Medicine:Chronic venous insufficiency
| Chronic venous insufficiency | |
|---|---|
| Other names | Chronic venous disease |
 | |
| Mild chronic venous insufficiency, with increased pigmentation of the lower legs. | |
| Specialty | Vascular surgery |
Chronic venous insufficiency (CVI) is a medical condition in which blood pools in the veins, straining the walls of the vein.[1] The most common cause of CVI is superficial venous reflux which is a treatable condition.[2] As functional venous valves are required to provide for efficient blood return from the lower extremities, this condition typically affects the legs. If the impaired vein function causes significant symptoms, such as swelling and ulcer formation, it is referred to as chronic venous disease.[3] It is sometimes called chronic peripheral venous insufficiency and should not be confused with post-thrombotic syndrome in which the deep veins have been damaged by previous deep vein thrombosis.
Most cases of CVI can be improved with treatments to the superficial venous system or stenting the deep system. Varicose veins for example can now be treated by local anesthetic endovenous surgery.
Rates of CVI are higher in women than in men.[4][5] Other risk factors include genetics, smoking, obesity, pregnancy, and prolonged standing.[6]
Signs and symptoms
Signs and symptoms of CVI in the leg include the following:
- Varicose veins
- Itching (pruritus)
- Hyperpigmentation
- Phlebetic lymphedema[7]
- Chronic swelling of the legs and ankles
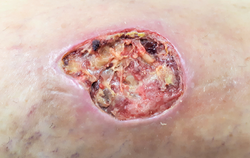
- Leg ulcer
CVI in the leg may cause the following:
- Venous stasis
- Venous ulcers[8]
- Stasis dermatitis,[8] also known as varicose eczema
- Contact dermatitis,[8] a disrupted epidermal barrier due to venous insufficiency, making patients more susceptible than the general population to contact sensitization and subsequent dermatitis.
- Atrophie blanche,[8] an end point of a variety of conditions that appears as atrophic plaques of ivory white skin with telangiectasias. It represents late sequelae of lipodermatosclerosis where the skin has lost its nutrient blood flow.
- Lipodermatosclerosis,[8] an indurated plaque in the medial malleolus.
- Malignancy,[8] malignant degeneration being a rare but important complication of venous disease since tumors that develop in the setting of an ulcer tend to be more aggressive.
- Pain,[8] a feature of venous disease often overlooked and commonly undertreated.
- Anxiety[8]
- Depression[8]
- Inflammation
- Cellulitis
Causes
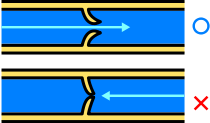
The most common cause of chronic venous insufficiency is reflux of the venous valves of superficial veins.[2] This may in turn be caused by several conditions:
- Deep vein thrombosis (DVT), that is, blood clots in the deep veins. Chronic venous insufficiency caused by DVT may be described as postthrombotic syndrome. DVT triggers an inflammatory response subsequently injuring the vein wall.[6]
- Superficial vein thrombosis.
