Medicine:Chalazion
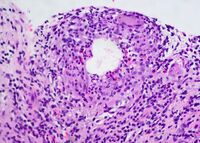
A chalazion (/kəˈleɪziən/; plural chalazia or chalazions) or meibomian cyst[1] is not a cyst but a granuloma[2] in the eyelid that results from a blocked meibomian gland.[3][4] It typically occurs in the middle of the eyelid, is red, and is not painful.[5] They tend to develop gradually over a few weeks.[5]
A chalazion may occur following a stye or from hardened oils blocking the gland.[5] The blocked gland is usually the meibomian gland, but can also be the gland of Zeis.[6]
A stye and cellulitis may appear similar.[5] A stye, however, is usually more sudden in onset, painful, and occurs at the edge of the eyelid.[5] Cellulitis is also typically painful.[5]
Treatment is initiated with warm compresses.[5] In addition, antibiotic/corticosteroid eyedrops or ointment may be used. If this is not effective, injecting corticosteroids into the lesion may be tried.[5] If the granuloma is large, incision and drainage may be recommended.[5] While relatively common, the frequency of the condition is unknown.[7] It is most common in people 30–50 years of age, and equally common in males and females.[8] The term is from grc χαλάζιον (khalazion) 'small hailstone'.[9]
Signs and symptoms

- Painless swelling on the eyelid
- Eyelid tenderness typically none-to-mild
- Increased tearing
- Heaviness of the eyelid
- Redness of conjunctiva
Complications
A large chalazion can cause astigmatism due to pressure on the cornea.[10]
As laser eye surgery involves shaping the cornea by burning parts of it away, weakening its structure, post-operation people can be left predisposed to deformation of the cornea from small chalazia.[11]
Complications of corticosteroid injection include hypopigmentation and fat atrophy which is less likely to occur in conjunctival approach of injection.[1]
Diagnosis
A chalazion or meibomian cyst can sometimes be mistaken for a stye.
Differential diagnosis
- Sebaceous gland adenoma
- Sebaceous gland carcinoma
- Sarcoid granuloma
- Foreign body granuloma
Treatment

General treatment
Chalazia will often disappear without further treatment within a few months, and virtually all will resorb within two years.[12]
Healing can be facilitated by applying a moist warm compress to the affected eye for approximately 10–15 minutes, 4 times per day.[13][14] This promotes opening, drainage, and healing by softening the hardened oil that is occluding the duct.[14][15] In addition, it is helpful to scrub the lid margin (at the base of the eyelashes) with a washcloth and mild (baby) shampoo, which removes oily debris.[16][17][18]
Topical antibiotic eye drops or ointment (e.g., chloramphenicol or fusidic acid) are sometimes used for the initial acute infection, but are otherwise of little value in treating a chalazion.[19]
If they continue to enlarge or fail to settle within a few months, smaller lesions can be injected with a corticosteroid.
Larger ones can be surgically removed using local anesthesia.[20][21] This is usually done from underneath the eyelid to avoid a scar on the skin. If the chalazion is located directly under the eyelid's outer tissue, however, an excision from above may be more advisable so as not to inflict any unnecessary damage on the lid itself. Eyelid epidermis usually mends well, without leaving any visible scar.[22] Depending on the chalazion's texture, the excision procedure varies: while fluid matter can easily be removed under minimal invasion, by merely puncturing the chalazion and exerting pressure upon the surrounding tissue, hardened matter usually necessitates a larger incision, through which it can be scraped out. Any residual matter should be metabolized in the course of the subsequent healing process, generally aided by regular appliance of dry heat. The excision of larger chalazia may result in visible hematoma around the lid, which will wear off within three or four days, whereas the swelling may persist for longer. Chalazion excision is an ambulant treatment and normally does not take longer than fifteen minutes. Nevertheless, owing to the risks of infection and severe damage to the eyelid, such procedures should only be performed by a medical professional.
Chalazia may recur, and they will usually be biopsied to rule out the possibility of a tumour.[1]
Antibiotic/corticosteroid eyedrops or ointment
A limited course of topical antibiotic/corticosteroid combination eyedrops or ointment such as tobramycin/dexamethasone may be effective in treating a chalazion.[23][24][25]
Surgery

Chalazion surgery is a simple procedure that is generally performed as a day operation, and the person does not need to remain in the hospital for further medical care. The eyelid is injected with a local anesthetic, a clamp is put on the eyelid, then the eyelid is turned over, an incision is made on the inside of the eyelid, and the chalazion is drained and scraped out with a curette. A scar on the upper lid can cause discomfort as some people feel the scar as they blink. As surgery damages healthy tissue (e.g., by scarring tissue or possibly even causing blepharitis), given other options, less invasive treatment is preferable.[26]
Chalazion removal surgery is performed under local or general anesthesia. Commonly, general anesthesia is administered in children to make sure they stay still and no injury to the eye occurs. Local anesthesia is used in adults and it is applied with a small injection into the eyelid. The discomfort of the injection is minimized with the help of an anesthetic cream, which is applied locally.
