Medicine:Atraumatic Restorative Treatment (ART)
Atraumatic Restorative Treatment (ART)[1] is a method for cleaning out tooth decay (dental caries) from teeth using only hand instruments (dental hatchet and spoon-excavator) and placing a filling. It does not use rotary dental instruments (dental drills) to prepare the tooth and can be placed in settings with no access to dental equipment. No drilling or local anaesthetic injections (LA) are required. ART is considered a conservative approach, not only because it removes the decayed tissue with hand instruments, avoiding removing more tissue necessary which preserves as much tooth structure as possible, but also because it avoids pulp irritation and minimises patient discomfort. ART can be used for small, medium and deep cavities (where decay has not reached the tooth nerve dental pulp)[1] caused by dental caries. In shallow/medium sized cavities (lesions), the decayed tissue removal is carried out until the soft tissue (demineralised dentine) is completely removed and harder tissue is reached (firm dentine). In deeper cavities (lesions that reach more than 2/3 of dentine thickness on a radiograph), the removal of the decay must be carried out more carefully in order to avoid reaching the tooth’s pulp (dental nerve). Soft tissue should be left on the cavity floor. The decision on how much decay to remove (whether to carry out the decay removal to firm dentine or stop when soft dentine has been reached) depends on:
- The depth of the cavity - a filling needs to have a minimum thickness of material placed to ensure it has enough filling material to be strong;[2]
- The possibility of reaching the tooth’s pulp (the nerve is exposed sometimes when deep cavities are accessed with rotary burs or vigorously with hand instruments, compromising the tooth’s vitality).
Dental radiographs need to be taken to evaluate the depth of the cavity and extension of decay. If too deep and close to the pulp, only the soft decayed tissue is removed from the cavity floor to avoid the risk of pulp exposure.
ART is suitable for both primary (baby teeth) and permanent dentition (adult teeth) and has a large evidence base supporting it (see “Effectiveness” section).
Background and History
ART makes restorative oral care more accessible
ART was firstly introduced by the dentist Jo Frencken in 1985, Tanzania (Frencken et al., 1996),[3] where the management of decayed teeth in children living in a deprived area was challenging because access to dental treatments using drills was restricted by limited dentist availability and a lack of electricity and/or piped water. The pattern of disease/ care meant that children’s teeth generally decayed until they caused pain/infection and removal was required. At that time, the dentists tried to use only hand instruments to open and/or enlarge small cavities, and selectively remove the decayed tissue, followed by the placement of an adhesive filling; Glass Ionomer Cement (GIC), which also releases fluoride and helps the tooth’s “recovery” from decay (remineralisation). This treatment was tested in clinical trials and found to be effective.
Although ART was initially developed in response to the needs of populations with less access to dental care, this minimally invasive dental treatment (preserving as much as possible the dental tissues) had similar outcomes to more invasive treatments (local anaesthetic and drilling the tooth with dental bur). This means that it suitable for use in any type of setting (from deprived communities to dental clinics) and it has been widely adopted into mainstream care. Due to its “atraumatic approach”, it has also been proven to be beneficial for patients with dental anxiety or learning disabilities, even where there is adequate dental care, as neither drilling nor local anaesthetics are required.
More recently, during the International Caries Consensus Collaboration (ICCC) meeting held in Leuven in 2015, ART was recommended by an international group of experts in cariology, restorative and paediatric dentistry as an option to treat decayed primary and permanent teeth with decay where restorative options were indicated, such as cavities that were difficult to clean using only toothbrushes and fluoride toothpaste.[4][2]
Concept
There are two different ART procedures with different aims:
i) Preventive (ART fissure sealant for non-cavitated teeth); and
ii) Restorative (ART filling for decayed and cavitated teeth)[3][5][6][7]
A. Preventive (ART fissure sealant)
The adult teeth that erupt behind the baby back teeth, have deep grooves (fissures) and are more susceptible to accumulating food debris and dental plaque which can stagnate and lead to decay. They are also difficult to toothbrush properly. While they are erupting, they are very susceptible to decay and it is very difficult to keep them dry enough to use a resin-based sealant material successfully. However, sealing the tooth pits and fissures helps make cleaning the tooth easier and stops the accumulation of plaque biofilm so a high viscosity glass ionomer cement (HVGIC), is used to seal these teeth, covering the pits and fissures. This is done by cleaning the tooth, placing a layer of HVGIC over the back teeth and using finger pressure to keep it in place and dry until the HVGIC material sets. Excess material is removed. If necessary, it is adjusted to fit the bite using hand instruments.