- Phlebitis
- May–Thurner syndrome. This is a rare condition in which blood clots occur in the iliofemoral vein due to compression of the blood vessels in the leg. The specific problem is compression of the left common iliac vein by the overlying right common iliac artery. Many May-Thurner compressions are overlooked when there is no blood clot. More and more of them get nowadays diagnosed and treated (by stenting) due to advanced imaging techniques.[9]
Deep and superficial vein thrombosis may in turn be caused by thrombophilia, which is an increased propensity of forming blood clots.[citation needed]
Arteriovenous fistula (an abnormal connection or passageway between an artery and a vein) may cause chronic venous insufficiency even with working vein valves.[citation needed]
Diagnosis
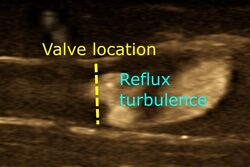
History and examination by a clinician for characteristic signs and symptoms are sufficient in many cases in ruling out systemic causes of venous hypertension such as hypervolemia and heart failure.[10] A duplex ultrasound (doppler ultrasonography and b-mode) can detect venous obstruction or valvular incompetence as the cause, and is used for planning venous ablation procedures, but it is not necessary in suspected venous insufficiency where surgical intervention is not indicated.[10][6]
Insufficiency within a venous segment is defined as reflux of more than 0.5 seconds with distal compression. Invasive venography can be used in patients who may require surgery or have suspicion of venous stenosis. Other modalities that may be employed are: ankle-brachial index to exclude arterial pathology, air or photoplethysmography, intravascular ultrasound, and ambulatory venous pressures, which provides a global assessment of venous competence. Venous plethysmography can assess for reflux and muscle pump dysfunction but the test is laborious and rarely done.[6]
The venous filling time after the patient is asked to stand up from a seated position also is used to assess for CVI. Rapid filling of the legs less than 20 seconds is abnormal.[6]
Classification
CEAP classification is based on Clinical, Etiological (causal), Anatomical, and Pathophysiological factors.[11] According to Widmer Classification for assessment of chronic venous insufficiency (CVI), diagnosis of chronic venous insufficiency is clearly differentiated from varicose veins.[12] It has been developed to guide decision-making in chronic venous insufficiency evaluation and treatment.[6]
The CEAP classification for CVI is as follows:[citation needed]
- Clinical
- C0: no obvious feature of venous disease
- C1: the presence of reticular or spider veins
- C2: Obvious varicose veins
- C3: Presence of edema but no skin changes
- C4: skin discoloration, pigmentation
- C5: Ulcer that has healed
- C6: Acute ulcer
- Etiology
- Primary
- Secondary (trauma, birth control pill)
- Congenital (Klipper trenaunay)
- No cause is known
- Anatomic
- Superficial
- Deep
- Perforator
- No obvious anatomic location
- Pathophysiology
- Obstruction, thrombosis
- Reflux
- Obstruction and reflux
- No venous pathology
Management
Conservative
Conservative treatment of CVI in the leg involves symptomatic treatment and efforts to prevent the condition from getting worse instead of effecting a cure. This may include
- Manual compression lymphatic massage therapy
- Red vine leaf extract may have a therapeutic benefit.[13]
- Sequential compression pump
- Ankle pump
- Compression stockings
- Blood pressure medicine
- Hydroxyethylrutoside medication[14]
- Frequent periods of rest elevating the legs above the heart level
- Tilting the bed so that the feet are above the heart. This may be achieved by using a 20 cm (7-inch) bed wedge or sleeping in a 6 degree Trendelenburg position.
Surgical
Surgical treatment of CVI attempts a cure by physically changing the veins with incompetent valves. Surgical treatments for CVI include the following:
- Ligation.[15] Tying off a vein to prevent blood flow
- Vein stripping.[15] Removal of the vein.
- Surgical repair.[15]
- Endovenous Laser Ablation
- Vein transplant.[15]
- Subfascial endoscopic perforator surgery.[15] Tying off the vein with an endoscope.
- Valve repair (experimental)
- Valve transposition (experimental)
- Hemodynamic surgeries.
Venous insufficiency conservative, hemodynamic and ambulatory treatment (CHIVA method) is an ultrasound guided, minimally invasive surgery strategic for the treatment of varicose veins, performed under local anaesthetic.[16]
Prognosis
CVI is not a benign disorder and, with its progression, can lead to morbidity. Venous ulcers are common and very difficult to treat. Chronic venous ulcers are painful and debilitating. Even with treatment, recurrences are common if venous hypertension persists. Nearly 60% develop phlebitis which often progresses to deep vein thrombosis in more than 50% of patients. The venous insufficiency can also lead to severe hemorrhage. Surgery for CVI remains unsatisfactory despite the availability of numerous procedures.[6]
References
- ↑ "Chronic Venous Insufficiency". Society for Vascular Surgery. December 1, 2009. http://www.vascularweb.org/vascularhealth/Pages/chronic-venous-insufficiency.aspx.
- ↑ 2.0 2.1 Whiteley MS (2011). "Understanding Venous Reflux - the cause of varicose veins and venous leg ulcers". Whiteley Publishing. http://www.markwhiteley.co.uk/books-mark-whiteley.php.
