Biology:Chemotactic drug-targeting
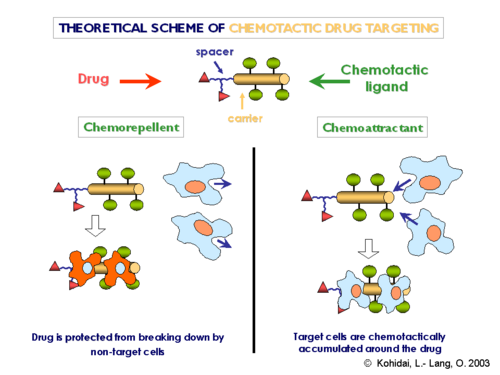
Targeted drug delivery is one of many ways researchers seek to improve drug delivery systems' overall efficacy, safety, and delivery. Within this medical field is a special reversal form of drug delivery called chemotactic drug targeting.[1][2] By using chemical agents to help guide a drug carrier to a specific location within the body, this innovative approach seeks to improve precision and control during the drug delivery process, decrease the risk of toxicity, and potentially lower the required medical dosage needed.[2][3][4][5] The general components of the conjugates are designed as follows: (i) carrier – regularly possessing promoter effect also on internalization into the cell; (ii) chemotactically active ligands acting on the target cells; (iii) drug to be delivered in a selective way and (iv) spacer sequence which joins drug molecule to the carrier and due to it enzyme labile moiety makes possible the intracellular compartment specific release of the drug. Careful selection of chemotactic component of the ligand not only the chemoattractant character could be expended, however, chemorepellent ligands are also valuable as they are useful to keep away cell populations degrading the conjugate containing the drug. In a larger sense, chemotactic drug-targeting has the potential to improve cancer, inflammation, and arthritis treatment by taking advantage of the difference in environment between the target site and its surroundings.[6][7][8] Therefore, this Wikipedia article aims to provide a brief overview of chemotactic drug targeting, the principles behind the approach, possible limitations and advantages, and its application to cancer and inflammation.
Importance of Chemotaxis in Chemotactic Drug-Targeting
In general terms, chemotaxis is a biological process where living entities, such as cells or organisms, detect, maneuver, and react in response to a chemical signal in their environment.[1] Such a phenomenon is critical for many biological processes, including but not limited to wound healing, detection of food, and avoidance of many toxins.[2] Chemotaxis also plays an essential role in serval diseases, such as tumor metastasis, the recruitment of T-lymphocytes during inflammation, and HIV-1 entry into T cells.[6][9][10] At the core of chemotaxis are specialized sensory cells called chemoreceptors. These cells allow an organism to detect chemical molecules within its environment and respond accordingly. Such chemical molecules are either known as chemoattractants or chemorepellents, which play a crucial role in attracting or repelling the organism towards or away from the source of the chemical signal, respectively. Thus, with this natural process of chemotaxis in mind, researchers have sought to apply the same phenomenon to targeted drug delivery, a medical technique aimed at delivering drugs to a specific cell, tissue, or organ within the body while minimizing its disruptive effects on healthy tissue.[4] By using both chemotaxes to help guide the drug delivery process, researchers aim to reduce toxicity by avoiding healthy tissues, improve drug efficacy by focusing only on the intended site, and decrease drug dosage by delivering the directly rather than throughout the whole body.[3][11]
Chemotactic Drug Targeting Systems
Chemotactic drug delivery systems are an emerging field of drug delivery that aims to apply the natural phenomenon of chemotaxis in guiding and delivering a drug to a specific tissue or cell within the body. Thus, similar to how organisms use chemotaxis, researchers have designed drug delivery systems to detect, maneuver, and react to chemical molecules released by a desired cell or its surrounding area.