B. Restorative (ART filling)
Where the enamel (the hard-outer surface of the tooth has cavitated or even has a small breach due to tooth decay, the cavity can be enlarged with special hand instruments (when necessary) to enable access to the soft decayed tooth tissue. After removing as much decay as necessary, the cavity is cleaned with water, dried and filled with the HVGIC. The filling seals the cavity preventing food debris and dental plaque stagnating inside the cavity. It also promotes remineralisation of the dental tissues affected by decay. When the cavity is sealed any decay and bacteria that has been left on the floor of the cavity cannot get access to oxygen and sugar and will not continue.
Effectiveness sealants
- The retention rate of ART sealants using HVGIC[8] has improved significantly compared to low and medium viscosity-viscosity glass-ionomers previously used[9]
- ART sealants appear to have a high caries preventive effect.[10]
- ART/HVGIC sealants are effective in controlling dentine-carious-lesion development in pits and fissures.[1]
- Occurrence of secondary carious lesions are rare at the tooth-restoration interface of single-surface ART/HVGIC restorations in primary teeth.[1]
ART Sealants Versus Resin-based Sealants
- Compared to resin composite sealants, ART/HVGIC sealants appear to be more effective in erupting permanent molars where moisture control is hard to achieve due to the “water like” nature of the glass-ionomer material and less sensitive technique.[11] However, moisture control should always be attempted as much as possible for a better material survival.
- The full- and partial-retention survival of ART/HVGIC is lower compared to resin based sealants.[11]
- 4 systematic reviews and meta-analyses, one of which is a Cochrane review. show that there is no difference in terms of dentine caries-lesion preventive effects between both types of sealants.[11][12][13][14][15]
Indications
ART fillings can be used for:[7][16]
- Single surface cavities in primary (baby teeth) and permanent (adult) teeth;
- Multiple-surface cavities in primary teeth, if no other option is available/suitable (e.g. Hall Technique);
- Non-frankly cavitated lesion (presenting a shadow under the enamel) that are not suitable for sealing; and
- Children, uncooperative, disabled and anxious patients.
Contraindications
ART fillings should not be used when there is:[7][16]
- Swelling or a fistula near the decayed tooth;
- Pulpal exposure (the nerve of the tooth is visible);
- History of pain from the teeth to be treated;
- Lesions that cannot be accessed with hand instruments (proximal side);
- Multi-surface cavities in permanent teeth; and
- Teeth that are badly broken down, which are unrestorable.
Instruments
- Mouth Mirror;
- Dental probe;
- Pair of dental tweezers;
- Dental Hatchet;
- Spoon Excavator (small and medium);
- Flat plastic instrument and a carver to shape the filling material; and
- Paper mixing pad and a plastic spatula (for mixing if powder/liquid GIC is used).
Procedure
- Ensure the patient understands the treatment to be carried out, has consented and knows what steps are involved. Advice to patients include:
- Cleaning the tooth will sound “scratchy” or “picky” during the procedures.
- The patient is advised not to eat for the first hour after the treatment is finished.
- Inspect the cavitated tooth
- Make sure the tooth is clean and dry either directly or indirectly using a dental mirror.
- Any plaque or food debris within the cavity is gently removed using a toothbrush or wet cotton pellet.
- Isolation (avoiding moisture on the tooth)
- The tooth to be restored (filled with a restorative material) is isolated with cotton wool to keep it dry.
- Other methods, such as a “Dry Guard” and saliva ejectors can also be used to keep the tooth dry.
- Cavity access and initial preparation
- If the cavity is too small to be able to clean and place a filling, then the entrance is widened by placing the dental hatchet into the cavity. The instrument is turned around one direction and then backwards, like turning a key in a lock.
- Soft, decayed tissue is removed by using a spoon excavator with circular scooping movements, avoiding pressure (the spoon excavator must be sharp to also remove unsupported enamel – the hardest part of the tooth).
- Peripheral margin modification
- Any remaining thin demineralised and unsupported overhanging enamel is removed with sharp spoon excavators or dental hatchets
- Cleaning and conditioning the prepared cavity·
- The cavity and the occlusal surfaces, including the pits and fissures, are cleaned with wet cotton pellets.
