Medicine:Pulp capping
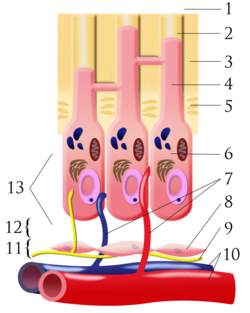
Pulp capping is a technique used in dental restorations to prevent the dental pulp from necrosis, after being exposed, or nearly exposed during a cavity preparation, from a traumatic injury, or by a deep cavity that reaches the center of the tooth causing the pulp to die. When dental caries is removed from a tooth, all or most of the infected and softened enamel and dentin are removed. This can lead to the pulp of the tooth either being exposed or nearly exposed which causes pulpitis (inflammation). Pulpitis, in turn, can become irreversible, leading to pain and pulp necrosis, and necessitating either root canal treatment or extraction.[1] The ultimate goal of pulp capping or stepwise caries removal is to protect a healthy dental pulp and avoid the need for root canal therapy.
To prevent the pulp from deteriorating when a dental restoration gets near the pulp, the dentist will place a small amount of a sedative dressing, such as calcium hydroxide or MTA. These materials, protect the pulp from noxious agents (heat, cold, bacteria) and stimulate the cell-rich zone of the pulp to lay down a bridge of reparative dentin. Dentin formation usually starts within 30 days of the pulp capping (there can be a delay in onset of dentin formation if the odontoblasts of the pulp are injured during cavity removal) and is largely completed by 130 days.[2]:491–494
Two different types of pulp cap are distinguished. In direct pulp capping, the protective dressing is placed directly over an exposed pulp; and in indirect pulp capping, a thin layer of softened dentin, that if removed would expose the pulp, is left in place and the protective dressing is placed on top.[3] A direct pulp cap is a one-stage procedure, whereas a stepwise caries removal is a two-stage procedure over about six months.
Direct
This technique is used when a pulpal exposure occurs, either due to caries extending to the pulp chamber, or accidentally, during caries removal. It is only feasible if the exposure is made through non infected dentin and there is no recent history of spontaneous pain (i.e. irreversible pulpitis) and a bacteria-tight seal can be applied.[3] Once the exposure is made, the tooth is isolated from saliva to prevent contamination by use of a dental dam, if it was not already in place. The tooth is then washed and dried, and the protective material placed, followed finally by a dental restoration which gives a bacteria-tight seal to prevent infection. Since pulp capping is not always successful in maintaining the vitality of the pulp, the dentist will usually keep the status of the tooth under review for about 1 year after the procedure.[3]
Indication for Direct Pulp Capping
Indication for Direct Pulp Capping:[4]
- Immature/mature permanent teeth with simple restoration needs
- Recent trauma less than 24 hours (less according to tichy) exposure of pulp / mechanical trauma exposure (during restorative procedure)
- Minimal or no bleeding at exposure site
- Normal sensibility test
- Not tender to percussion
- No periradicular pathology
- Young patient
Contraindication for Direct Pulp Capping
Contraindication for Direct Pulp Capping:[4]
- Systemic disease involvement
- Primary teeth
- Inflammatory signs and symptoms
- Pre-operative tooth sensitivity
- Large pulpal exposure
- Uncontrollable bleeding from the pulp
- Non-restorable tooth
- Elderly patient
Indirect
In 1938, Bodecker introduced the Stepwise Caries Excavation (SWE) Technique for treatment of teeth with deep caries for preservation of Pulp vitality.[5] This technique is used when most of the decay has been removed from a deep cavity, but some softened dentin and decay remains over the pulp chamber that if removed would expose the pulp and trigger irreversible pulpitis. Instead, the dentist intentionally leaves the softened dentin/decay in place, and uses a layer of protective temporary material which promotes remineralization of the softened dentin over the pulp and the laying down of new layers of tertiary dentin in the pulp chamber. The color of the carious lesion changes from light brown to dark brown, the consistency goes from soft and wet to hard and dry so that Streptococcus Mutans and Lactobacilli have been significantly reduced to a limited number or even zero viable organisms and the radiographs show no change or even a decrease in the radiolucent zone.[6] A temporary filling is used to keep the material in place, and about 6 months later, the cavity is re-opened and hopefully there is now enough sound dentin over the pulp (a "dentin bridge") that any residual softened dentin can be removed and a permanent filling can be placed. This method is also called "stepwise caries removal."[3][7] The difficulty with this technique is estimating how rapid the carious process has been, how much tertiary dentine has been formed and knowing exactly when to stop excavating to avoid pulp exposure.[8]
Materials
The following materials have been studied as potential materials for direct pulp capping. However, calcium hydroxide and mineral trioxide aggregate (MTA) are the preferred material of choice in clinical practice due to their favourable outcome.