The chalazion can be removed in two ways, depending on the size of cyst. Relatively small chalazia are removed through a small cut at the back of the eyelid.[27] The surgeon lifts the eyelid to access the back of its surface and makes an incision of approximately 3mm just on top of the chalazion. The lump is then removed, and pressure is applied for a few minutes to stop any oozing of blood that may occur because of the operation.[28] Surgery of small chalazia does not require stitches, as the cut is at the back of the eyelid and therefore the cut cannot be seen, and the cosmetic result is excellent.
Larger chalazia are removed through an incision in front of the eyelid. Larger chalazia usually push on the skin of the eyelid, and this is the main reason why doctors prefer removing them this way. The incision is not usually larger than 3mm and it is made on top of the chalazion. The lump is removed and then pressure is applied to the incision to prevent oozing. This type of surgery is closed with very fine stitches. They are hardly visible and are usually removed within a week after the surgery has been performed. Although chalazia are rarely dangerous, it is common to send the chalazion or part of it to a laboratory to screen for cancer.[12]
In rare cases, people are kept overnight in the hospital after chalazion surgery. This includes cases in which complications occurred and the person needs to be closely monitored. In most cases, however, people are able to go home after the operation has ended.
Chalazion surgery is a safe procedure and complications seldom occur. Serious complications that require another operation are also very rare. Among potential complications, there are infection, bleeding, or the recurrence of the chalazion.
Steroid injection
Because the inflammatory cells of chalazia are sensitive to steroids, intralesional or subcutaneous injection of soluble steroids, commonly 0.1 to 0.2 ml of triamcinolone acetonide (TA) into the lesion's center one or two times, is one option.[29][30] The success rate is in the 77% to 93% range.[30] It carries a quite small risk of central retinal artery obstruction, focal depigmentation in dark-skinned patients, and inadvertent ocular penetration.[29] It is considered a simple and effective treatment option, one with high success rates.[31] It may give the same results as surgical treatment (I&C).[1] Larger, long-standing lesions are best treated surgically.[29] Considering the surgical risks, steroid injection is believed to be a safer procedure in marginal lesions and lesions close to lacrimal punctum.[1]
One injection alone has a success rate of about 80%; if requested, a second injection can be given 1–2 weeks later.[1]
Carbon dioxide laser
Chalazion excision using a CO2 laser is also a safer procedure, with minimal bleeding and no eye patching required.[32]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 John F, Salmon. "Eyelids". Kanski's Clinical ophthalmology (9 ed.). Elsevier. pp. 39–41.
- ↑ Sihota, Ramanjit; Tandon, Radhika (2020). Parsons' Diseases of the Eye (23rd ed.). Elsevier. ISBN 978-81-312-5415-8.
- ↑ "Eyelid Disorders Chalazion & Stye". National Eye Institute. 4 May 2010. https://nei.nih.gov/faqs/eyelid-disorders-chalazion-stye.
- ↑ Korn, Bobby S. (2021). 2021-2022 Basic and Clinical Science Course, Section 07: Oculofacial Plastic and Orbital Surgery. American Academy of Ophthalmology. pp. 181. ISBN 978-1681044453.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Carlisle, RT; Digiovanni, J (15 July 2015). "Differential Diagnosis of the Swollen Red Eyelid". American Family Physician 92 (2): 106–12. PMID 26176369.
- ↑ Deibel, JP; Cowling, K (May 2013). "Ocular inflammation and infection". Emergency Medicine Clinics of North America 31 (2): 387–97. doi:10.1016/j.emc.2013.01.006. PMID 23601478.
- ↑ Rutter, Paul Professor; Newby, David (2013). Community Pharmacy ANZ: Symptoms, Diagnosis and Treatment (3 ed.). Elsevier Health Sciences. p. 57. ISBN 9780729583459. https://books.google.com/books?id=NbjVCgAAQBAJ&pg=PA57.
- ↑ Ferri's Clinical Advisor 2021 E-Book: 5 Books in 1. Elsevier Health Sciences. 10 June 2020. ISBN 9780323713344. https://books.google.com/books?id=FubqDwAAQBAJ&pg=PA338-IA6.
- ↑ "chalazion (n.)". http://www.etymonline.com/index.php?term=chalazion.
- ↑ Jin, Ki Won; Shin, Young Joo; Hyon, Joon Young (2017-03-31). "Effects of chalazia on corneal astigmatism". BMC Ophthalmology 17 (1): 36. doi:10.1186/s12886-017-0426-2. ISSN 1471-2415. PMID 28359272.