- ↑ Venous Insufficiency. 2022. PMID 28613694. https://www.ncbi.nlm.nih.gov/books/NBK430975/. Retrieved 9 July 2021.
- ↑ "Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study.". Journal of Epidemiology & Community Health (J Epidemiol Community Health.) 53 (3): 149–153. 1999. doi:10.1136/jech.53.3.149. PMID 10396491.
- ↑ "Incidence and risk factors for venous reflux in the general population: Edinburgh Vein Study. Eur J Vasc Endovasc Surg. 2014 Aug;48(2):208-14. doi: 10.1016/j.ejvs.2014.05.017. Epub 2014 Jun 18.". European Journal of Vascular and Endovascular Surgery (Eur J Vasc Endovasc Surg.) 48 (2): 208–14. May 2014. doi:10.1016/j.ejvs.2014.05.017. PMID 24951373. http://www.ejves.com/article/S1078-5884(14)00271-8/abstract. Retrieved January 8, 2015.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Patel, Shivik K.; Surowiec, Scott M. (2020). "Venous Insufficiency". StatPearls (StatPearls Publishing). PMID 28613694. https://www.ncbi.nlm.nih.gov/books/NBK430975/. Retrieved 9 July 2020.
 Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
Text was copied from this source, which is available under a Creative Commons Attribution 4.0 International License.
- ↑ Avril, Stéphane; Badel, Pierre; Dubuis, Laura; Rohan, Pierre-Yves; Debayle, Johan; Couzan, Serge; Pouget, Jean-Fraçois (25 January 2012). Gefen, Amit. ed. Patient-Specific Modeling in Tomorrow's Medicine. Springer. pp. 218, 220. ISBN 978-3-642-24618-0. https://books.google.com/books?id=aHgIi7mjBhMC&pg=PA220. Retrieved 12 November 2020.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 8.8 "Dermatologic complications of chronic venous disease: medical management and beyond". Ann Vasc Surg 21 (5): 652–62. Sep 2007. doi:10.1016/j.avsg.2007.07.002. PMID 17823046.
- ↑ "Chronic Venous Insufficiency". https://www.lecturio.com/concepts/chronic-venous-insufficiency/.
- ↑ 10.0 10.1 Patrick C Alguire, Barbara M Mathes. "Diagnostic evaluation of lower extremity chronic venous insufficiency". https://www.uptodate.com/contents/diagnostic-evaluation-of-lower-extremity-chronic-venous-insufficiency. Topic last updated: Dec 04, 2017.
- ↑ Antignani, P. L. (August 2001). "Classification of chronic venous insufficiency: a review". Angiology 52 Suppl 1: S17–26. doi:10.1177/0003319701052001S03. ISSN 0003-3197. PMID 11510593.
- ↑ Hafner, Jürg (1999-01-01) (in en). Management of Leg Ulcers. Karger Medical and Scientific Publishers. p. 81. ISBN 978-3-8055-6654-4. https://books.google.com/books?id=5FF9uoPeITgC&pg=PA81.
- ↑ "Red Vine Leaf Extract (AS 195) Can Improve Some Signs and Symptoms of Chronic Venous Insufficiency, a Systematic Review". Phytotherapy Research 34 (10): 2577–2585. 2020. doi:10.1002/ptr.6705. PMID 32314844.
- ↑ Frick, RW (March 2000). "Three treatments for chronic venous insufficiency: escin, hydroxyethylrutoside, and Daflon.". Angiology 51 (3): 197–205. doi:10.1177/000331970005100303. PMID 10744007.
- ↑ 15.0 15.1 15.2 15.3 15.4 "Chronic Venous Insufficiency". hopkinsmedicine.org. 8 August 2021. http://www.hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/chronic_venous_insufficiency_85,P08250/.
- ↑ Mowatt-Larssen, Eric; Shortell, Cynthia (2010). "CHIVA". Seminars in Vascular Surgery 23 (2): 118–22. doi:10.1053/j.semvascsurg.2010.01.008. PMID 20685567.
External links
| Classification | |
|---|---|
| External resources |
 |
