Organization:Safe to Sleep
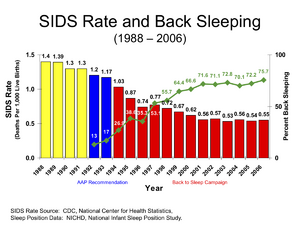
The Safe to Sleep campaign, formerly known as the Back to Sleep campaign,[1] is an initiative backed by the US National Institute of Child Health and Human Development (NICHD) at the US National Institutes of Health to encourage parents to have their infants sleep on their backs (supine position) to reduce the risk of sudden infant death syndrome, or SIDS. The target age group of the campaign is 0–1 years of age, because this is when babies are at the greatest risk of experiencing SIDS.[2] Since "Safe to Sleep" was launched in 1994, the incidence of SIDS has declined by more than 50%.[2] However, there has been a rise in infant sleep-related suffocation events. Consequently, the campaign has broadened its goal to focus on safe sleep conditions and further preventative measures.
The campaign was successful in significantly reducing the percentage of babies sleeping on their stomachs (prone position). It was found, however, that a significant portion of African-American babies were still sleeping on their stomachs; in 1999, an African-American baby was 2.2 times more likely to die of SIDS than a white baby. Thus, then Secretary of Health and Human Services Donna Shalala and Tipper Gore refocused the "Back to Sleep" campaign on minority babies.[2]
History
In 1992, the American Academy of Pediatrics (AAP) recommended[lower-alpha 1] that babies sleep on their backs or sides to reduce the risk of SIDS (a revised statement in 1996 retracted the side-sleeping option). NICHD launched the "Back to Sleep" campaign in 1994 to spread the message.[2]
The campaign was successful in significantly reducing the percentage of babies sleeping on their stomachs (prone position). It was found, however, that a significant portion of African-American babies were still sleeping on their stomachs; in 1999, an African-American baby was 2.2 times more likely to die of SIDS than a white baby. Thus, then Secretary of Health and Human Services Donna Shalala and Tipper Gore refocused the "Back to Sleep" campaign on minority babies.[2]
Campaign
In 1985 Davies reported that in Hong Kong, where the common Chinese habit was for supine infant sleep position (face up), SIDS was a rare problem.[4] In 1987 the Netherlands started a campaign advising parents to place their newborn infants to sleep on their backs (supine position) instead of their stomachs (prone position).[5] This was followed by infant supine sleep position campaigns in the United Kingdom (as "Back to Sleep"),[6] New Zealand, and Australia in 1991, the U.S. and Sweden in 1992, and Canada in 1993.[5][7]
This advice was based on the epidemiology of SIDS and physiological evidence which showed that infants who sleep on their back have lower arousal thresholds and less slow-wave sleep (SWS) compared to infants who sleep on their stomachs.[8] Thus, these infants are more easily awakened. However, the arousal thresholds have been shown to be higher during SWS causing infants to be less easily awakened.[8]
In human infants, sleep develops rapidly during early development. This development includes an increase in non-rapid eye movement (NREM) sleep – which is also called quiet sleep (QS) – during the first 12 months of life, in association with a decrease in rapid eye movement (REM) sleep – which is also known as active sleep (AS).[9][10][11] In addition, slow wave sleep (SWS) – which consists of stage 3 and stage 4 NREM sleep – appears at 2 months of age,[12][13][14][15] and it is theorized that some infants have a brain-stem defect which increases their risk of being unable to arouse from SWS (also called deep sleep) and therefore have an increased risk of SIDS due to their decreased ability to arouse from SWS.[8]
Studies have shown that preterm infants,[16][17] full-term infants,[18][19] and older infants[20] have greater time periods of quiet sleep and also decreased time awake when they are positioned to sleep on their stomachs, meaning these babies are harder to wake when sleeping on their tummy. In both human infants and rats, arousal thresholds have been shown to be at higher levels in the electroencephalography (EEG) during slow-wave sleep.[21][22][23]
In 1992,[24] a SIDS risk reduction strategy based upon lowering arousal thresholds during SWS was implemented by the American Academy of Pediatrics (AAP) which began recommending that healthy infants be positioned to sleep on their back (supine position) or side (lateral position) instead of their stomach (prone position) when being placed down for sleep. In 1994,[25] a number of organizations in the United States combined to further communicate these non-prone sleep position recommendations and this became formally known as the "Back To Sleep" campaign. In 1996,[26] the AAP further refined its sleep position recommendation by stating that infants should only be placed to sleep in the supine position and not in the prone or lateral positions.