- ↑ "Medical Definition of Laser surgery". MedicineNet. https://www.medicinenet.com/script/main/art.asp?articlekey=31889.
- ↑ 12.0 12.1 "Chalazion". GPnotebook. https://www.gpnotebook.co.uk/simplepage.cfm?ID=2080768019.
- ↑ Adult-Gerontology Practice Guidelines. Springer. 2019. ISBN 9780826195197. https://books.google.com/books?id=O15xDwAAQBAJ&pg=PA142.
- ↑ 14.0 14.1 Advanced Practice Nursing in the Care of Older Adults. F.A. Davis. 31 October 2018. ISBN 9780803694798. https://books.google.com/books?id=nd11DwAAQBAJ&pg=PA138.
- ↑ "Chalazion". http://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/chalazion.
- ↑ First Aid for the Emergency Medicine Boards Third Edition. McGraw Hill Professional. 2016. ISBN 9780071843676. https://books.google.com/books?id=6QYEDAAAQBAJ&q=chalazion+compress+minutes.
- ↑ Clinical Eye Atlas. Oxford University Press. 2010. ISBN 9780195342178. https://books.google.com/books?id=qDd_IiblCiUC&pg=PA22.
- ↑ Pfenninger and Fowler's Procedures for Primary Care E-Book: Expert Consult. Elsevier Health Sciences. 2010. ISBN 9781455700929. https://books.google.com/books?id=loI3ZhC4UN4C&pg=PA427. Retrieved 2023-03-18.
- ↑ "Chalazion". https://www.webmd.com/eye-health/chalazion-what-is.
- ↑ "Chalazion therapy. Intralesional steroids versus incision and curettage". Acta Ophthalmol (Copenh) 66 (3): 352–354. 1988. doi:10.1111/j.1755-3768.1988.tb04609.x. PMID 10994460.
- ↑ "A prospective study of cost, patient satisfaction, and outcome of treatment of chalazion by medical and nursing staff". Br J Ophthalmol 84 (7): 782–785. 2000. doi:10.1136/bjo.84.7.782. PMID 10873994. – in which of those cases attending a District General Hospital, approximately one third of selected chalazia resolved within 3 months with conservative treatment, and surgical treatment was successful for 72%.
- ↑ "Gerstenkorn/Hagelkorn | Auge Online". https://www.auge-online.de/Erkrankungen/Liderkrankungen/Gerstenkorn_Hagelkorn.
- ↑ Pediatric Ophthalmology, an Issue of Pediatric Clinics. Elsevier Health Sciences. 2014. ISBN 9780323299466. https://books.google.com/books?id=Ihu7AwAAQBAJ&pg=PA599. Retrieved 2023-03-18.
- ↑ Pfenninger and Fowler's Procedures for Primary Care E-Book. Elsevier Health Sciences. 24 March 2019. ISBN 9780323567954. https://books.google.com/books?id=uZKODwAAQBAJ&pg=PA367. Retrieved 18 March 2023.
- ↑ Wu, Albert Y.; Gervasio, Kalla A.; Gergoudis, Kellie N.; Wei, Chen; Oestreicher, James H.; Harvey, John T. (June 25, 2018). "Conservative therapy for chalazia: is it really effective?". Acta Ophthalmologica 96 (4): e503–e509. doi:10.1111/aos.13675. PMID 29338124.
- ↑ "Chalazion". 27 October 2020. https://www.lecturio.com/concepts/chalazion/.
- ↑ "Removal of chalazion". 2009-07-06. http://www.netdoctor.co.uk/surgical-procedures/removal-of-chalazion.htm.
- ↑ "The operation". 2009-07-06. http://www.netdoctor.co.uk/surgical-procedures/removal-of-chalazion.htm.
- ↑ 29.0 29.1 29.2 Diagnostic Atlas of Common Eyelid Diseases. CRC Press. 2007. ISBN 9781420016321. https://books.google.com/books?id=JbY6Syu9QZEC&pg=PA135. Retrieved 2023-03-18.
- ↑ 30.0 30.1 Clinical Ocular Pharmacology. Elsevier Health Sciences. 2007. ISBN 9780750675765. https://books.google.com/books?id=Eybg7fbs65MC&pg=PA390. Retrieved 2023-03-18.
- ↑ Kashinath Choudhary; Vinod Bhagwat; Manish Shyamkul; Akshay Sathe; Naser Razvi. "Non-Operative Management of Chalazion: Experiences at Tertiary Health Care Centre". Walawalkar International Medical Journal. http://www.wimjournal.com/html/journal/images/5a1.pdf. Retrieved 2020-06-01.
- ↑ Korn EL (1988-06-01). "Laser chalazion removal". Ophthalmic Surgery 19 (6): 428–431. PMID 3419780.
External links
| Classification | |
|---|---|
| External resources |
 |