Zinc oxide eugenol
Zinc Oxide Eugenol (ZOE) is a commonly used material in dentistry. The use of ZOE as a pulp capping material remains controversial. This is due to Eugenol, being cytotoxic to the pulp are present in large quantity in this formulation. Also due to its nature of non-adhesive, it leads to poor coronal seal hence increases micro-leakage. Studies have demonstrated unfavourable results for ZOE when compared to calcium hydroxide as a direct pulp capping material as it causes pulpal necrosis.[9]
Glass and resin modified glass ionomer
Both Glass Ionomer (GI) and Resin Modified Glass Ionomer (RMGIC) has been widely used as a lining or base material for deep cavities where pulp is in close proximity. This is due to its superior properties of good biocompatibility and adhesive nature, providing coronal seal to prevent bacteria infiltration. However, they are not a material of choice for direct pulp capping. When the use of RMGIC and calcium hydroxide has been studied as direct pulp capping agents, RMGIC has demonstrated increase in chronic inflammation in pulpal tissues and lack of reparative dentine bridge formation.[9]
Adhesive system
Materials that fall under this category include 4-META-MMA-TBB adhesives and hybridizing dentine bonding agents. The idea of using adhesive materials for direct pulp capping has been explored two decades ago. Studies have demonstrated that it encourages bleeding due to its vasodilating properties hence impairing polymerisation of the material, affecting its ability to provide a coronal seal when used as a pulp capping agent. In addition, the material triggers chronic inflammation even without the presence of bacteria makes it an unfavourable condition for pulp healing to take place. Most importantly, its toxicity to human pulp cells once again makes it an unacceptable material of choice.[9]
Calcium hydroxide cement
Calcium hydroxide (CaOH) is an organo-metallic cement that was introduced into dentistry in the early twentieth century[10] and there have since been many advantages to this material described in much of the available literature. CaOH has a high antimicrobial activity which has been shown to be outstanding.[11][12] In one experiment conducted by Stuart et al. (1991), bacteria-inoculated root canals of extracted human teeth were treated with CaOH for 1 hour against a control group with no treatment and the results yielded 64-100% reductions in all viable bacteria.[11] CaOH also has a high pH and high solubility, thus it readily leaches into the surrounding tissues.[13] This alkaline environment created around the cement has been suggested to give beneficial irritancy to pulpal tissues and stimulates dentine regeneration. One study further demonstrated that CaOH causes release of growth factors TGF-B1 and bioactive molecules from the dentine matrix which induces the formation of dentine bridges.[14]
CaOH does however have significant disadvantages. The set cement has low compressive strength and cannot withstand or support condensation of a restoration.[13][15] It is thus good practice to place a stronger separate lining material (e.g. glass ionomer or resin-modified glass ionomer) over CaOH before packing the final restorative material.[9] CaOH cement is not adhesive to tooth tissues and thus does not provide a coronal seal.[9] In pulp perfusion studies, CaOH has shown to insufficiently seal all dentinal tubules, and presence of tunnel defects (patent communications within reparative dentine connecting pulp and exposure sites) indicate a potential for microleakage when CaOH is used.[13][16] It is suggested that an adhesive coronal restoration be used above the CaOH lining to provide adequate coronal seal. Because of its many advantageous properties and long-standing success in clinical use, it has been used as a control material in multiple experiments with pulp capping agents over the years[17][18] and is considered the gold standard dental material for direct pulp capping to date.[19]
Mineral trioxide aggregate