- Dentine conditioner (polyacrylic acid) is applied to the entire cavity and adjacent fissures to promote a better bond between the GIC filling and the tooth using a disposable dental micro brush or cotton pellet, rubbing it against the dental tissues for 15 seconds.
- The cavity is washed immediately with wet cotton pellets and dried with dry cotton pellets.
- Mixing and restoring the cavity with HVGIC
- The dental nurse/assistant mixes the HVGIC (encapsulated or powder/liquid) and the operating clinician slightly overfills the cavity with the material, also placing it in the remaining pits and fissures.
- The clinician places their gloved finger with slight pressure over the filling surface (this allows the material to accommodate better to the cavity shape) for a full 2 minutes until the material has set (press-finger technique).[17]
Effectiveness
- ART is effective for restoring single surface cavities in both primary and permanent dentition and should be considered as the preferred option.[10]
- ART shows higher failure rates for multi-surface carious lesions restorations when compared to single surface lesions.[1] Meta-analysis concluded that the mean annual failure rate for multiple surface ART restorations in primary teeth are still high.[9]
- Very few studies have investigated the survival (success) of ART restorations in multiple-surface cavities in permanent teeth, and it is not possible to draw conclusions yet.[10]
- ART preserves the tooth structure as only the soft demineralised tissue in deep cavities is removed.[5][6]
- Low pain and discomfort are experienced. Dental anxiety is lower when performing ART when compared to conventional drill and fill methods.[3][18][19]
Comparison with conventional fillings
- Systematic reviews and meta-analyses show that there are no differences between ART/HVGIC restorations in terms of longevity in primary teeth (for both single and multiple surface lesions) compared to the conventional methods using either amalgam[20][21][22] or resin composite.[23][24]
- Systematic reviews and meta-analyses have shown that there are no differences between ART restorations for single surfaces lesions in permanent teeth when compared to conventional filling methods.[20][25][26]
- However, a 2017 Cochrane Review on ART could not draw any conclusions about ART/HVGIC restorations compared to amalgam/composite restoration due to the low quality of the evidence.[27]
Evidence
Below is the summary of success of ART/HVGIC restorations in different type of cavities[10]
| Type of cavities using ART/HVGIC | Evidence of restoration success |
| Single surface in posterior primary teeth (baby back teeth) for first 2 years | High (Survival percentage = 94.3% (± 1.5) )[10] |
| Multiple-surface in posterior primary teeth for first 2 years | Medium to Low (Survival percentage = 65.4% (± 3.9))[10] |
| Single surface in posterior permanent teeth (back adult teeth) for first 3 years | High (Survival percentage = 87.1% (± 3.2) ) |
| Multiple surface in posterior permanent teeth for the first | No conclusion can be drawn due to insufficient data[10] |
Although originally developed for use in developing countries, due to its “atraumatic” approach, ART has become increasingly well accepted in developed countries/[28] Although ART alone is insufficient to improve the oral health of people in low- and middle-income countries in a sustainable manner, the WHO Collaborating Centre of Oral Health Care Planning and Future Scenarios in Nijmegen has included it in the Basic Package of Oral Care (BPOC). This aims to improve the oral health of deprived communities in a cost-effective manner. This package comprises three components:
- Oral Urgent Treatment (OUT) – relief of oral pain (through extracting non-repairable painful teeth; and other urgent treatment), first aid for oral infections and dental trauma;
- Affordable Fluoride Toothpaste (AFT) – through oral health promotion and prevention of caries and gingivitis through toothbrushing using toothpaste fluoride; and
- Atraumatic Restorative Treatment (ART) - operative and preventive caries management through the use of the ART approach (sealants and fillings), introduction of dental care to young children and patients with dental fear/anxiety, presenting with mental or physical disabilities or home-bound elderly and those stay in nursing homes; and ART as an intermediate treatment to stabilize conditions in high risk caries clinical situations.[29]
ART in multiple surface cavities
ART/HVGIC restorations can be successfully used in single surface lesions in both primary (SDCEP)[30] and permanent teeth.[1] For multi-surface lesions (tooth decay that has spread across more than one surface of the tooth), systematic reviews and meta-analyses show that the mean failure rate of ART/HVGIC restorations is higher than occlusal lesions and with a wide range of success.[10] In these cases, there is evidence that the Hall Technique be more successful.
