Medicine:Hematidrosis
| Hematidrosis | |
|---|---|
| Other names | Hematohidrosis, haematidrosis, hemidrosis, blood sweat |
 | |
| Red-tinted sweat (or "blood sweat") caused by hematohidrosis | |
| Specialty | Dermatology |
Hematidrosis, also called hematohidrosis, haematidrosis, hemidrosis and blood sweat, is a very rare condition in which a human sweats blood.[1] The term is from Ancient Greek haîma/haímatos (αἷμα/αἵματος), meaning blood, and hīdrṓs (ἱδρώς), meaning sweat.
Signs and symptoms
Blood usually oozes from the forehead, nails, umbilicus, and other skin surfaces. In addition, oozing from mucocutaneous surfaces causing nosebleeds, bloodstained tears, and vicarious menstruation are common.[2] The episodes may be preceded by intense headache and abdominal pain and are usually self-limiting. In some conditions, the secreted fluid is more dilute and appears to be blood-tinged, while others may have darker, bright red secretions resembling blood.[3]
While the extent of blood loss generally is minimal, hematidrosis also results in the skin becoming extremely tender and fragile.
Causes
Hematidrosis is a condition in which capillary blood vessels that feed the sweat glands rupture, causing them to exude blood, occurring under conditions of extreme physical or emotional stress.[4] Severe mental anxiety activates the sympathetic nervous system to invoke the fight-or-flight response to such a degree as to cause hemorrhage of the vessels supplying the sweat glands.[5] It has been suggested that acute fear and extreme stress can cause hematidrosis.[6]
Diagnosis
Investigation such as platelets count, platelet aggregation test, coagulation profile, and skin biopsy reveal no abnormalities and direct light microscopy of fluid demonstrates presence of normal red blood cells. Investigations also fail to show any vasculitis or skin appendages (i.e. sweat glands, sebaceous glands and hair follicles) abnormalities.[3][7]
A 2015 case study investigated hematidrosis with a patient who has epilepsy.[8]
Treatment
Effect on the body is weakness and mild to moderate dehydration from the severe anxiety and both blood and sweat loss.[9]
The condition is very rare, but there are reports in medical literature of successful treatment with beta blockers (propranolol 10 mg)[10][11] with significant reduction in the frequency of spontaneous blood oozing. The successful use of beta blockers supports the theory that the condition is induced by stress and anxiety; however, this etiology is not fully established yet as the high prevalence of stress and anxiety in the modern era did not change the incidence of this extremely rare disease, suggesting that other co-abnormalities also play a key role in this disease.[7] Atropine sulfate transdermal patches have also been used successfully.[3]
Favorable results with psychiatric counselling to reduce stress highlight the relationship between psychogenic causes and hematohidrosis.[5]
Instances
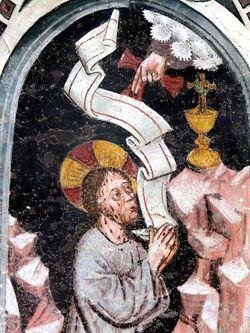
Dermatological research notes the presence of hematidrosis in people awaiting execution.[5] It has also been proposed as a possible explanation for Jesus' agony in the garden of Gethsemane (Luke 22:44)[12] and for claims associated with stigmata.[13][14]
Leonardo da Vinci described a soldier who sweated blood before battle. The phenomenon has also been observed in individuals in fear for their lives; a case occurred during the London blitz, and a case of fear of a storm while sailing, etc.[13]
See also
- Haemolacria – blood in tears
- Hyperhidrosis
References
- ↑ Tshifularo, M. (2014). "Blood otorrhea: blood stained sweaty ear discharges: hematohidrosis; four case series (2001-2013).". American Journal of Otolaryngology 35 (2): 271–3. doi:10.1016/j.amjoto.2013.09.006. PMID 24315735. http://repository.up.ac.za/bitstream/2263/42202/1/Tshifularo_Blood_2014.pdf.
- ↑ Holoubek, J. E.; Holoubek, A. B. (1996). "Blood, sweat and fear. "A classification of hematidrosis"". Journal of Medicine 27 (3–4): 115–33. PMID 8982961.
- ↑ 3.0 3.1 3.2 Biswas, S.; Surana, T.; De, A.; Nag, F. (2013). "A curious case of sweating blood". Indian Journal of Dermatology 58 (6): 478–80. doi:10.4103/0019-5154.119964. PMID 24249903.
- ↑ Freddrick Z., Dr "Hematidrosis"
- ↑ 5.0 5.1 5.2 Jerajani, H. R.; Jaju, Bhagyashri; Phiske, M. M.; Lade, Nitin (2009). "Hematohidrosis – A rare clinical phenomenon". Indian Journal of Dermatology 54 (3): 290–2. doi:10.4103/0019-5154.55645. PMID 20161867.
- ↑ Holoubek JE; Holoubek AB (1996). "Blood, Sweat and Fear: A Classification of Hematidrosis". Journal of Medicine 27 (3–4): 115–133. PMID 8982961.
- ↑ 7.0 7.1 Mora, E; Lucas, J (2013). "Hematidrosis: Blood sweat". Blood 121 (9): 1493. doi:10.1182/blood-2012-09-450031. PMID 23570065.
- ↑ Shen H., Wang Z., Wu T., Wang J., Ren C., Chen H., Yu Z., Don W. (2015). "Haematidrosis associated with epilepsy in a girl successfully Treated with oxcarbazepine: Case report". Journal of International Medical 43 (2): 263–69. doi:10.1177/0300060514562488. PMID 25673645.
- ↑ Zhang FK, Zheng YL, Liu JH, Chen HS, Liu SH, Xu MQ (2004). "Clinical and laboratory study of a case of hematidrosis". Zhonghua Xue Ye Xue Za Zhi 25 (3): 147–50. PMID 15182582.
- ↑ Wang, Z.; Yu, Z.; Su, J.; Cao, L.; Zhao, X.; Bai, X.; Zhan, S.; Wu, T. et al. (2010). "A Case of Hematidrosis Successfully Treated with Propranolol". American Journal of Clinical Dermatology 11 (6): 440–43. doi:10.2165/11531690-000000000-00000. PMID 20666570.
- ↑ Khalid, S. R.; Maqbool, S; Raza, N; Mukhtar, T; Ikram, A; Qureshi, S (2013). "Ghost spell or hematohidrosis". Journal of the College of Physicians and Surgeons (JCPSP) 23 (4): 293–94. PMID 23552544.
- ↑ William D. Edwards; Wesley J. Gabel; Floyd E. Hosmer (March 21, 1986). "On the Physical Death of Jesus Christ". JAMA 255 (11): 1455–1463. doi:10.1001/jama.1986.03370110077025. PMID 3512867. http://hilbornbiblehistory.cmswiki.wikispaces.net/file/view/JAMA+article+The+Crucifixion+of+Jesus+Christ.pdf.
- ↑ 13.0 13.1 Manonukul J, Wisuthsarewong W, Chantorn R, Vongirad A, Omeapinyan P. (2008). Hematidrosis: A pathologic process or stigmata. A case report with comprehensive histopathologic and immunoperoxidase studies. Am J Dermatopathol 30: 135-139.
- ↑ Kluger, N; Cribier, B. (2013). Stigmata: From Saint-Francis of Assisi to Idiopathic Haematidrosis. Ann Dermatol Venereol 140: 771-777.
 |