Biology:Antibiotic sensitivity
Antibiotic sensitivity or antibiotic susceptibility is the susceptibility of bacteria to antibiotics.
Motivation
In clinical practice, antibiotics are most frequently prescribed on the basis of general guidelines and knowledge about sensitivity: e.g. uncomplicated urinary tract infections can be treated with a first generation quinolone, etc. This is because Escherichia coli is the most likely causative pathogen, and it is known to be sensitive to quinolone treatment. However, many bacteria are known to be resistant to several classes of antibiotics, and treatment is not so straightforward.
Because susceptibility can vary even within a species (with some strains being more resistant than others), antibiotic susceptibility testing (AST) is usually carried out to determine which antibiotic will be most successful in treating a bacterial infection in vivo.
Testing methods
Tests for antibiotic sensitivity include:
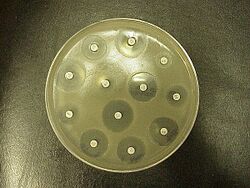
- Kirby-Bauer method. Small wafers containing antibiotics are placed onto a plate upon which bacteria are growing. If the bacteria are sensitive to the antibiotic, a clear ring, or zone of inhibition, is seen around the wafer indicating poor growth.[1] Müeller-Hinton agar is frequently used in this antibiotic susceptibility test.[2][3]
- Stokes method
- Etest (also based on antibiotic diffusion)
- Agar and Broth dilution methods for minimum inhibitory concentration (MIC) determination.[4][5]
Antibiogram
The results of the test are reported on the antibiogram. Once a culture is established, there are two possible ways to get an antibiogram:
- a semi-quantitative way based on diffusion (Kirby-Bauer method); small discs containing different antibiotics, or impregnated paper discs, are dropped in different zones of the culture on an agar plate, which is a nutrient-rich environment in which bacteria can grow. The antibiotic will diffuse in the area surrounding each tablet, and a disc of bacterial lysis will become visible. Since the concentration of the antibiotic was the highest at the centre, and the lowest at the edge of this zone, the diameter is suggestive for the Minimum Inhibitory Concentration, or MIC, (conversion of the diameter in millimeter to the MIC, in μg/ml, is based on known linear regression curves).
- a quantitative way based on dilution: a dilution series of antibiotics is established (this is a series of reaction vials with progressively lower concentrations of antibiotic substance). The last vial in which no bacteria grow contains the antibiotic at the Minimal Inhibiting Concentration.
Analysis
Once the MIC is calculated, it can be compared to known values for a given bacterium and antibiotic: e.g. a MIC > 0,06 μg/ml may be interpreted as a penicillin-resistant Streptococcus pneumoniae. Such information may be useful to the clinician, who can change the empirical treatment, to a more custom-tailored treatment that is directed only at the causative bacterium.
Often clinical specimens are sent to the clinical laboratory for culture and sensitivity (C&S), which is culture and antibiotic sensitivity testing offered as one combined service. This is because the clinician needs to know which organism is causing the infection, and which drugs will specifically work against this strain.
Some antibiotics actually kill the bacteria (bactericidal), whereas others merely prevent the bacteria from multiplying (bacteriostatic) so that the host's immune system can overcome them; this may affect testing procedures.[citation needed]
Clinical practice
Ideal antibiotic therapy is based on determination of the aetiological agent and its relevant antibiotic sensitivity. Empiric treatment is often started before laboratory microbiological reports are available when treatment should not be delayed due to the seriousness of the disease. The effectiveness of individual antibiotics varies with the location of the infection, the ability of the antibiotic to reach the site of infection, and the ability of the bacteria to resist or inactivate the antibiotic.

An antibiogram is the result of an antibiotic sensitivity test. It is by definition an in vitro sensitivity, but the correlation of in vitro to in vivo sensitivity is often high enough for the test to be clinically useful.
This is especially the case in vulnerable patients, such as patients in the intensive care unit. When these patients develop a hospital-acquired pneumonia, more hardy bacteria like Pseudomonas aeruginosa are potentially involved. Treatment is then generally started on the basis of surveillance data about the local pathogens probably involved. This first treatment, based on statistical information about former patients, and aimed at a large group of potentially involved microbes, is called empirical treatment.