As for multiple surface cavities in posterior permanent teeth, there is insufficient data to draw conclusions about its use and effectiveness. Therefore, in this case, alternative treatments should be attempted. These might include selective caries removal followed by restoration using conventional filling materials (usually resin composite) depending on the clinical situation.[30]
Advantages and limitations
Advantages
- Conserves tooth structure;[17][31][32]
- Non-aerosol generating (considered important in the acute COVID-19 pandemic situation and maybe similar for other respiratory infectious disease outbreaks)
- Does not require a dental surgery and can be carried out in school or some settings;
- Minimises trauma (related to dental anxiety);
- Biologically friendly approach[33]
- As an introduction of dental care to young children, it is more acceptable than the conventional “drill and fill” method.[3][18][19]
- Is a patient-friendly approach for children, adults with dental anxiety/phobia, elderly and special-needs patients;[34][35][36][37][38] and
- Low cost as hand instruments and HVGIC which are relatively cheaper are used[39][40]
Reasons for using hand instruments
- More “patient friendly” as hand instruments cause less pain and discomfort compared to rotary instruments.[35][41][18][42]
- Increases accessibility of restorative care to wider populations (can be carried out in deprived communities, clinics, patient’s home or hospital)[43]
- Minimally invasive, therefore causes less trauma to the teeth and preserve teeth structure;
- Hand instruments are easily available and less expensive compared to electrically driven dental equipment;
- Because no “live” dentine is removed and pressure on the dentinal tubules is avoided, local anaesthetic (LA) is not required thus reduces psychological trauma to patients; and
- Infection control is more straightforward; hand instruments can be cleaned and sterilised easily.
Reasons for using HVGIC
- Low cost[17][9]
- Allows the use of “press-finger” method to place the material into the cavity – some excess will spread along the margins and over the pits and fissures, acting as an ART sealant and providing extra preventive benefit;
- Releases fluoride that may be sustained for very long period of time which helps in tissue remineralisation;
- Adhesive and bio-compatible, i.e. does not irritate pulp or gingiva and has a co-efficient of thermal expansion similar to tooth structure;
- Less potential for recurrent caries
- Since HVGIC relies on chemical adhesion to the tooth there is less need to remove healthy tissue to create mechanical retention; and
- Easy to manipulate and repair if there are any defects or excess material.
- Can achieve good cavity seal
- Seals decay into the tooth away from sugar and oxygen which it needs to progress. This helps in managing dental carious lesions without removing additional tooth and without damaging the pulp[27][17]
Limitations
- No conclusion has been made on the long-term survival rates of GIC ART restorations and sealants, the longest study reported so far is of three years duration[44] although this is likely to be a good lifespan for primary teeth;
- The technique might not be readily accepted by oral healthcare personnel because they may not be prepared to carry out selective removal of decay;
- The possibility of hand fatigue from the use of hand instruments; and
- GIC produced by hand mixing might be relatively unstandardized, even if the manufacturer’s instructions are followed.
In combination with other approaches
Use with conditioner
HVGIC has been proven to perform better when a dentine conditioner (Cavity conditioner; GC)[45][46] in used prior to placement of the restorative material. The conditioner is made up of 20% polyacrylic acid and 3% aluminum chloride hexahydrate. It helps to improve the bonding of GIC to the tooth surface by eliminating the smear layer and debris.[47] It also has the advantage of sealing the dentinal tubules to eliminate sensitivity.[47]
Chemo-Mechanical approach
This approach comprises the use of chemical material (eg. Papacarie and Carisolv) which contains enzymes and proteases that soften the decayed tooth structure before removing the decay mechanically).[48][49][50][51][52][53] In ART, these chemical materials can be used in conjunction with hand instruments while removing dental caries as they have the advantage of improving treatment comfort by reducing the pain, heat and vibration experienced, make ART more accepted for children.[54][55]
Examples of use in different countries
| Brazil[56] | Atraumatic Restorative Treatment (ART) for a disadvantaged Brazilian Community:
