Engineering:Negative-pressure wound therapy
| Negative-pressure wound therapy | |
|---|---|
 Application of a vacuum pump using a foam dressing to a wound | |
| Other names | Vacuum assisted closure |
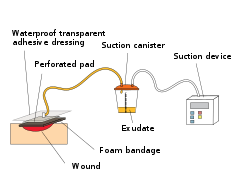
Negative-pressure wound therapy (NPWT), also known as a vacuum assisted closure (VAC), is a therapeutic technique using a suction pump, tubing, and a dressing to remove excess exudate and promote healing in acute or chronic wounds and second- and third-degree burns. The therapy involves the controlled application of sub-atmospheric pressure to the local wound environment using a sealed wound dressing connected to a vacuum pump.[1][2][3] The use of this technique in wound management started in the 1990s and this technique is often recommended for treatment of a range of wounds including dehisced surgical wounds, closed surgical wounds, open abdominal wounds, open fractures, pressure injuries or pressure ulcers, diabetic foot ulcers, venous insufficiency ulcers, some types of skin grafts, burns, sternal wounds. It may also be considered after a clean surgery in a person who is obese.[1][4][5]
NPWT is performed by applying a vacuum through a special sealed dressing. The continued vacuum draws out fluid from the wound and increases blood flow to the area.[1] The vacuum may be applied continuously or intermittently, depending on the type of wound being treated and the clinical objectives. Typically, the dressing is changed two to three times per week.[3] The dressings used for the technique include foam dressings and gauze, sealed with an occlusive dressing intended to contain the vacuum at the wound site.[1] Where NPWT devices allow delivery of fluids, such as saline or antibiotics to irrigate the wound, intermittent removal of used fluid supports the cleaning and drainage of the wound bed.[6]
In 1995, Kinetic Concepts was the first company to have a NPWT product cleared by the US Food and Drug Administration.[7] Following increased use of the technique by hospitals in the US, the procedure was approved for reimbursement by the Centers for Medicare and Medicaid Services in 2001.[8]
Technique

General technique for NPWT is as follows: A dressing or filler material is fitted to the contours of a wound to protect the periwound and the overlying foam or gauze is then sealed with a transparent film.[9] A drainage tube is then connected to the dressing through an opening of the transparent film. Tubing is connected through an opening in the film drape to a canister on the side of a vacuum pump.[10] This turns an open wound into a controlled, closed wound with an airtight seal while removing excess fluid from the wound bed to enhance circulation and remove wound fluids.[11] This creates a moist healing environment and reduces edema.[9][10]
There are four types of dressings used over the wound surface: foam or gauze, a transparent film, and a non-adherent (woven or non-woven) contact layer if necessary. Foam dressings or woven gauze are used to fill open cavity wounds. Foam can be cut to size to fit wounds. Once the wound is filled, then a transparent film is applied over the top to create a seal around the dressing. The tubing is then attached and connected to the pump.
Once the dressing is sealed, the vacuum pump can be set to deliver continuous or intermittent pressures, with levels of pressure depending on the device used,[10][12][13] varying between −200 and −40 mmHg depending on the material used and patient tolerance.[14] Pressure can be applied constantly or intermittently.[10]


The dressing type used depends on the type of wound, clinical objectives and patient. For pain sensitive patients with shallow or irregular wounds, wounds with undermining or explored tracts or tunnels, gauze may be used, while foam may be cut easily to fit a patient's wound that has a regular contour and perform better when aggressive granulation formation and wound contraction is the desired goal.[15]
Contraindications
Contraindications for NPWT use include:[16]
- Malignancy in the wound
- Untreated osteomyelitis
- Non enteric and unexplored fistulas
- Necrotic tissue with eschar present
- Exposed blood vessels, anastomotic sites, organs and nerves in the periwound area (must avoid direct foam contact with these structures)[17]
Effectiveness
Negative pressure wound therapy is usually used with chronic wounds or wounds that are expected to present difficulties while healing (such as those associated with diabetes).[3] Negative pressure wound therapy is approved by the FDA and numerous randomized controlled trials have been conducted on this technique, however, the evidence supporting how effective NPWT is compared to standard wound care dressings is not clear.[1] Low-level evidence indicates that there may be a lower risk of death and less surgical site infections associated with NPWT compared to standard dressing care, however there may not be a difference in the risk of wound reopening when comparing the two approaches.[1] NPWT may increase the risk of skin blistering compared to standard wound care.[1] NPWT may be a more cost effective approach for closing wounds following a caesarean section in women who are obese, however, NPWT is not likely as cost effective for closing wounds associated with fracture surgeries. It is not clear if NPWT is cost effective for closing wounds associated with other types of surgery.[1] NPWT has been used to treat non-trauma patients after abdominal surgery.[18] Non-trauma patients are people who might need surgery for conditions such as abdominal infections or cancer. However, it is still not clear how safe and effective NPWT is for treating non-trauma patients with open abdomens.[18]
For treating diabetic ulcers of the feet, "consistent evidence of the benefit of NPWT" in the treatment of diabetic ulcers of the feet has been reported.[19] Results for bedsores were conflicting and research on mixed wounds was of poor quality, but promising.[19] There is no evidence of increased significant complications.[19] The review concluded "There is now sufficient evidence to show that NPWT is safe, and will accelerate healing, to justify its use in the treatment of diabetes-associated chronic leg wounds. There is also evidence, though of poor quality, to suggest that healing of other wounds may also be accelerated."[19]
Mechanism
The use of NPWT to enhance wound healing is thought to be by removing excess extracellular fluid and decreasing tissue edema, which leads to increased blood flow and stabilization of the wound environment.[citation needed] A reduction in systemic (e.g. interleukins, monocytes) and local mediators of inflammation has been demonstrated in experimental models, while decreased matrix metalloproteinase activity and bacterial burden have been documented clinically.[citation needed] In vivo, NPWT has been shown to increase fibroblast proliferation and migration, collagen organization, and to increase the expression of vascular endothelial growth factor and fibroblast growth factor-2, thereby enhancing wound healing.[20]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 "Negative pressure wound therapy for surgical wounds healing by primary closure". The Cochrane Database of Systematic Reviews 2022 (4): CD009261. April 2022. doi:10.1002/14651858.CD009261.pub7. PMID 35471497.