Before starting this treatment, the physician will collect a sample from a suspected contaminated compartment: a blood sample when bacteria possibly have invaded the bloodstream, a sputum sample in the case of a ventilator associated pneumonia, and a urine sample in the case of a urinary tract infection. These samples are transferred to the microbiology lab, which looks at the sample under the microscope, and tries to culture the bacteria. This can help in the diagnosis.
Further research
Point-of-care resistance diagnostics (POCRD) can help practitioners avoid prescribing unnecessary antibiotics in the style of precision medicine.[6] Traditional techniques typically take 12 to 48 hours[7] whereas rapid testing using molecular diagnostics is defined as "being feasible within an 8-h working shift".[7] Progress has been slow due to a range of reasons including cost and regulation.[8]
In 2016, the United States National Institutes of Health (NIH) announced the Antimicrobial Resistance Diagnostic Challenge as a $20 million prize to encourage the development of diagnostic tests to identify highly resistant bacterial infections.[9] Also, the US Congress wants drug companies that are not working on new resistance antibiotics to do so and if not may pay into a fund if they are not working on new antibiotics to combat the antibiotic resistance crisis.[10]
As of 2017, point-of-care resistance diagnostics (POCRD) was available for methicillin-resistant Staphyloccus aureus (MRSA), rifampin-resistant Mycobacterium tuberculosis (TB), and vancomycin-resistant Enterococci (VRE) through GeneXpert by molecular diagnostics company Cepheid.[11]
See also
- Antibiotic resistance
- Miles-Misra method
- Bacterial culture
- Throat culture
- Laboratory specimen
References
- ↑ http://www.uphs.upenn.edu/bugdrug/antibiotic_manual/bk.html
- ↑ "Testing the Effectiveness of Antimicrobials | Microbiology". https://courses.lumenlearning.com/microbiology/chapter/testing-the-effectiveness-of-antimicrobials/.
- ↑ http://www.microrao.com/micronotes/antibiotic.pdf
- ↑ http://www.slideshare.net/doctorrao/antibiotic-sensitivity-testing-presentation
- ↑ http://cid.oxfordjournals.org/content/49/11/1749.full
- ↑ "Diagnostics Are Helping Counter Antimicrobial Resistance, But More Work Is Needed" (in en). MDDI Online. 2018-11-20. https://www.mddionline.com/diagnostics-are-helping-counter-antimicrobial-resistance-more-work-needed.
- ↑ 7.0 7.1 "Developmental roadmap for antimicrobial susceptibility testing systems" (in En). Nature Reviews. Microbiology 17 (1): 51–62. January 2019. doi:10.1038/s41579-018-0098-9. PMID 30333569.
- ↑ "Progress on antibiotic resistance" (in EN). Nature 562 (7727): 307. October 2018. doi:10.1038/d41586-018-07031-7. PMID 30333595.
- ↑ Mullin, Emily (19 September 2014). "Antibiotics R & D to get critical lift by executive order, Obama advisory group". fiercebiotech.com. http://www.fiercebiotech.com/story/antibiotics-rd-get-critical-lift-executive-order-obama-advisory-group/2014-09-19.
- ↑ MacKenzie, Debora (2019). "Facing the resistance" (in en). New Scientist 241 (3213): 20–21. doi:10.1016/S0262-4079(19)30114-9.
- ↑ McAdams, David (January 2017). "Resistance diagnosis and the changing epidemiology of antibiotic resistance" (in en). Annals of the New York Academy of Sciences 1388 (1): 5–17. doi:10.1111/nyas.13300. ISSN 0077-8923. PMID 28134444.
Jump up
^ http://www.uphs.upenn.edu/bugdrug/antibiotic_manual/bk.html Jump up ^ http://www.slideshare.net/doctorrao/antibiotic-sensitivity-testing-presentation Jump up ^ http://cid.oxfordjournals.org/content/49/11/1749.full Jump up ^ http://www.microrao.com/micronotes/antibiotic.pdf
External links
- Research Data
- Raw Data
- Antibiogram technique video (diffusion method)