“Training oral health personnel in October 2001, three oral health teams were included in the Family Health Programme in this area. These teams and other dentists in the public health network were trained by a university teacher in the area, to perform ART restorations using glass ionomer cement.” |
|---|---|
| South Africa[57] | Introducing the Atraumatic Restorative Treatment (ART) approach in Liberian Refugee Services:
“In 1997, twelve lay refugees in the Liberian refugee camp were trained in basic oral health care including ART according to WHO training module. This primary oral health programme for refugees were revisited after 3 years in December 1999. The 12 trained refugees maintained an oral health clinic in the camp, where patients were treated with ART.” |
| Sri Lanka[58][59] | Atraumatic Restorative Treatment (ART) Programme in Sri Lanka (Based on WHO 2008 Oral Health Database):
“Once a month a team of dentists and about 10 dental students from the Division of Community Dentistry visit a primary school in the Kandy area. The faculty receive requests from the Principals of schools, mainly from impoverished areas where the schoolchildren otherwise will not receive any dental care. The students, supervised by the doctors, carry out the examination and treatment in a well-lit classroom or outside in the school premises. While the children are waiting for treatment, they are given oral health education by the dental students. ART is carried out on about 25-30 children on one visit. Around 250 students are provided with ART per year.” |
| Turkey[60] | Atraumatic Restorative Treatment (ART) Programme in some rural areas of Turkey:
“From year 1997, dentists and often dental students visit the rural areas including Bagivar, a small town in Anatolia. ART restorations are performed in school children, farm worker’s children living in tents or children working in cotton fields.” |
In minimally intervention dentistry
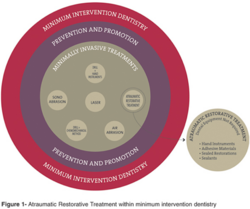
ART is one part of the MID concept and is minimally invasive. It consists of both preventive and restorative components. In ART, the preventive component involves using ART sealants for vulnerable pits and fissures of teeth whereas the restorative treatment part of the MID involves selective removal of the infected dentine using hand instruments while conserving the affected dentine that can be remineralized, preserving as much tooth structure as possible. This is followed by cavity restoration with HVGIC.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Caries excavation : evolution of treating cavitated caries lesions. Basel. 13 September 2018. ISBN 978-3-318-06369-1. OCLC 1028640797.
- ↑ 2.0 2.1 "Managing Carious Lesions: Consensus Recommendations on Carious Tissue Removal". Advances in Dental Research 28 (2): 58–67. May 2016. doi:10.1177/0022034516639271. PMID 27099358. https://discovery.dundee.ac.uk/ws/files/9395094/ICCC_MS_Recommendations_submission_060716_author_accepted_manuscript_version.pdf.
- ↑ 3.0 3.1 3.2 3.3 "Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview". Clinical Oral Investigations 16 (5): 1337–46. October 2012. doi:10.1007/s00784-012-0783-4. PMID 22824915.
- ↑ "Managing Carious Lesions: Consensus Recommendations on Terminology". Advances in Dental Research 28 (2): 49–57. May 2016. doi:10.1177/0022034516639276. PMID 27099357.
- ↑ 5.0 5.1 "Minimal intervention dentistry". Annals of the Royal Australasian College of Dental Surgeons 12: 72–9. April 1994. PMID 7993063.
- ↑ 6.0 6.1 "An atraumatic restorative treatment (ART) technique: evaluation after one year". International Dental Journal 44 (5): 460–4. October 1994. PMID 7814116.
- ↑ 7.0 7.1 7.2 Textbook of preventive and community dentistry.. [Place of publication not identified]: ELSEVIER INDIA. 2011. ISBN 978-81-312-2530-1. OCLC 993695037.
- ↑ "ART restorations and glass ionomer sealants in Zimbabwe: survival after 3 years". Community Dentistry and Oral Epidemiology 26 (6): 372–81. December 1998. doi:10.1111/j.1600-0528.1998.tb01975.x. PMID 9870536.
- ↑ 9.0 9.1 9.2 "The atraumatic restorative treatment (ART) approach for managing dental caries: a meta-analysis". International Dental Journal 56 (6): 345–51. December 2006. doi:10.1111/j.1875-595X.2006.tb00339.x. PMID 17243467.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 "Survival percentages of atraumatic restorative treatment (ART) restorations and sealants in posterior teeth: an updated systematic review and meta-analysis". Clinical Oral Investigations 22 (8): 2703–2725. November 2018. doi:10.1007/s00784-018-2625-5. PMID 30232622.
- ↑ 11.0 11.1 11.2 "The state-of-the-art of ART sealants". Dental Update 41 (2): 119–20, 122-4. March 2014. doi:10.12968/denu.2014.41.2.119. PMID 24783880.