Microdroplets
Recent progress in the field of microfluidics has led to the development of microdroplets, a new drug-delivery system that uses uniform droplets to deliver drugs to specific locations within the body.[2][12] These microdroplets allow researchers to load drugs during the polymerization step of their formation and provide variations in porosity, which can control the time it takes to release a therapeutic payload.[13] Thus, by using the natural process of chemotaxis, researchers aim to guide these tiny droplets by using chemical gradients released by a specific cell, tissue, or organ within the body.[2][4][12] In fact, a few examples of microdroplet systems that use chemotaxis are self-propelling, ionic liquid-based, and synthetic base.[2][12] These microdroplet-based drug delivery systems offer several advantages over traditional drug delivery methods, which are talked about later in the advantage and limitations subsection of this article. Overall, the development of microdroplet-based drug delivery systems using the phenomenon of chemotaxis is just one of may avenues to potentially revolutionize the field of medicine and targeted drug delivery.[14]
Protocells
Another drug delivery system that has shown potential for chemotactic applicability is protocells.[15] In general, protocells are artificial cells that mimic living cells but cannot reproduce and have genetic mutations like living cells do.[15] Moreover, protocells combine the advantages of liposomes with that of mesoporous silica nanoparticles.[16] These advantages include but are not limited to stability, large capacity for various cargos, low toxicity, immunogenicity, and the ability to circulate the blood for long periods.[16] Thus, researchers aim to create a tunable chemotactic protocell that can move towards or away from a chemical signal.[17][18] In fact, researchers have devised a way to use the enzymes catalase, urease, and ATPase to move the protocell closer or further away from the reactant, giving them direction and movement control of these protocells.[17][18] Overall, the development of chemotactic controlled protocols holds great promise for the targeted delivery of drugs to specific areas of the body, potentially increasing treatment efficacy while minimizing side effects. However, more research is needed to fully understand the capabilities and limitations of protocells as drug delivery systems and optimize their design and functionality for specific applications.
Biological and Bio-hybrid drug carriers
Finally, biological and bio-hybrid drug carriers have shown potential for chemotactic applications. In general, these systems are inspired by microorganisms or cells to help design drug delivery systems that mimic their surface, shape, texture, and movement.[4][19] One phenomenon that has become increasingly popular in improving the movement and release of bio-hybrid drug carriers is that of chemotaxis. Indeed, thanks to their natural chemotactic sensing property, bacteria can be used to locate a tumor, carry a therapeutic payload to the site, and release that drug in a controlled manner.[4] Researchers can also genetically modify these bacteria to produce a specific protein like anti-tumor cytotoxins for cancer treatment.[4]
Yet, this is not to say that they don't come with their own set of challenges and limitations. For one, the genetic modifications of the bacteria used can be manipulated by recent or unforeseen mutations, leading to a decrease in the efficacy of the drug and drug carrier.[4] Moreover, the therapeutic proteins produced may have incomplete protein folding, decreasing the drug's effectiveness or causing unforeseen side effects.[4] Generally speaking, using bacteria may provide some advantages, but further research and development are still needed to address their limitations.
Another example of bio-hybrid drug carriers is human cells, like macrophages, which offer compatibility with the human immune system and a simple way to load drugs as a bio-hybrid drug carrier.[4] Leukocytes demonstrate great promise because Tumor cells secrete large amounts of chemoattractants when the cell undergoes inflammation.[4] This secretion of chemoattractants naturally attracts leukocytes, such as macrophages, to the T cell location.[4] Thus, with their well-known chemotactic homing behavior to inflammation or pathogens' sites in mind, researchers can manipulate leukocytes to carry and deliver a therapeutic payload to the tumor site. However, this is not to say that Biological and bio-hybrid drug carriers do not have challenges and limitations of their own. For example, Leukocytes cannot penetrate deeply into the tumors, have a low capacity for carrying drugs, and slow down when the tumor size reduces. Thus, similar to bacteria drug carriers, further research and development are still needed to address their limitations and improve the overall drug delivery system.
Applications of Chemotactic Drug Targeting
The applications of chemotactic drug delivery systems include but are not limited to cancer therapy, wound healing, and inflammation. The ability to target specific cells and locations within the body through chemical cues has opened up new avenues for the field of drug delivery, allowing for increased drug efficacy and reducing harmful side effects.