Mineral trioxide aggregate (MTA) is a recent development of the 1990s[20] initially as a root canal sealer but has seen increased interest in its use as a direct pulp capping material.[9] The material comprises a blend of tricalcium silicate, dicalcium silicate and tricalcium aluminate; bismuth oxide is added to give the cement radiopaque properties to aid radiological investigation.[20] MTA has been shown to produce CaOH as a hydration product[21] and maintains an extended duration of high pH in lab conditions.[22] Similar to CaOH, this alkalinity potentially provides beneficial irritancy and stimulates dentine repair and regeneration.[23] MTA has also demonstrated reliable and favourable healing outcomes on human teeth when used as a pulp cap on teeth diagnosed as nothing more severe than reversible pulpitis.[24] There is also less coronal microleakage of MTA in one experiment comparing it to amalgam[25] thus suggesting some tooth adhesion properties. MTA also comes in white and grey preparations[26] which may aid visual identification clinically. Disadvantages have also been described for MTA. Grey MTA preparations can potentially cause tooth discolouration.[9] MTA also takes a long time (up to 2 hours 45 minutes) to set completely[27] thus preventing immediate restoration placement without mechanical disruption of the underlying MTA. It has been suggested that a pulp capped with MTA should be temporised to allow for the complete setting of MTA,[9] and the patient to present at a second visit for placement of the permanent restoration.[24] MTA also has for difficult handling properties and is a very expensive material, thus is less cost effective as compared to CaOH.[9]
Although MTA shows great promise which is possibly attributed to its adhesive properties and ability to act as a source of CaOH release,[9] the available literature and experimental studies of MTA is limited due to its recency. Studies that compare pulp capping abilities of MTA to CaOH in human teeth yielded generally equal and similarly successful healing outcomes at a histological level from both materials.[28][29]
Success rates
There have been several studies conducted on the success rates of direct and indirect pulp capping using a range of different materials. One study of indirect pulp capping recorded success rates of 98.3% and 95% using bioactive tricalcium silicate [Ca3SiO5]-based dentin substitute and light-activated calcium hydroxide [CA(OH)2]-based liner respectively.[30] These results show no significant difference, nor do the results from an indirect pulp capping experiment comparing calcium silicate cement (Biodentine) and glass ionomer cement, which had clinical success rates of 83.3%.[31] A further study testing medical Portland cement, Mineral Trioxide Aggregate (MTA) and calcium hydroxide in indirect pulp treatment found varying success rates of 73%-93%. This study concluded that indirect pulp capping had a success rate of 90.3% regardless of which material was used but stated that it is preferable to use non-resorbing materials where possible.[32]
Similar studies have been conducted of direct pulp capping, with one study comparing ProRoot Mineral Trioxide Aggregate (MTA) and Biodentine which found success rates of 92.6% and 96.4% respectively.[33] This study was conducted on 6-18 year old patients, while a comparable study conducted on mature permanent teeth found success rates of 84.6% using MTA and 92.3% using Biodentine.[34] Calcium hydroxide has also been tested on its use in indirect pulp capping and was found to have a success rate of 77.6%, compared to a success rate of 85.9% for MTA in another study.[35]
A systematic review attempted to compare success rates of direct pulp capping and indirect pulp capping and found that indirect pulp capping had a higher level of success but found a low quality of evidence in studies on direct pulp capping.[36] More research will be needed to provide a comprehensive answer.
See also
References
- ↑ "Vital Pulp Capping: A Worthwhile Procedure (review)". J Can Dent Assoc 65 (6): 328–31. 1999. PMID 10412240. http://www.cda-adc.ca/jcda/vol-65/issue-6/328.html.
- ↑ Cohen's Pathways of the Pulp (Tenth ed.). St. Louis, Missouri: Mosby Elsevier. 2011. ISBN 978-0-323-06489-7.
- ↑ 3.0 3.1 3.2 3.3 European Society of Endodontology (December 2006). "Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology". International Endodontic Journal 39 (12): 921–30. doi:10.1111/j.1365-2591.2006.01180.x. PMID 17180780.