- ↑ "Caries-preventive effect of resin-based and glass ionomer sealants over time: a systematic review". Community Dentistry and Oral Epidemiology 34 (6): 403–9. December 2006. doi:10.1111/j.1600-0528.2006.00321.x. PMID 17092268.
- ↑ "Caries-preventive effect of glass ionomer and resin-based fissure sealants on permanent teeth: a meta analysis". Journal of Oral Science 51 (3): 373–82. September 2009. doi:10.2334/josnusd.51.373. PMID 19776504. http://joi.jlc.jst.go.jp/JST.JSTAGE/josnusd/51.373?from=CrossRef.
- ↑ "Caries-preventive effect of glass ionomer and resin-based fissure sealants on permanent teeth: An update of systematic review evidence". BMC Research Notes 4 (1): 22. January 2011. doi:10.1186/1756-0500-4-22. PMID 21276215.
- ↑ Ahovuo-Saloranta, Anneli; Forss, Helena; Walsh, Tanya; Nordblad, Anne; Mäkelä, Marjukka; Worthington, Helen V. (31 July 2017). "Pit and fissure sealants for preventing dental decay in permanent teeth". The Cochrane Database of Systematic Reviews 7: CD001830. doi:10.1002/14651858.CD001830.pub5. ISSN 1469-493X. PMID 28759120. PMC 6483295. https://www.ncbi.nlm.nih.gov/pubmed/28759120.
- ↑ 16.0 16.1 "Minimal intervention dentistry: part 5. Atraumatic restorative treatment (ART)--a minimum intervention and minimally invasive approach for the management of dental caries". British Dental Journal 214 (1): 11–8. January 2013. doi:10.1038/sj.bdj.2012.1175. PMID 23306489. http://www.nature.com/articles/sj.bdj.2012.1175.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 "Atraumatic restorative treatment (ART): rationale, technique, and development". Journal of Public Health Dentistry 56 (3 Spec No): 135–40; discussion 161-3. September 1996. doi:10.1111/j.1752-7325.1996.tb02423.x. PMID 8915958.
- ↑ 18.0 18.1 18.2 "Pain related to different ways of minimal intervention in the treatment of small caries lesions". ASDC Journal of Dentistry for Children 67 (2): 123–7, 83. 2000. PMID 10826048.
- ↑ 19.0 19.1 "The influence of restorative treatment approaches and the use of local analgesia, on the children's discomfort". European Archives of Paediatric Dentistry 7 (1): 11–6. March 2006. doi:10.1007/BF03320809. PMID 17140522.
- ↑ 20.0 20.1 "Atraumatic restorative treatment versus amalgam restoration longevity: a systematic review". Clinical Oral Investigations 14 (3): 233–40. June 2010. doi:10.1007/s00784-009-0335-8. PMID 19688227.
- ↑ "Failure rate of atraumatic restorative treatment using high-viscosity glass-ionomer cement compared to that of conventional amalgam restorative treatment in primary and permanent teeth: a systematic review update". J Minim Interv Dent 5: 63–124. 2012.
- ↑ "Effectiveness of glass-ionomer (ART) and amalgam restorations in the deciduous dentition: results after 3 years" (in en). Caries Research 36 (6): 437–44. 2002. doi:10.1159/000066531. PMID 12459617. https://www.karger.com/Article/FullText/66531.
- ↑ "Is Atraumatic restorative treatment an option for restoring occlusoproximal caries lesions in primary teeth? A systematic review and meta-analysis". International Journal of Paediatric Dentistry 23 (6): 435–43. November 2013. doi:10.1111/ipd.12013. PMID 23190278.
- ↑ "ART is an alternative for restoring occlusoproximal cavities in primary teeth - evidence from an updated systematic review and meta-analysis". International Journal of Paediatric Dentistry 27 (3): 201–209. May 2017. doi:10.1111/ipd.12252. PMID 27489205.
- ↑ "High-viscosity glass-ionomer cements for direct posterior tooth restorations in permanent teeth: The evidence in brief". Journal of Dentistry 55: 121–123. December 2016. doi:10.1016/j.jdent.2016.10.007. PMID 27765512.
- ↑ "Effectiveness of single-surface ART restorations in the permanent dentition: a meta-analysis". Journal of Dental Research 83 (2): 120–3. February 2004. doi:10.1177/154405910408300207. PMID 14742648.