Cancer
Cancer is not just one disease but a group of diseases involving abnormal cell growth and metastasis of such cells to other body parts.[20][21] There are also several types of cancers, each with its own distinctive characteristics and stages that may require different treatment or targeted drug delivery approaches.[21][22] Yet, even these treatments have their own advantages and disadvantages. Thus, since the discovery of cancer, researchers have constantly been developing new and innovative cancer treatments, including chemotactic drug delivery. For example, and as mentioned earlier in this article, researchers have sought to use microdroplets, protocells, and biological and bio-hybrid drug carriers to deliver drugs to cancer cells in a more effective manner, while reducing unwanted side effects.[2][4][12][15][19] In fact, the justification for using such systems, guided by chemotaxis, is that the environment inside a tumor has a higher resting temperature, higher peroxide concentration, lower pH, and a lower oxygen concentration than its surrounding tissue.[4] With these unique conditions, researchers can exploit chemotactic drug delivery to target tumor cells directly, avoiding healthy tissues, reducing toxicity, improving drug efficacy, and decreasing drug dosage.[12][13]
Inflammation
Inflammation is the body's response to foreign objects, irritants, germs, and even pathogens. Although such a response is standard in some cases, if left untreated, chronic inflammation can lead to muscle degeneration, gastrointestinal disorders, and some types of cancers.[23][24] While most treatments, such as anti-inflammatory drugs and steroid injections, can help relieve symptoms, they often fail to address the condition's underlying cause. Therefore, researchers have sought to explore new and innovative ways of inflammation treatment, such as chemotactic drug delivery.
One promising drug delivery system was based on engineered neutrophils that targeted inflammation sites through chemotaxis's unique properties.[4][7] This approach took advantage of the concentration difference between iNOS and ROS for inflammatory disease sites and normal tissues.[7] By doing so, this drug delivery system provides the possibility to target areas of inflammation, increase drug efficacy, and minimize damage to the surrounding tissue.[3][11] Moreover, because this concentration gradient is ubiquitous in the microenvironment of inflammatory diseases, common drug-targeting limitations such as individual differences can be avoided.[7] Another example of an innovative drug delivery system that uses the property of chemotaxis is leukocytes.[4] Indeed, during inflammation, the molecules on a cell that allows for adhesion are overly produced.[4] With this unique condition, researchers can modify leukocytes to quickly detect the cell, attach itself to the surface, and deliver a therapeutic payload.[4] Overall, many promising therapies and drug delivery systems are being developed to target inflammation more effectively. Chemotactic drug delivery systems are just one of many promising avenues that seek to increase target sites specifically, decreasing the needed drug dosage, reducing toxicity, and increasing drug efficacy.[3][4][11]
Advantages and limitations of Chemotactic Drug Targeting
While this emerging field of drug delivery shows excellent promise in targeting specific cells and locations within the body, understanding current challenges and drawbacks can allow researchers to optimize design, development, and delivery to improve the overall outcome of their medical treatment.
Microdroplets
- Advantages
- By using uniform droplets to deliver therapeutic payloads to specific locations in the body, researchers can achieve greater precision and control over drug delivery while also minimizing toxicity and harmful side effects.[4][1][14] For example, these droplets can be quickly loaded during the polymerization process and can be varied in porosity to control the time it takes to release a drug.[13] Microdroplets-based drug delivery also has a significant advantage over traditional systems in that they can minimize side effects, reduce the need for invasive procedures, and even improve a drug's efficacy. Overall, microdroplet-based drug delivery systems show great promise for revolutionizing medicine with significant potential for targeted drug delivery.
- Limitations
- Nevertheless, it is essential to note some common challenges associated with microdroplet-based drug delivery systems, including their biocompatibility, toxicity, and scalability.[2] The biocompatibility and toxicity of Microdroplets are essential to consider because these can affect a drug's safety and overall efficacy, causing unwanted side effects and possibly death. On the other hand, scalability is another crucial challenge to consider because this aspect can lead to increased manufacturing costs, problems with quality control, and limitations in equipment used. All in all, even with great promise to revolutionize targeted drug delivery, researchers must keep in mind the biocompatibility, toxicity, and scalability of microdroplet-based drug delivery systems when using them.
Protocells
- Advantages
- At large, protocells are advantageous because they can store more drugs, be loaded faster than other nanomedicine delivery systems, and are more stable than liposomes.[25] By keeping more drugs, researchers can reduce the quantity of medications needed to be administered, potentially reducing side effects and toxicity. In like manner, controlling the direction and movement of a drug also reduces the amount of medication needed, increases the speed of delivery, and allows for the controlled release of high-concentration multicomponent cargo within cancer cells.[26] Finally, the stability of protocells is vital because it ensures that the drugs remain effective and do not degrade before reaching their target. Overall, the development of protocells as a drug delivery system, coupled with chemotactic properties, holds great promise for targeted drug delivery.