- ↑ 4.0 4.1 Fuks, A.; Peretz, B. (2016). Pediatric Endodontics Current Concepts in Pulp Therapy for Primary and Young Permanent Teeth. SpringerLink.
- ↑ Banava, Sepideh (2011). "Stepwise Excavation: A Conservative Community-Based Dental Treatment of Deep Caries to Inhibit Pulpal Exposure". Iran J Public Health 40 (3): 140. PMID 23113097.
- ↑ Hilton, Thomas J (2009). "Keys to Clinical Success with Pulp Capping: A Review of the Literature". Operative Dentistry 34 (5): 615–625. doi:10.2341/09-132-0. PMID 19830978.
- ↑ "Incomplete caries removal: a systematic review and meta-analysis". Journal of Dental Research 92 (4): 306–14. April 2013. doi:10.1177/0022034513477425. PMID 23396521.
- ↑ David Ricketts, David (2001). "Restorative dentistry: Management of the deep carious lesion and the vital pulp dentine complex". British Dental Journal 191 (11): 606–610. doi:10.1038/sj.bdj.4801246. PMID 11770946.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 9.9 "Keys to clinical success with pulp capping: a review of the literature". Operative Dentistry 34 (5): 615–25. 2009. doi:10.2341/09-132-0. PMID 19830978.
- ↑ "Review of calcium hydroxide" (in en). International Endodontic Journal 23 (6): 283–97. November 1990. doi:10.1111/j.1365-2591.1990.tb00108.x. PMID 2098345.
- ↑ 11.0 11.1 "The comparative antimicrobial effect of calcium hydroxide". Oral Surgery, Oral Medicine, and Oral Pathology 72 (1): 101–4. July 1991. doi:10.1016/0030-4220(91)90198-l. PMID 1891227.
- ↑ "TNF-alpha release in monocytes after exposure to calcium hydroxide treated Escherichia coli LPS". International Endodontic Journal 30 (3): 155–9. May 1997. doi:10.1046/j.1365-2591.1997.00066.x. PMID 9477798.
- ↑ 13.0 13.1 13.2 McCabe, John F.; Walls, Angus W. G. (2008). "29". Applied Dental Materials. Blackwell Publishing Ltd.. pp. 281–282. ISBN 9781405139618. https://archive.org/details/applieddentalmat00mcca.
- ↑ "The effect of calcium hydroxide on solubilisation of bio-active dentine matrix components". Biomaterials 27 (14): 2865–73. May 2006. doi:10.1016/j.biomaterials.2005.12.020. PMID 16427123.
- ↑ "Calcium hydroxide liners: a literature review". Clinical, Cosmetic and Investigational Dentistry 9: 67–72. 2017-07-13. doi:10.2147/CCIDE.S141381. PMID 28761378.
- ↑ "Tunnel defects in dentin bridges: their formation following direct pulp capping". Operative Dentistry 21 (1): 4–11. January 1996. PMID 8957909.
- ↑ "Response of human pulps capped with different self-etch adhesive systems". Clinical Oral Investigations 12 (2): 119–27. June 2008. doi:10.1007/s00784-007-0161-9. PMID 18027004.
- ↑ "Response of human pulps capped with a self-etching adhesive system". Dental Materials 17 (3): 230–40. May 2001. doi:10.1016/s0109-5641(00)00076-2. PMID 11257296.
- ↑ Dean, Jeffrey A. (September 2015). "Chapter 13 – Treatment of Deep Caries, Vital Pulp Exposure, and Pulpless Teeth". McDonald and Avery's Dentistry for the Child and Adolescent (Tenth ed.). pp. 221–242. doi:10.1016/B978-0-323-28745-6.00013-2. ISBN 978-0-323-28745-6.
- ↑ 20.0 20.1 "Mineral trioxide aggregate: a review of the constituents and biological properties of the material" (in en). International Endodontic Journal 39 (10): 747–54. October 2006. doi:10.1111/j.1365-2591.2006.01135.x. PMID 16948659.