- ↑ 27.0 27.1 "Micro-invasive interventions for managing proximal dental decay in primary and permanent teeth". The Cochrane Database of Systematic Reviews (11): CD010431. November 2015. doi:10.1002/14651858.CD010431.pub2. PMID 26545080.
- ↑ Fejerskov, Ole; Nyvad, Bente; Kidd, Edwina A M (26 May 2015). Dental caries : the disease and its clinical management (Third ed.). Chichester, West Sussex, UK. ISBN 978-1-118-93582-8. OCLC 897493320.
- ↑ "Introduction--ART from a global perspective". Community Dentistry and Oral Epidemiology 27 (6): 421–2. December 1999. doi:10.1111/j.1600-0528.1999.tb02042.x. PMID 10600075.
- ↑ 30.0 30.1 "Prevention and Management of Caries in Children". https://www.sdcep.org.uk/published-guidance/cariesin-children.
- ↑ "Selection of restorative materials for the atraumatic restorative treatment (ART) approach: a review". Special Care in Dentistry 21 (6): 216–21. November 2001. doi:10.1111/j.1754-4505.2001.tb00257.x. PMID 11885670.
- ↑ "Alliance for a Cavity-Free Future". 2010. p. 1–5. https://www.acffglobal.org/.
- ↑ "A review of atraumatic restorative treatment (ART)". International Dental Journal 49 (3): 127–31. June 1999. doi:10.1002/j.1875-595X.1999.tb00896.x. PMID 10858744.
- ↑ "Atraumatic restorative treatment and dental anxiety in outpatients attending public oral health clinics in South Africa". Journal of Public Health Dentistry 67 (3): 179–84. June 2007. doi:10.1111/j.1752-7325.2007.00017.x. PMID 17899905.
- ↑ 35.0 35.1 "Atraumatic perspectives of ART: psychological and physiological aspects of treatment with and without rotary instruments". Community Dentistry and Oral Epidemiology 31 (1): 15–20. February 2003. doi:10.1034/j.1600-0528.2003.00021.x. PMID 12542428.
- ↑ "Atraumatic dental treatment among Finnish elderly persons". Journal of Oral Rehabilitation 29 (5): 435–40. May 2002. doi:10.1046/j.1365-2842.2002.00903.x. PMID 12028490.
- ↑ "ART for treating root caries in older people". Evidence-Based Dentistry 8 (2): 51. June 2007. doi:10.1038/sj.ebd.6400497. PMID 17589492. http://www.nature.com/articles/6400497.
- ↑ "One year survival of ART and conventional restorations in patients with disability". BMC Oral Health 14 (1): 49. May 2014. doi:10.1186/1472-6831-14-49. PMID 24885938.
- ↑ "Glass ionomer cements used as fissure sealants with the atraumatic restorative treatment (ART) approach: review of literature". International Dental Journal 52 (2): 67–70. April 2002. doi:10.1111/j.1875-595X.2002.tb00602.x. PMID 12013252.
- ↑ "Cost-effectiveness analysis of the atraumatic restorative treatment-based approach to managing early childhood caries". Community Dentistry and Oral Epidemiology 45 (1): 92–100. February 2017. doi:10.1111/cdoe.12265. PMID 27859533.
- ↑ "Dental anxiety and pain related to ART". Journal of Applied Oral Science 17 (special issue): 84–8. 2009. doi:10.1590/S1678-77572009000700015. PMID 21499661.
- ↑ "Self-report of pain in children treated according to the atraumatic restorative treatment and the conventional restorative treatment--a pilot study". The Journal of Clinical Pediatric Dentistry 34 (2): 151–5. December 2009. doi:10.17796/jcpd.34.2.9k67p786l7126263. PMID 20297707.
- ↑ "How effective is ART in the management of dental caries?". Community Dentistry and Oral Epidemiology 27 (6): 423–30. December 1999. doi:10.1111/j.1600-0528.1999.tb02043.x. PMID 10600076.
- ↑ "Atraumatic restorative treatment (ART): a three-year community field trial in Thailand--survival of one-surface restorations in the permanent dentition". Journal of Public Health Dentistry 56 (3 Spec No): 141–5; discussion 161-3. September 1996. doi:10.1111/j.1752-7325.1996.tb02424.x. PMID 8915959.