- ↑ "Negative pressure wound therapy: Unusual and innovative applications". OPUS 12 Scientist 2 (3): 15–29. 2008. http://journal.opus12.org/o12-ojs/ojs-2.1.1/index.php/o12sci/article/view/240. Retrieved 2 March 2015.
- ↑ 3.0 3.1 3.2 "Best treatment of nonhealing and problematic wounds". JAAPA 22 (8): 46, 48. August 2009. doi:10.1097/01720610-200908000-00013. PMID 19725415.
- ↑ "Guidelines for using negative pressure wound therapy". Advances in Skin & Wound Care 14 (6): 314–22; quiz 324–5. 2001. doi:10.1097/00129334-200111000-00015. PMID 11794443.
- ↑ "Laparostomy management using the ABThera™ open abdomen negative pressure therapy system in a grade IV open abdomen secondary to acute pancreatitis". International Wound Journal 10 (2): 138–144. April 2013. doi:10.1111/j.1742-481X.2012.00953.x. PMID 22487377.
- ↑ "Instillationsvakuumversiegelung — ein erster Erfahrungsbericht" (in German). Vielfalt und Einheit der Chirurgie Humanität und Wissenschaft. 115. 1998. 1197–1199. doi:10.1007/978-3-642-45774-6_279. ISBN 978-3-540-65144-4.
- ↑ "Vacuum Assisted Closure Wound Therapy Cleared for Partial Thickness Burns". Reuters Health Medical News. 27 January 2003.[verification needed]
- ↑ "Effective wound care requires look at total patient picture". Healthcare Purchasing News 27 (1): 32. 2003. ISSN 0279-4799. http://findarticles.com/p/articles/mi_m0BPC/is_1_27/ai_96950328/.
- ↑ 9.0 9.1 "The Challenges of Negative Pressure Wound Therapy in Clinical Practice | Today's Wound Clinic". http://www.todayswoundclinic.com/NPWT.
- ↑ 10.0 10.1 10.2 10.3 "Vacuum-assisted closure". Nursing Times 97 (35): 51–52. 2001. PMID 11957602. https://www.nursingtimes.net/clinical-archive/tissue-viability/vacuum-assisted-closure-30-08-2001/.
- ↑ "Advances in healing chronic wounds". The Ithaca Journal (Ithaca, NY): p. 10A. 19 July 2001.
- ↑ "Negative pressure wound therapy options promote patient care". Biomechanics: p. 49. 1 September 2005. http://www.biomech.com/full_article_printfriendly/?ArticleID=628&month=9&year=2005&fromdb=archives.
- ↑ "Multiple approaches offer negative pressure options". Biomechanics. February 2009. http://www.biomech.com/full_article_printfriendly/?ArticleID=215&month=4&year=2007&fromdb=archives.
- ↑ "Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation". Annals of Plastic Surgery 38 (6): 553–562. June 1997. doi:10.1097/00000637-199706000-00001. PMID 9188970.
- ↑ "Options in negative pressure wound therapy: five case studies". Journal of Wound, Ostomy, and Continence Nursing 36 (2): 202–211. 2009. doi:10.1097/01.WON.0000347664.10217.2e. PMID 19287271.
- ↑ KCI clinical guidelines
- ↑ "V.A.C. Therapy Indications and Contraindications". http://www.activactherapy.com/cs/Satellite?c=KCI_General_C&childpagename=KCI1/KCILayout&cid=1229624973260&pagename=KCI1Wrapper.
- ↑ 18.0 18.1 "Negative pressure wound therapy for managing the open abdomen in non-trauma patients". The Cochrane Database of Systematic Reviews 2022 (5): CD013710. May 2022. doi:10.1002/14651858.CD013710.pub2. PMID 35514120.
- ↑ 19.0 19.1 19.2 19.3 "The clinical effectiveness of negative pressure wound therapy: a systematic review". Journal of Wound Care 19 (11): 490–495. November 2010. doi:10.12968/jowc.2010.19.11.79697. PMID 21135797. http://www.journalofwoundcare.com/cgi-bin/go.pl/library/article.html?uid=79697;article=JWC_19_11_490. Retrieved 6 June 2011.
- ↑ "Histopathological study of chronic wounds modulated by intermittent negative pressure therapy under limited access dressing" (in en-us). Plastic and Aesthetic Research 2 (5): 272–276. 15 September 2015. doi:10.4103/2347-9264.156993.
 |
