Medicine:Electrocardiography in myocardial infarction
| Electrocardiography in myocardial infarction | |
|---|---|
| Medical diagnostics | |
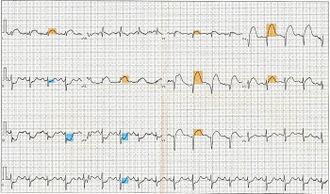 12-lead electrocardiogram showing ST-segment elevation (orange) in I, aVL and V1-V5 with reciprocal changes (blue) in the inferior leads, indicative of an anterior wall myocardial infarction. | |
| Purpose | detecting ischemia or acute coronary injury in emergency department |
Electrocardiography in suspected myocardial infarction has the main purpose of detecting ischemia or acute coronary injury in emergency department populations coming for symptoms of myocardial infarction (MI). Also, it can distinguish clinically different types of myocardial infarction.
Technical issues
The standard 12 lead electrocardiogram (ECG) has several limitations. An ECG represents a brief sample in time. Because unstable ischemic syndromes have rapidly changing supply versus demand characteristics, a single ECG may not accurately represent the entire picture.[1] It is therefore desirable to obtain serial 12 lead ECGs, particularly if the first ECG is obtained during a pain-free episode. Alternatively, many emergency departments and chest pain centers use computers capable of continuous ST segment monitoring.[2] The standard 12 lead ECG also does not directly examine the right ventricle, and is relatively poor at examining the posterior basal and lateral walls of the left ventricle. In particular, acute myocardial infarction in the distribution of the circumflex artery is likely to produce a nondiagnostic ECG.[1] The use of additional ECG leads like right-sided leads V3R and V4R and posterior leads V7, V8, and V9 may improve sensitivity for right ventricular and posterior myocardial infarction. In spite of these limitations, the 12 lead ECG stands at the center of risk stratification for the patient with suspected acute myocardial infarction. Mistakes in interpretation are relatively common, and the failure to identify high risk features has a negative effect on the quality of patient care.[3]
Main patterns
The 12 lead ECG is used to classify MI patients into one of three groups:[4]
- those with ST segment elevation or new bundle branch block (suspicious for acute injury and a possible candidate for acute reperfusion therapy with thrombolytics or primary PCI),
- those with ST segment depression or T wave inversion (suspicious for ischemia), and
- those with a so-called non-diagnostic or normal ECG. However, a normal ECG does not rule out acute myocardial infarction.
ST elevation MI
The 2018 European Society of Cardiology/American College of Cardiology Foundation/American Heart Association/World Health Federation Universal Definition of Myocardial Infarction for the ECG diagnosis of the ST segment elevation type of acute myocardial infarction require new ST elevation at J point of at least 1mm (0.1 mV) in two contiguous leads with the cut-points: ≥1 mm in all leads other than leads V2-V3. For leads V2-V3: ≥2 mm in men ≥40 years, ≥2.5 mm in men <40 years, or ≥1.5 mm in women regardless of age. This assumes usual calibration of 1mV/10mm.[5] These elevations must be present in anatomically contiguous leads.[4] (I, aVL, V5, V6 correspond to the lateral wall; V3-V4 correspond to the anterior wall ; V1-V2 correspond to the septal wall; II, III, aVF correspond to the inferior wall.) This criterion is problematic, however, as acute myocardial infarction is not the most common cause of ST segment elevation in chest pain patients.[6] Over 90% of healthy men have at least 1 mm (0.1 mV) of ST segment elevation in at least one precordial lead.[7] The clinician must therefore be well versed in recognizing the so-called ECG mimics of acute myocardial infarction, which include left ventricular hypertrophy, left bundle branch block, paced rhythm, early repolarization, pericarditis, hyperkalemia, and ventricular aneurysm.[7][8][9]
There are heavily researched clinical decision tools such as the TIMI Scores which help prognose and diagnose STEMI based on clinical data. For example, TIMI scores are frequently used to take advantage of EKG findings to prognose patients with MI symptoms.[10] Based on symptoms and electrocardiographic findings, practitioners can differentiate between unstable angina, NSTEMI and STEMI, normally in the emergency room setting.[11] Other calculators such as the GRACE[12] and HEART [13] scores, assess other major cardiac events using electrocardiogram findings, both predicting mortality rates for 6 months and 6 weeks, respectively.[citation needed]
Typical progression
Sometimes the earliest presentation of acute myocardial infarction is the hyperacute T wave, which is treated the same as ST segment elevation.[14] In practice this is rarely seen, because it only exists for 2–30 minutes after the onset of infarction.[15] Hyperacute T waves need to be distinguished from the peaked T waves associated with hyperkalemia.[16]
In the first few hours the ST segments usually begin to rise.[17] Pathological Q waves may appear within hours or may take greater than 24 hr.[17] The T wave will generally become inverted in the first 24 hours, as the ST elevation begins to resolve.[17]
Long term changes of ECG include persistent Q waves (in 90% of cases) and persistent inverted T waves.[17] Persistent ST elevation is rare except in the presence of a ventricular aneurysm.[17]
See also
References
- ↑ 1.0 1.1 Cannon CP at al. Management of Acute Coronary Syndromes. p. 175. New Jersey: Humana Press, 1999. ISBN:0-89603-552-2.