- ↑ "Characterization of hydration products of mineral trioxide aggregate". International Endodontic Journal 41 (5): 408–17. May 2008. doi:10.1111/j.1365-2591.2007.01370.x. PMID 18298574.
- ↑ "MTA solubility: a long term study". Journal of Endodontics 31 (5): 376–9. May 2005. doi:10.1097/01.don.0000140566.97319.3e. PMID 15851933.
- ↑ "Dissolution of bio-active dentine matrix components by mineral trioxide aggregate". Journal of Dentistry 35 (8): 636–42. August 2007. doi:10.1016/j.jdent.2007.04.008. PMID 17566626.
- ↑ 24.0 24.1 "Direct pulp capping with mineral trioxide aggregate: an observational study". Journal of the American Dental Association 139 (3): 305–15; quiz 305–15. March 2008. doi:10.14219/jada.archive.2008.0160. PMID 18310735.
- ↑ "Coronal microleakage of two root-end filling materials using a polymicrobial marker". Journal of Endodontics 34 (2): 201–3. February 2008. doi:10.1016/j.joen.2007.09.019. PMID 18215682.
- ↑ "Chemical analysis of powder and set forms of Portland cement, gray ProRoot MTA, white ProRoot MTA, and gray MTA-Angelus". Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 102 (6): 809–15. December 2006. doi:10.1016/j.tripleo.2005.11.034. PMID 17138186.
- ↑ "Physical and chemical properties of a new root-end filling material". Journal of Endodontics 21 (7): 349–53. July 1995. doi:10.1016/S0099-2399(06)80967-2. PMID 7499973.
- ↑ "Evaluation of mineral trioxide aggregate and calcium hydroxide cement as pulp-capping agents in human teeth". Journal of Endodontics 34 (1): 1–6. January 2008. doi:10.1016/j.joen.2007.09.012. PMID 18155482.
- ↑ "Histological evaluation of mineral trioxide aggregate and calcium hydroxide in direct pulp capping of human immature permanent teeth". American Journal of Dentistry 21 (4): 262–6. August 2008. PMID 18795524.
- ↑ "Bioactive Tricalcium Silicate-based Dentin Substitute as an Indirect Pulp Capping Material for Primary Teeth: A 12-month Follow-up". Pediatric Dentistry 39 (5): 377–382. September 2017. PMID 29070160.
- ↑ "Clinical and radiographic assessment of the efficacy of calcium silicate indirect pulp capping: a randomized controlled clinical trial". Journal of Dental Research 94 (4): 562–8. April 2015. doi:10.1177/0022034515571415. PMID 25710953.
- ↑ "A randomized clinical trial on the use of medical Portland cement, MTA and calcium hydroxide in indirect pulp treatment". Clinical Oral Investigations 18 (5): 1383–9. 2014. doi:10.1007/s00784-013-1107-z. PMID 24043482.
- ↑ "Outcomes of Direct Pulp Capping by Using Either ProRoot Mineral Trioxide Aggregate or Biodentine in Permanent Teeth with Carious Pulp Exposure in 6- to 18-Year-Old Patients: A Randomized Controlled Trial". Journal of Endodontics 44 (3): 341–348. December 2017. doi:10.1016/j.joen.2017.10.012. PMID 29275850.
- ↑ "Treatment Outcome Following Direct Pulp Capping Using Bioceramic Materials in Mature Permanent Teeth with Carious Exposure: A Pilot Retrospective Study". Journal of Endodontics 43 (10): 1635–1639. October 2017. doi:10.1016/j.joen.2017.06.017. PMID 28807371.
- ↑ "Prognostic factors in direct pulp capping with mineral trioxide aggregate or calcium hydroxide: 2- to 6-year follow-up". Clinical Oral Investigations 21 (1): 357–367. January 2017. doi:10.1007/s00784-016-1798-z. PMID 27041110.
- ↑ "Primary Tooth Vital Pulp Therapy: A Systematic Review and Meta-analysis". Pediatric Dentistry 39 (1): 16–123. January 2017. PMID 28292337.
 |