Medicine:Vaginal dilator


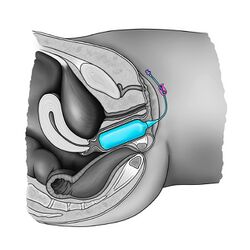
A vaginal dilator, sometimes called a vaginal trainer, vaginal stent or vaginal expander,[1] is an instrument used to gently stretch the vagina. They are used when the vagina has become narrowed (vaginal stenosis), such as after brachytherapy for gynecologic cancers,[2], as therapy for vaginismus and other forms of dyspareunia,[3] and to maintain the neovaginal canal following gender-affirming surgery.[4]
There is evidence for dilator use across many different diagnoses with fair to good results.[5] This includes following cancer treatments and for vaginal agenesis conditions. The evidence presents varying approaches and protocols.
Vaginal dilators, can be solid or inflatable and are commonly used during surgeries.[6][7][8] Vaginal stents are routinely used in surgery and postoperative care for transgender women who are undergoing gender-affirming vaginoplasty to form a neovagina.[8][4][9][10] The vaginal expander is used immediately after surgery to keep the passage from collapsing, and regularly thereafter to maintain the viability of the neovagina. Frequency of use requirements decrease over time, but remains obligatory lifelong.[11][12]
Use
With solid vaginal dilators, the patient starts with the smallest dilator size, then gradually increasing until the largest dilator size is reached. This practice can be accompanied by breathing exercises in order to relax the pelvic floor muscles. Dilation acts should not cause pain or bleeding.[13] Dilatation with rigid dilators must be done carefully as vaginal perforation and urethral injury may occur.[14][15] There is no consensus on the frequency and duration of using vaginal dilators.[16] In case of vaginal expanders, the therapist or the patient introduces the deflated balloon into the vagina and then inflates it gently until the required diameter is obtained.[10]
Following gender-affirming vaginoplasty, patients may be required to use vaginal dilators multiple times daily to maintain the depth and length of the neovagina. Different size dilators may be used, typically starting with a smaller diameter and increasing the size over the course of several weeks post-surgery. Over time the frequency of dilation can be reduced to daily and eventually to every few days as instructed by surgeons.[8][4][9]
Image gallery

In popular culture
Vaginal dilators appear in the comedy feature film Lady Parts, as the main character struggles with vaginismus after receiving a vestibulectomy.[17]
See also
- Dilator (medical instrument)
- Dildo
- Rectal dilator
- Vaginoplasty
References
- ↑ "Vaginismus". National Health Service. 11 January 2018. http://www.nhs.uk/Conditions/Vaginismus/Pages/Treatment.aspx.
- ↑ Miles, Tracie; Johnson, Neal (2014). "Vaginal dilator therapy for women receiving pelvic radiotherapy". Cochrane Database Syst Rev 9 (9). doi:10.1002/14651858.CD007291.pub3. PMID 25198150.
- ↑ Idama, T. O.; Pring, D. W. (2000). "Vaginal dilator therapy-an outpatient gynaecological option in the management of dyspareunia". Journal of Obstetrics and Gynaecology 20 (3): 303–05. doi:10.1080/01443610050009683. PMID 15512559.
- ↑ 4.0 4.1 4.2 Bene, Nicholas C.; Ferrin, Peter C.; Xu, Jing; Dy, Geolani W.; Dugi, Daniel; Peters, Blair R. (8 May 2024). "Tissue Options for Construction of the Neovaginal Canal in Gender-Affirming Vaginoplasty" (in en). Journal of Clinical Medicine 13 (10): 2760. doi:10.3390/jcm13102760. ISSN 2077-0383. PMID 38792302.
- ↑ Olson, Amanda. "Frequently Asked Questions - Vaginal Dilators FAQ". https://www.intimaterose.com/pages/frequently-asked-questions-vaginal-dilators/.
