Medicine:Pringle manoeuvre
| Pringle manoeuvre | |
|---|---|
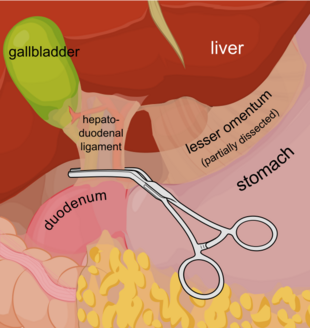 A diagram showing a haemostat being used to clamp the hepatoduodenal ligament. | |
| Specialty | General surgery |
| Uses | Liver surgery |
| Complications | Increased blood loss in patients with chronic venous insufficiency |
| Approach | Open surgery. Compress hepatoduodenal ligament |
The Pringle manoeuvre is a surgical technique used in some abdominal operations and in liver trauma. The hepatoduodenal ligament is clamped either with a surgical tool called a haemostat, an umbilical tape or by hand. This limits blood inflow through the hepatic artery and the portal vein, controlling bleeding from the liver. It was first published by and named after James Hogarth Pringle in 1908.
Uses
The Pringle manoeuvre is used during liver surgery and in some cases of severe liver trauma to minimize blood loss.[1] For short durations of use, it is very effective at reducing intraoperative blood loss.[2] The Pringle manoeuvre is applied during closure of a vena cava injury when an atriocaval shunt is placed.[citation needed]
Limits
The Pringle manoeuvre is more effective in preventing blood loss during liver surgery if central venous pressure is maintained at 5 mmHg or lower. This is due to the fact that Pringle manoeuver technique aims at controlling the blood inflow into the liver, having no effect on the outflow.[3] In case of using Pringle manoeuver during liver trauma, should bleeding continue, it is likely that the inferior vena cava or the hepatic vein are also traumatised.[4] If bleeding continues, a variation in arterial blood flow may be present.
Adverse effects
The Pringle manoeuvre can directly lead to reperfusion injury in the liver, causing impaired function.[5] This is particularly true for long durations of use, such as more than 120 minutes of intermittent Pringle occlusion.[6]
Technique
The Pringle manoeuvre consists in clamping the hepatoduodenal ligament (the free border of the lesser omentum). This interrupts the flow of blood through the hepatic artery and the portal vein, which helps to control bleeding from the liver. The common bile duct is also temporarily closed during this procedure. This can be achieved using:
History
The Pringle manoeuvre was developed by James Hogarth Pringle in the early 1900s in order to attempt to control bleeding during severe liver traumatic injuries.[8]
References
- ↑ Poon, R. T.; Fan, S. T. (2007-01-01), Blumgart, Leslie H.; Belghiti, Jacques; Jarnagin, William R. et al., eds., "Chapter 82 - Liver Resection in Cirrhosis of the Liver" (in en), Surgery of the Liver, Biliary Tract and Pancreas (Fourth Edition) (Philadelphia: W.B. Saunders): pp. 1427–1439, ISBN 978-1-4160-3256-4, http://www.sciencedirect.com/science/article/pii/B9781416032564501010, retrieved 2021-01-25
- ↑ Man, K; Fan, S T; Ng, I O; Lo, C M; Liu, C L; Wong, J (December 1997). "Prospective evaluation of Pringle maneuver in hepatectomy for liver tumors by a randomized study.". Annals of Surgery 226 (6): 704–713. doi:10.1097/00000658-199712000-00007. ISSN 0003-4932. PMID 9409569.
- ↑ Smyrniotis, Vassilios; Kostopanagiotou, Georgia; Theodoraki, Kassiani; Tsantoulas, Dimitrios; Contis, John C (2004-03-01). "The role of central venous pressure and type of vascular control in blood loss during major liver resections" (in en). The American Journal of Surgery 187 (3): 398–402. doi:10.1016/j.amjsurg.2003.12.001. ISSN 0002-9610. PMID 15006570. http://www.sciencedirect.com/science/article/pii/S0002961003005798.
- ↑ Monkhouse, Stanley (16 February 2007). Master Medicine: Clinical Anatomy (2nd ed.). ISBN 9780443102905. https://books.google.com/books?id=da5GJ9P1ejAC. Retrieved 20 December 2016.[page needed]
- ↑ Man, Kwan; Fan, Sheung-Tat (1999-05-01). "Tolerance of the Liver to Intermittent Pringle Maneuver in Hepatectomy for Liver Tumors". Archives of Surgery 134 (5): 533–539. doi:10.1001/archsurg.134.5.533. PMID 10323426.
- ↑ Man, K; Fan, ST; Ng, IO; Lo, CM; Liu, CL; Yu, WC; Wong, J (May 1999). "Tolerance of the liver to intermittent pringle maneuver in hepatectomy for liver tumors.". Archives of Surgery 134 (5): 533–9. doi:10.1001/archsurg.134.5.533. PMID 10323426.
- ↑ Ethun, Cecilia G.; Maithel, Shishir K. (2017-01-01), Jarnagin, William R., ed., "Chapter 103B - Hepatic resection for benign disease and for liver and biliary tumors" (in en), Blumgart's Surgery of the Liver, Biliary Tract and Pancreas, 2-Volume Set (Sixth Edition) (Philadelphia: Elsevier): pp. 1522–1571.e4, ISBN 978-0-323-34062-5, http://www.sciencedirect.com/science/article/pii/B9780323340625001291, retrieved 2021-01-25
- ↑ Graham, Jay A.; Johnson, Lynt B. (2009-01-01), Evans, Stephen R. T., ed., "Chapter 31 - Right Hepatectomy" (in en), Surgical Pitfalls (Philadelphia: W.B. Saunders): pp. 329–338, ISBN 978-1-4160-2951-9, http://www.sciencedirect.com/science/article/pii/B9781416029519500414, retrieved 2021-01-25
 |