- Limitations
- One fundamental limitation of protocells is their modularity and versatility, which must be accounted for when assessing clinical applications.[16] Modularity and versatility are essential considerations for targeted drug delivery because they enable the customization and adaptation of drug delivery systems to meet specific clinical needs. In fact, without modularity and versatility, it will be hard to tailor protocells to different therapeutic applications and particular populations. Another critical challenge, especially when using enzymes to maneuver the protocell, is that the motility reduces when the enzymes become oversaturated with the chemical stimuli.[16] Reducing motility becomes a problem because this is essential for targeted drug delivery efficiency, limiting the system's effectiveness and increasing the risk of off-target effects. Therefore, further research is still needed to improve our understanding of protocells and their potential clinical applications.
Biological and Bio-hybrid drug carriers
- Advantages
- Some advantages to Biological and bio-hybrid drug carriers include but are not limited to offering compatibility with the human immune system, having the potential to be genetically modified, and having the capacity to hold drugs.[4] Moreover, an essential advantage is their natural property of homing to inflammation and tumor sites. This natural property of homing to inflammation and tumor sites can enhance the targeted delivery of drugs, minimizing the risk of off-target effects and reducing the required dosage.[3][4][11] Additionally, these systems have the potential to increase drug stability and prolong circulation time in the body, improving drug efficacy and reducing the frequency of dosing.[3][4][11] Overall, these advantages make biological and bio-hybrid drug carriers promising for developing more effective and targeted drug delivery systems.
- Limitations
- One limitation of Biological and bio-hybrid drug carriers, especially leukocytes, is that they have a low drug-carrying capacity.[27][4] A limit in the carrying capacity of a carrier means that researchers will have to use more medication to achieve the desired therapeutic effect, increasing the risk of adverse side effects and the cost of the treatment. Moreover, the short lifespan can limit their potential use for long-term drug delivery applications [4] [35]. Coupling this aspect with an inability to penetrate deep into tumors and the potential for genetic mutations can pose significant challenges for future drug delivery systems.[4] Therefore, despite their advantages, further research and development are needed to address current limitations and improve their clinical feasibility.
Conclusion
Generally speaking, chemotactic drug-targeting is a drug delivery strategy with promising avenues for treating diseases such as cancer and inflammation. This approach mimics the biological process of chemotaxis, which biological organisms use to detect, maneuver, and react to chemical signals in their environment. By applying this technique to targeted drug delivery, researchers aim to create drugs that can precisely reach their intended targets, minimizing the potential for side effects, improving drug efficacy, and decreasing drug dosage. Some examples include but are not limited to microdroplets, protocells, biological and bio-hybrid drug carriers, leukocytes, and neutrophils.
While chemotactic drug targeting holds great promise for drug delivery, there are key advantages and limitations that must be considered. One main advantage is that these systems can precisely target specific cells, tissues, or organs within the body while minimizing their disruptive effects on healthy tissue. Moreover, by delivering the drug directly to the desired target, researchers can effectively reduce the required drug dosage needed. However, some limitations to chemotactic drug targeting include issues with biocompatibility, drug-carrying capacity, and the life span of specific carriers. Another major challenge with this approach is motility, when either the chemical stimuli diminish, or the attached enzymes become oversaturated. This can limit the effectiveness of the drug delivery system and may require additional modifications to improve its performance. Thus, although these approaches have shown great promise, more research is still needed to fully understand chemotaxis mechanisms and optimize this property for targeted drug delivery strategies.
References
- ↑ 1.0 1.1 1.2 Almijalli, Mohammed; Ibrahim, Moustafa; Saad, Ali; Saad, Mazen (2021-05-28). "Chemotaxis Model for Drug Delivery Using Turing's Instability and Non-Linear Diffusion" (in en). Applied Sciences 11 (11): 4979. doi:10.3390/app11114979. ISSN 2076-3417.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Khodarahmian, Kobra; Ghiasvand, Alireza (2022-01-25). "Mimic Nature Using Chemotaxis of Ionic Liquid Microdroplets for Drug Delivery Purposes" (in en). Molecules 27 (3): 786. doi:10.3390/molecules27030786. ISSN 1420-3049. PMID 35164048.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Lagzi, István (2013-08-01). "Chemical robotics — chemotactic drug carriers" (in en). Open Medicine 8 (4): 377–382. doi:10.2478/s11536-012-0130-9. ISSN 2391-5463.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 Nguyen, Hung V.; Faivre, Vincent (June 2020). "Targeted drug delivery therapies inspired by natural taxes" (in en). Journal of Controlled Release 322: 439–456. doi:10.1016/j.jconrel.2020.04.005. PMID 32259545.