- ↑ Coskun, Ayhan; Coban, Yusuf Kenan; Vardar, Mehmet Ali; Dalay, Ahmet Cemil (10 July 2007). "The use of a silicone-coated acrylic vaginal stent in McIndoe vaginoplasty and review of the literature concerning silicone-based vaginal stents: a case report". BMC Surgery 7 (1): 13. doi:10.1186/1471-2482-7-13. PMID 17623058.
- ↑ Barutçu, Ali; Akgüner, Muharrem (November 1998). "McIndoe Vaginoplasty with the Inflatable Vaginal Stent". Annals of Plastic Surgery 41 (5): 568–569. doi:10.1097/00000637-199811000-00020. PMID 9827964.
- ↑ 8.0 8.1 8.2 Dy, Geolani W.; Jun, Min Suk; Blasdel, Gaines; Bluebond-Langner, Rachel; Zhao, Lee C. (1 May 2021). "Outcomes of Gender Affirming Peritoneal Flap Vaginoplasty Using the Da Vinci Single Port Versus Xi Robotic Systems". European Urology 79 (5): 676–683. doi:10.1016/j.eururo.2020.06.040. ISSN 0302-2838. PMID 32624272. https://www.sciencedirect.com/science/article/abs/pii/S0302283820304693. Retrieved 31 August 2025.
- ↑ 9.0 9.1 Liang, Fan; Cohen, Andrew. "Vaginoplasty for Gender Affirmation" (in en). https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/vaginoplasty-for-gender-affirmation.
- ↑ 10.0 10.1 Antoniadis, N; Charles, G; Mejías, I; Pabón, R (March 2011). "Vaginoplastia: modificación de la técnica de McIndoe usando esponja de gel hemostático". Cirugía Plástica Ibero-Latinoamericana 37 (1): 73–77. doi:10.4321/S0376-78922011000100010. http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0376-78922011000100010.
- ↑ Rinzler, Carol Ann (12 May 2010). The Encyclopedia of Cosmetic and Plastic Surgery. Facts on File library of health and living.. New York: Infobase Publishing. p. 195. ISBN 978-1-4381-2702-6. OCLC 223107099. https://books.google.com/books?id=N5nWmFCbYqcC&pg=PA195. Retrieved 31 May 2018.
- ↑ Georgiade, Gregory S.; Georgiade, Nicholas G. (1992). Textbook of plastic, maxillofacial, and reconstructive surgery. Baltimore, Maryland: Williams & Wilkins. ISBN 978-0-683-03454-7. OCLC 455225627. https://books.google.com/books?id=snJsAAAAMAAJ. Retrieved 31 May 2018.
- ↑ Psychosexual Team, Oxfordshire Sexual Health Service. "Vaginal Dilator Exercises for Psychosexual Therapy". Oxford University Hospitals NHS Foundation Trust. https://www.ouh.nhs.uk/patient-guide/leaflets/files/30804Pexercises.pdf.
- ↑ HOFFMAN, M (May 2003). "Risks of rigid dilation for a radiated vaginal cuff: two related rectovaginal fistulas". Obstetrics & Gynecology 101 (5): 1125–1126. doi:10.1016/s0029-7844(02)02624-8. PMID 12738124.
- ↑ Lue, Kathy; Heinsimer, Kevin; Madiraju, SriGita K.; Rideout, Drew; Wiegand, Lucas (January 2020). "Urologic trauma from vaginal dilation for congenital vaginal stenosis: A newly-described and challenging complication". Urology Case Reports 28. doi:10.1016/j.eucr.2019.101075. PMID 31788430.
- ↑ Liu, Marisa; Juravic, Mark; Mazza, Genevieve; Krychman, Michael L. (January 2020). "Vaginal Dilators: Issues and Answers". Sexual Medicine Reviews 9 (2): 212–220. doi:10.1016/j.sxmr.2019.11.005. PMID 32014450.
- ↑ "Lady Parts Film Trailer" (in en). https://www.intimaterose.com/pages/lady-parts-film-trailer.
 |