- ↑ "Acceptance and discomfort from atraumatic restorative treatment in secondary school students in Egypt". Medical Principles and Practice 18 (1): 26–30. 2009. doi:10.1159/000163042. PMID 19060487. https://www.karger.com/Article/FullText/163042.
- ↑ "Restoration of permanent teeth in young rural children in Cambodia using the atraumatic restorative treatment (ART) technique and Fuji II glass ionomer cement". International Journal of Paediatric Dentistry 8 (1): 35–40. March 1998. doi:10.1046/j.1365-263X.1998.00058.x. PMID 9558544.
- ↑ 47.0 47.1 "Efficiency of different polyacrylic acid concentrations on the smear layer, after ART technique, by Scanning Electron Microscopy (SEM)". European Archives of Paediatric Dentistry 11 (5): 232–5. October 2010. doi:10.1007/BF03262753. PMID 20932397.
- ↑ "Caries Removal by Chemomechanical (Carisolv™) vs. Rotary Drill: A Systematic Review". The Open Dentistry Journal 9 (1): 462–72. 2015-12-31. doi:10.2174/1874210601509010462. PMID 26962375.
- ↑ "Comparison of Carisolv system vs traditional rotating instruments for caries removal in the primary dentition: A systematic review and meta-analysis". Acta Odontologica Scandinavica 73 (8): 569–80. 2015-11-17. doi:10.3109/00016357.2015.1023353. PMID 25772193.
- ↑ "Systematic Review and Meta-Analysis of Randomized Clinical Trials on Chemomechanical Caries Removal". Operative Dentistry 40 (4): E167-78. 2015-06-01. doi:10.2341/14-021-LIT. PMID 26167737. https://meridian.allenpress.com/operative-dentistry/article/40/4/E167/194357/Systematic-Review-and-MetaAnalysis-of-Randomized.
- ↑ "How to make choice of the carious removal methods, Carisolv or traditional drilling? A meta-analysis". Journal of Oral Rehabilitation 41 (6): 432–42. June 2014. doi:10.1111/joor.12161. PMID 24661083.
- ↑ "Efficacy of using Carisolv in the removal of decayed tooth structure in primary teeth". Evidence-Based Dentistry 17 (2): 44–5. June 2016. doi:10.1038/sj.ebd.6401167. PMID 27339236. http://www.nature.com/articles/6401167.
- ↑ "Effects of Papacarie on children with dental caries in primary teeth: a systematic review and meta-analysis". International Journal of Paediatric Dentistry 28 (4): 361–372. July 2018. doi:10.1111/ipd.12364. PMID 29682851.
- ↑ "Papain gel: a new chemo-mechanical caries removal agent". The Journal of Clinical Pediatric Dentistry 30 (2): 115–9. January 2006. doi:10.17796/jcpd.30.2.xq641w720u101048. PMID 16491964.
- ↑ "Clinical and radiographic study of chemical-mechanical removal of caries using Papacárie: 24-month follow up". The Journal of Clinical Pediatric Dentistry 35 (3): 251–4. April 2011. doi:10.17796/jcpd.35.3.75803m02524625h5. PMID 21678665.
- ↑ "Brazil - Atraumatic Restorative Treatment for a disadvantaged Brazilian Community". https://capp.mau.se/bank-of-ideas/brazil-atraumatic-restorative-treatment-for-a-disadvantaged-brazilian-community/.
- ↑ "South Africa - An Atraumatic Restorative Treatment (ART) Project: Activity Report". https://capp.mau.se/bank-of-ideas/south-africa-an-atraumatic-restorative-treatment-art-project-activity-report/.
- ↑ "Sri Lanka - ART Training Programme for School Dental Therapists, Jaffna". https://capp.mau.se/bank-of-ideas/sri-lanka-art-training-programme-for-school-dental-therapists-jaffna/.
- ↑ "Sri Lanka - An ongoing school-based ART Programme". https://capp.mau.se/bank-of-ideas/sri-lanka-an-ongoing-school-based-art-programme/.
- ↑ "Turkey - Ongoing Atraumatic Restorative Treatment (ART) Programme in some rural areas". https://capp.mau.se/bank-of-ideas/turkey-ongoing-atraumatic-restorative-treatment-art-programme-in-some-rural-areas/.
- ↑ "The correct use of the ART approach". Journal of Applied Oral Science 18 (1): 1–4. February 2010. doi:10.1590/S1678-77572010000100002. PMID 20379674.