Since the launch of the campaign, the incidence of SIDS has declined by more than half. However, 3,400 babies (ages 0–1) still die per year from SIDS and sleep-related suffocation events despite the implementation of this campaign.[27] The AAP and further research has shown that there are preventative measures that can be taken to control environmental factors to prevent such adverse events.[28]
SIDS risk factors
Risk factors for SIDS can be divided into three major categories: maternal, infant, and environmental factors.[28] The factors mentioned below are modifiable and preventable to help decrease the occurrence of SIDS and sleep-related suffocation events.
| Maternal factors | Infant factors | Environmental factors |
|---|---|---|
|
|
|
Preventive measures
Several precautions focused on controlling environmental factors can be taken to minimize the risk of SIDS and sleep-related suffocation events.[2][28][30][31] Per the safe to sleep campaign, these preventive measures can be taken to decrease the rate of SIDS and sleep-related suffocation events:[2]
- Sleeping on back[30]
- Sleeping on a firm/hard surface [30]
- Nothing in the crib or bassinet other than the baby[30]
- No stuffed toys, loose blankets and/or crib bumpers[30]
- Room sharing[28]
- It is important to note this is different from sharing a bed with an infant. This entails sleeping in the same room as one's baby but making sure the baby has a safe sleeping space free of the aforementioned risk factors.
- Use of a pacifier while the baby is sleeping[30]
- The concept behind the use of a pacifier during sleep is that these babies do not sleep as deeply and might be more easily arousable; thus, they are less likely to have an adverse sleep-related event.
- Tummy time[2]
- Regular tummy time helps to strengthen babies' core, neck, and shoulder muscles. These muscle groups are essential in helping babies to turn their head and bodies to avoid suffocating during sleep.
- Avoiding sleep in a car seat outside of the car[28]
- A car seat is only safe to sleep in while in the car.
- Avoiding sleep in an inclined chair (e.g., Rock 'n Play Sleeper, rocking swings, etc.) without constant supervision[28]
- Breastfeeding[31]
- Regular prenatal care[31]
- No smoking during pregnancy[31]
- Avoid secondhand smoke exposure[31]
- Up-to-date immunizations[31]
See also
- Sudden infant death syndrome
- Tummy time
- Plagiocephaly
- United States Department of Health and Human Services
Footnotes
References
- ↑ Safe to Sleep Public Education Campaign
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 "Safe to Sleep". https://safetosleep.nichd.nih.gov/campaign/history.
- ↑ "Microbiology in sudden infant death syndrome (SIDS) and other childhood deaths". FEMS Immunol Med Microbiol 25 (1–2): 59–66. August 1, 1999. doi:10.1111/j.1574-695X.1999.tb01327.x. PMID 10443492. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1574-695X.1999.tb01327.x.
- ↑ Davies DP (December 1985). "Cot death in Hong Kong: a rare problem?". Lancet 2 (8468): 1346–9. doi:10.1016/S0140-6736(85)92637-6. PMID 2866397.
- ↑ 5.0 5.1 Högberg U; Bergström E (April 2000). "Suffocated prone: the iatrogenic tragedy of SIDS". Am J Public Health 90 (4): 527–31. doi:10.2105/AJPH.90.4.527. PMID 10754964.
- ↑ Perkins, Anne (26 August 2016). "Back to sleep: the doctor who helped stem a cot death epidemic". The Guardian. https://www.theguardian.com/society/2016/aug/26/back-to-sleep-sudden-infant-death-syndrome-cot-death-peter-fleming.
- ↑ Rusen ID; Liu S; Sauve R; Joseph KS; Kramer MS (2004). "Sudden infant death syndrome in Canada: trends in rates and risk factors, 1985–1998". Chronic Dis Can 25 (1): 1–6. PMID 15298482.
- ↑ 8.0 8.1 8.2 Kattwinkel J, Hauck F.R., Moon R.Y., Malloy M and Willinger M (2006). "Infant Death Syndrome: In Reply, Bed Sharing With Unimpaired Parents Is Not an Important Risk for Sudden". Pediatrics 117 (3): 994–996. doi:10.1542/peds.2005-2994.
- ↑ Louis J; Cannard C; Bastuji H; Challamel MJ (May 1997). "Sleep ontogenesis revisited: a longitudinal 24-hour home polygraphic study on 15 normal infants during the first two years of life". Sleep 20 (5): 323–33. doi:10.1093/sleep/20.5.323. PMID 9381053.
- ↑ Navelet Y; Benoit O; Bouard G (July 1982). "Nocturnal sleep organization during the first months of life". Electroencephalogr Clin Neurophysiol 54 (1): 71–8. doi:10.1016/0013-4694(82)90233-4. PMID 6177520.
- ↑ Roffwarg HP; Muzio JN; Dement WC (April 1966). "Ontogenetic Development of the Human Sleep-Dream Cycle". Science 152 (3722): 604–619. doi:10.1126/science.152.3722.604. PMID 17779492. Bibcode: 1966Sci...152..604R.
- ↑ Anders TF; Keener M (1985). "Developmental course of nighttime sleep-wake patterns in full-term and premature infants during the first year of life. I". Sleep 8 (3): 173–92. doi:10.1093/sleep/8.3.173. PMID 4048734.
- ↑ Bes F; Schulz H; Navelet Y; Salzarulo P (February 1991). "The distribution of slow-wave sleep across the night: a comparison for infants, children, and adults". Sleep 14 (1): 5–12. doi:10.1093/sleep/14.1.5. PMID 1811320.