- ↑ "An evaluation of technologies for identifying acute cardiac ischemia in the emergency department: executive summary of a National Heart Attack Alert Program Working Group Report". Ann Emerg Med 29 (1): 1–12. January 1997. doi:10.1016/S0196-0644(97)70297-X. PMID 8998085.
- ↑ "Implications of the failure to identify high-risk electrocardiogram findings for the quality of care of patients with acute myocardial infarction: results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study". Circulation 114 (15): 1565–71. October 2006. doi:10.1161/CIRCULATIONAHA.106.623652. PMID 17015790.
- ↑ 4.0 4.1 Ecc Committee, Subcommittees Task Forces of the American Heart Association (2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care — Part 8: Stabilization of the Patient With .......Acute Coronary Syndromes". Circulation 112 (24_suppl): IV–89–IV–110. doi:10.1161/CIRCULATIONAHA.105.166561. PMID 16314375. http://circ.ahajournals.org/cgi/content/full/112/24_suppl/IV-89.
- ↑ Thygesen, Kristian; Alpert, Joseph S.; Jaffe, Allan S.; Chaitman, Bernard R.; Bax, Jeroen J.; Morrow, David A.; White, Harvey D. (October 2018). "Fourth Universal Definition of Myocardial Infarction (2018)". Journal of the American College of Cardiology 72 (18): 2252. doi:10.1016/j.jacc.2018.08.1038. PMID 30153967. http://www.onlinejacc.org/content/72/18/2231.
- ↑ "Cause of ST segment abnormality in ED chest pain patients". Am J Emerg Med 19 (1): 25–8. January 2001. doi:10.1053/ajem.2001.18029. PMID 11146012.
- ↑ 7.0 7.1 "ST-segment elevation in conditions other than acute myocardial infarction". N. Engl. J. Med. 349 (22): 2128–35. November 2003. doi:10.1056/NEJMra022580. PMID 14645641.
- ↑ "Electrocardiographic manifestations: patterns that confound the EKG diagnosis of acute myocardial infarction-left bundle branch block, ventricular paced rhythm, and left ventricular hypertrophy". J Emerg Med 18 (1): 71–8. January 2000. doi:10.1016/S0736-4679(99)00178-X. PMID 10645842.
- ↑ "Electrocardiographic ST-segment elevation: correct identification of acute myocardial infarction (AMI) and non-AMI syndromes by emergency physicians". Acad Emerg Med 8 (4): 349–60. April 2001. doi:10.1111/j.1553-2712.2001.tb02113.x. PMID 11282670.
- ↑ David A. Morrow; Elliott M. Antman; Andrew Charlesworth; Richard Cairns; Sabina A. Murphy; James A. de Lemos; Robert P. Giugliano; Carolyn H. McCabe et al. (2000). "TIMI Risk Score for ST-Elevation Myocardial Infarction: A Convenient, Bedside, Clinical Score for Risk Assessment at Presentation: An Intravenous nPA for Treatment of Infarcting Myocardium Early II Trial Substudy". Circulation 102 (17): 2031–7. doi:10.1161/01.cir.102.17.2031. PMID 11044416.
- ↑ David A. Morrow; Elliott M. Antman; Andrew Charlesworth; Richard Cairns; Sabina A. Murphy; James A. de Lemos; Robert P. Giugliano; Carolyn H. McCabe et al. (2000). "The TIMI Risk Score for Unstable Angina/Non–ST Elevation MI: A Method for Prognostication and Therapeutic Decision Making". JAMA 284 (7): 835–42. doi:10.1001/jama.284.7.835. PMID 10938172.
- ↑ "Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE).". BMJ 333 (7578): 2153–8. 2006. doi:10.1136/bmj.38985.646481.55. PMID 17032691.
- ↑ "A prospective validation of the HEART score for chest pain patients at the emergency department.". Circulation 168 (3): 2153–8. 2013. doi:10.1016/j.ijcard.2013.01.255. PMID 23465250.
- ↑ "The Prominent T wave: electrocardiographic differential diagnosis". Am J Emerg Med 20 (3): 243–51. May 2002. doi:10.1053/ajem.2002.32630. PMID 11992348.
- ↑ "Acute coronary syndromes". Emerg. Med. Clin. North Am. 24 (1): 53–89, vi. February 2006. doi:10.1016/j.emc.2005.08.008. PMID 16308113.
- ↑ "The clinical value of the ECG in noncardiac conditions". Chest 125 (4): 1561–76. April 2004. doi:10.1378/chest.125.4.1561. PMID 15078775. http://www.chestjournal.org/cgi/content/full/125/4/1561.
- ↑ 17.0 17.1 17.2 17.3 17.4 gpnotebook.co.uk > ECG changes in myocardial infarction Retrieved on June 16, 2010
External links
- TIMI Risk Score for UA/NSTEMI and STEMI
- Heart Risk Scores Print out by American Heart Association
 |