Margaret M.; Ricci, William; III, Paul Tornetta (2014) (in en). Rockwood and Green's Fractures in Adults. Lippincott Williams & Wilkins. ISBN 9781469884820.
- ↑ Wheeless Online
- ↑ Brown, David E.; Neumann, Randall D. (2004) (in en). Orthopedic Secrets. Elsevier Health Sciences. p. 182. ISBN 9781560535416. https://books.google.com/books?id=yujV5S_TP_UC&pg=PA182.
- ↑ "AO Surgery Reference" (in en). https://www2.aofoundation.org/wps/portal/!ut/p/a1/04_Sj9CPykssy0xPLMnMz0vMAfGjzOKN_A0M3D2DDbz9_UMMDRyDXQ3dw9wMDAwCTYEKIvEocDQnTr8BDuBoQEi_l35Uek5-EtipkY55ScYW6fpRRalpqUWpRXqlRUDhjJKSgmIrVQNVg_Lycr30_Pz0nFS95PxcVQNsWjLyi0v0I1BV6hfkhkZU-aSGAwBJYqzy/dl5/d5/L2dJQSEvUUt3QS80SmlFL1o2XzJPMDBHSVMwS09PVDEwQVNFMUdWRjAwME0z/?bone=Radius&segment=Distal&soloState=lyteframe&contentUrl=srg/popup/further_reading/23/Fernandez/23_fernandez_class.jsp.