- ↑ Coons S; Guilleminault C (June 1982). "Development of sleep-wake patterns and non-rapid eye movement sleep stages during the first six months of life in normal infants". Pediatrics 69 (6): 793–8. doi:10.1542/peds.69.6.793. PMID 7079046.
- ↑ Fagioli I; Salzarulo P (April 1982). "Sleep states development in the first year of life assessed through 24-h recordings". Early Hum. Dev. 6 (2): 215–28. doi:10.1016/0378-3782(82)90109-8. PMID 7094858.
- ↑ "Effects of sleeping position and time after feeding on the organization of sleep/wake states in prematurely born infants". Sleep 21 (4): 343–9. June 1998. PMID 9646378.
- ↑ "Quality of diet, body position, and time after feeding influence behavioral states in low birth weight infants". Pediatr. Res. 52 (3): 399–404. September 2002. doi:10.1203/00006450-200209000-00016. PMID 12193675.
- ↑ Brackbill Y; Douthitt TC; West H (January 1973). "Psychophysiologic effects in the neonate of prone versus supine placement". J. Pediatr. 82 (1): 82–4. doi:10.1016/S0022-3476(73)80017-4. PMID 4681872.
- ↑ Amemiya F; Vos JE; Prechtl HF (May 1991). "Effects of prone and supine position on heart rate, respiratory rate and motor activity in fullterm newborn infants". Brain Dev. 13 (3): 148–54. doi:10.1016/S0387-7604(12)80020-9. PMID 1928606.
- ↑ Kahn A; Rebuffat E; Sottiaux M; Dufour D; Cadranel S; Reiterer F (February 1991). "Arousals induced by proximal esophageal reflux in infants". Sleep 14 (1): 39–42. PMID 1811318.
- ↑ Ashton R (April 1973). "The influence of state and prandial condition upon the reactivity of the newborn to auditory stimulation". J Exp Child Psychol 15 (2): 315–27. doi:10.1016/0022-0965(73)90152-5. PMID 4735894.
- ↑ Rechtschaffen A; Hauri P; Zeitlin M (June 1966). "Auditory awakening thresholds in REM and NREM sleep stages". Perceptual and Motor Skills 22 (3): 927–42. doi:10.2466/pms.1966.22.3.927. PMID 5963124.
- ↑ Neckelmann D; Ursin R (August 1993). "Sleep stages and EEG power spectrum in relation to acoustical stimulus arousal threshold in the rat". Sleep 16 (5): 467–77. PMID 8378687.
- ↑ "American Academy of Pediatrics AAP Task Force on Infant Positioning and SIDS: Positioning and SIDS". Pediatrics 89 (6 Pt 1): 1120–6. June 1992. doi:10.1542/peds.89.6.1120. PMID 1503575.
- ↑ U.S. Department of Human Services. "BACK TO SLEEP" CAMPAIGN SEEKS To Reduce Inicidence of SIDS In African American Populations PressRelease. [1] Tuesday, October 26, 1999
- ↑ "Positioning and sudden infant death syndrome (SIDS): update. American Academy of Pediatrics Task Force on Infant Positioning and SIDS". Pediatrics 98 (6 Pt 1): 1216–8. December 1996. doi:10.1542/peds.98.6.1216. PMID 8951285.
- ↑ "CDC SIDS". 7 September 2022. http://www.cdc.gov/sids/.
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 TASK FORCE ON SUDDEN INFANT DEATH SYNDROME (2016-10-24). "SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment". Pediatrics 138 (5): e20162938. doi:10.1542/peds.2016-2938. ISSN 0031-4005. PMID 27940804.
- ↑ Bigger, Harold R.; Silvestri, Jean M.; Shott, Susan; Weese-Mayer, Debra E. (July 1998). "Influence of increased survival in very low birth weight, low birth weight, and normal birth weight infants on the incidence of sudden infant death syndrome in the United States: 1985-1991". The Journal of Pediatrics 133 (1): 73–78. doi:10.1016/s0022-3476(98)70181-7. ISSN 0022-3476. PMID 9672514. http://dx.doi.org/10.1016/s0022-3476(98)70181-7.
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 TASK FORCE ON SUDDEN INFANT DEATH SYNDROME (2016-10-24). "SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment". Pediatrics 138 (5): e20162938. doi:10.1542/peds.2016-2938. ISSN 0031-4005. PMID 27940804.
- ↑ 31.0 31.1 31.2 31.3 31.4 31.5 Hauck, Fern R.; Thompson, John M. D.; Tanabe, Kawai O.; Moon, Rachel Y.; Vennemann, Mechtild M. (2011-07-01). "Breastfeeding and Reduced Risk of Sudden Infant Death Syndrome: A Meta-analysis". Pediatrics 128 (1): 103–110. doi:10.1542/peds.2010-3000. ISSN 0031-4005. PMID 21669892. http://dx.doi.org/10.1542/peds.2010-3000.
External links
 |