- ↑ Láng, O.; Török, K.; Mező, G.; Hudecz F.; Kőhidai, L. (2003). Chemotactic conjugates New Aspects in Drug-Targeting.. pp. 118.
- ↑ 6.0 6.1 Roussos, Evanthia T.; Condeelis, John S.; Patsialou, Antonia (August 2011). "Chemotaxis in cancer" (in en). Nature Reviews Cancer 11 (8): 573–587. doi:10.1038/nrc3078. ISSN 1474-175X. PMID 21779009.
- ↑ 7.0 7.1 7.2 7.3 Li, Ting; Liu, Zhiyong; Hu, Jinglei; Chen, Lin; Chen, Tiantian; Tang, Qianqian; Yu, Bixia; Zhao, Bo et al. (November 2022). "A Universal Chemotactic Targeted Delivery Strategy for Inflammatory Diseases" (in en). Advanced Materials 34 (47): 2206654. doi:10.1002/adma.202206654. ISSN 0935-9648. PMID 36122571. https://onlinelibrary.wiley.com/doi/10.1002/adma.202206654.
- ↑ Damsker, Jesse M.; Okwumabua, Ifeanyi; Pushkarsky, Tatiana; Arora, Kamalpreet; Bukrinsky, Michael I.; Constant, Stephanie L. (January 2009). "Targeting the chemotactic function of CD147 reduces collagen-induced arthritis" (in en). Immunology 126 (1): 55–62. doi:10.1111/j.1365-2567.2008.02877.x. PMID 18557953.
- ↑ Baggiolini, Marco (April 1998). "Chemokines and leukocyte traffic" (in en). Nature 392 (6676): 565–568. doi:10.1038/33340. ISSN 0028-0836. PMID 9560152. Bibcode: 1998Natur.392..565B. http://www.nature.com/articles/33340.
- ↑ D'Souza, M. Patricia; Harden, Victoria (December 1996). "Chemokines and HIV–1 second receptors" (in en). Nature Medicine 2 (12): 1293–1300. doi:10.1038/nm1296-1293. ISSN 1078-8956. PMID 8946819. http://www.nature.com/articles/nm1296-1293.
- ↑ 11.0 11.1 11.2 11.3 11.4 Sahari, Ali; Traore, Mahama A.; Scharf, Birgit E.; Behkam, Bahareh (October 2014). "Directed transport of bacteria-based drug delivery vehicles: bacterial chemotaxis dominates particle shape" (in en). Biomedical Microdevices 16 (5): 717–725. doi:10.1007/s10544-014-9876-y. ISSN 1387-2176. PMID 24907051. http://link.springer.com/10.1007/s10544-014-9876-y.
- ↑ 12.0 12.1 12.2 12.3 12.4 Theberge, Ashleigh B.; Courtois, Fabienne; Schaerli, Yolanda; Fischlechner, Martin; Abell, Chris; Hollfelder, Florian; Huck, Wilhelm T. S. (2010-08-09). "Microdroplets in Microfluidics: An Evolving Platform for Discoveries in Chemistry and Biology" (in en). Angewandte Chemie International Edition 49 (34): 5846–5868. doi:10.1002/anie.200906653. PMID 20572214.
- ↑ 13.0 13.1 13.2 Owen, Markus R.; Byrne, Helen M.; Lewis, Claire E. (February 2004). "Mathematical modelling of the use of macrophages as vehicles for drug delivery to hypoxic tumour sites" (in en). Journal of Theoretical Biology 226 (4): 377–391. doi:10.1016/j.jtbi.2003.09.004. PMID 14759644. Bibcode: 2004JThBi.226..377O. https://linkinghub.elsevier.com/retrieve/pii/S0022519303003412.
- ↑ 14.0 14.1 State, Penn (2019-12-07). "Artificial Cells Engineered to Act More Like the Real Thing" (in en-us). https://scitechdaily.com/artificial-cells-engineered-to-act-more-like-the-real-thing/.
- ↑ 15.0 15.1 15.2 Butler, K. S.; Durfee, P. N.; Theron, C.; Ashley, C. E.; Carnes, E. C.; Brinker, C. J. (2016). "Choose your library affiliation". Small 12 (16): 2173–2185. doi:10.1002/smll.201502119. PMID 26780591. PMC 4964272. https://docs.shib.ncsu.edu/ds/ncsu/WAYF?entityID=https%3a%2f%2fprox.lib.ncsu.edu%2fezproxy%2fshibboleth&return=https%3a%2f%2flogin.prox.lib.ncsu.edu%2fShibboleth.sso%2fDS%3fSAMLDS%3d1%26target%3dezp.2aHR0cHM6Ly9kb2kub3JnLzEwLjEwMDIvc21sbC4yMDE1MDIxMTk%2d. Retrieved 2023-04-07.
- ↑ 16.0 16.1 16.2 16.3 "Enzyme-coated protocells could be used as targeted drug-delivery system" (in en). https://www.europeanpharmaceuticalreview.com/news/106039/enzyme-coated-protocells-could-be-used-as-targeted-drug-delivery-system/.
- ↑ 17.0 17.1 "4 Innovations in Nanoscale Drug Delivery - ASME" (in en). https://www.asme.org/topics-resources/content/4-innovations-in-nanoscale-drug-delivery.
- ↑ 18.0 18.1 Alvarez-Lorenzo, Carmen; Concheiro, Angel (2013-12-01). "Bioinspired drug delivery systems" (in en). Current Opinion in Biotechnology. Chemical biotechnology • Pharmaceutical biotechnology 24 (6): 1167–1173. doi:10.1016/j.copbio.2013.02.013. ISSN 0958-1669. PMID 23465754. https://www.sciencedirect.com/science/article/pii/S095816691300027X.
- ↑ 19.0 19.1 Li Jeon, Noo; Baskaran, Harihara; Dertinger, Stephan K. W.; Whitesides, George M.; Van De Water, Livingston; Toner, Mehmet (2002). "Neutrophil chemotaxis in linear and complex gradients of interleukin-8 formed in a microfabricated device" (in en). Nature Biotechnology 20 (8): 826–830. doi:10.1038/nbt712. ISSN 1546-1696. PMID 12091913. https://www.nature.com/articles/nbt712.
- ↑ "cancer" (in en). 2011-02-02. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cancer.
- ↑ 21.0 21.1 CDCBreastCancer (2021-05-12). "Cancer Treatments" (in en-us). https://www.cdc.gov/cancer/survivors/patients/treatments.htm.
- ↑ (in en) What is an inflammation?. Institute for Quality and Efficiency in Health Care (IQWiG). 2018-02-22. https://www.ncbi.nlm.nih.gov/books/NBK279298/.
- ↑ Lin, Ruyi; Yu, Wenqi; Chen, Xianchun; Gao, Huile (January 2021). "Self‐Propelled Micro/Nanomotors for Tumor Targeting Delivery and Therapy" (in en). Advanced Healthcare Materials 10 (1): 2001212. doi:10.1002/adhm.202001212. ISSN 2192-2640. PMID 32975892. https://onlinelibrary.wiley.com/doi/10.1002/adhm.202001212.
- ↑ "Inflammation: What Is It, Causes, Symptoms & Treatment" (in en). https://my.clevelandclinic.org/health/symptoms/21660-inflammation.
- ↑ Ashley, Carlee E.; Carnes, Eric C.; Phillips, Genevieve K.; Padilla, David; Durfee, Paul N.; Brown, Page A.; Hanna, Tracey N.; Liu, Juewen et al. (May 2011). "The targeted delivery of multicomponent cargos to cancer cells by nanoporous particle-supported lipid bilayers" (in en). Nature Materials 10 (5): 389–397. doi:10.1038/nmat2992. ISSN 1476-4660. PMID 21499315. Bibcode: 2011NatMa..10..389A.
- ↑ "Choose your library affiliation". https://docs.shib.ncsu.edu/ds/ncsu/WAYF?entityID=https%3a%2f%2fprox.lib.ncsu.edu%2fezproxy%2fshibboleth&return=https%3a%2f%2flogin.prox.lib.ncsu.edu%2fShibboleth.sso%2fDS%3fSAMLDS%3d1%26target%3dezp.2aHR0cHM6Ly9wdWJtZWQubmNiaS5ubG0ubmloLmdvdi8xMjk5MDU0Ny8%2d.
- ↑ Kline, Daniel L.; Cliffton, Eugene E. (August 1952). "Lifespan of Leucocytes in Man" (in en). Journal of Applied Physiology 5 (2): 79–84. doi:10.1152/jappl.1952.5.2.79. ISSN 8750-7587. PMID 12990547. http://www.physiology.org/doi/10.1152/jappl.1952.5.2.79.
External links
 |
