Medicine:Intracoronary optical coherence tomography
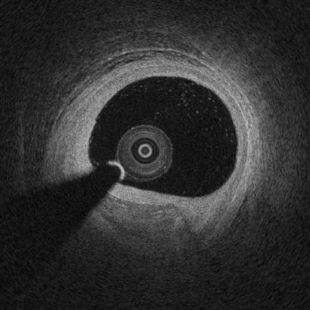
Intracoronary optical coherence tomography (OCT) (or, more generally, intravascular optical coherence tomography) is a catheter-based imaging application of optical coherence tomography. Currently prospective trials demonstrate OCT alters morbidity and/or mortality in coronary stenting as discussed below.
Intracoronary OCT creates images at a resolution of approximately 15 micro-meters, an order of magnitude improved resolution with respect to intravascular ultrasound and X-ray coronary angiogram.[1]
Theory
OCT is analogous to ultrasound, measuring the backreflection of infrared light rather than sound. The time for light to be relfected back from the tissue under inspection is used to measure distances. The backreflection intensity with depth plots the structure of the tissue. An A-scan (a 1 dimension scan as opposed to a 2 dimensioal B-scan) [clarification needed] can be taken (1-dimension) or the beam can scanned to produce two and three dimensional data sets. Due the high speed associated with light propagation, the backreflection time can not be measured directly, but is instead measured using interferometry.[2]
OCT is measured using either time domain (TD-OCT) and frequency domain techniques (SS-OCT/FD-OCT/Spectral OCT). TD-OCT can be considered like ultrasound, directly measuring the time for the photon make the round-trip from the source to the tissue and back to the detector. Frequency domain OCT collects all the frequencies from an A-scan and ascertains backreflection depth using Fourier analysis.[3] Time domain and frequency domain OCT both existed by 1981. TD-OCT was initially used in cardiology but frame rates at the time were too slow. The ultimate maximum acquisition rate for TD-OCT remains unknown as work in this field stopped before later advances in data acquisition techniques were available. FD-OCT is faster but is believed to have lower dynamic range, which can effect imaging quality such as penetration.[3] Some groups dispute this, though they appear to be talking about SNR and not dynamic range.[4]
OCT needs to image at 1300 nm in cardiovascular tissue, but those could damage the eye. On the other hand, ophthalmologic systems image at 830 nm, which would only image a few hundred micron in arteries. The eye effectively has no scattering, but imaging to the retina occurs over a range of several cenitmeters, so water absorption becomes significant. The coronary application needs a wavelength with low scattering and preferably low absorption (though imaging is only over a range of a few millimeters). The light also had to have a broad bandwidth, significant power at high acquisition rates, and a Gaussian spectrum.[5]
Cardiological applications
In 1993, after OCT had been unsuccessful in imaging non-transparent tissue, Mark Brezinski proposed imaging at 1300 nm rather than 830 nm used in the eye (after analyzing a 1989 scattering/absorption study by Parsa et al. in liver).[6] The goal was to image vulnerable plaque (where better than 20 µm resolution is needed based on histology and stress studies) and guide stent placement. A collaboration was established between Brezinski and James Fujimoto and they successfully imaged artery as well as other scattering tissue in 1993 with students Micheal Hee and postdoctoral fellow Joseph Izatt generated the first images with Brezinski (initially chicken and fish).[2] The first demonstration of endoscopic OCT was reported in 1997, by researchers in James Fujimoto laboratory at Massachusetts Institute of Technology and the Mark Brezinski Laboratory at Massachusetts General Hospital. Other team members include pathologist James Southern MD, PhD, student Guillermo James Tearney, student Micheal Hee, post-doctoral fellow Joe Izatt, and post-doctoral fellow Brett Bouma. The superior resolution to IVUS was demonstrated.[7] The first TD-OCT imaging catheter and system was commercialized by LightLab Imaging, Inc., a company based in Massachusetts formed in 1997 by Fujimoto, Swanson, and Brezinski. Technical advances over the ophthamologic system were needed beyond wavelength, particularly the catheter and acquisition rate. The most important technical advance for cardiology and other nontransparent tissue was likely the catheter/endoscope. The fiber optic catheter/endoscope required rapid alignment of two optical fibers with 8 µm cores (one rotating) across free space. The first intravascular imaging was in rabbit but blood needed to be pushed out of the field in 1998.[8] Index matching was proposed to make the red cells invisible to infrared light.[9] The initial few years of the millineum did not see in vivo human imaging as only a few groups were capable. The Brezinski and Fujimoto groups could not because of COI, owning Lightlab and IP. Lightlab had not moved this forward. The Tearney and Bouma group finally achieved it in 2003 looking at stents.[10] The last two decade have seen consensus groups and registries but a lack of prospective trials with MACE endpoints for unclear reasons.[11] Part was related to only several groups having access to cardiovascular systems early (Brezinski at Harvard, Fujimoto at MIT, LightLab, and former MIT trainees at MGH (Bouma/Tearney), with at least the first two having COI for intravascular studies. A study in 2012 concluded IVUS led to better stent expansion, but experience with OCT may have been limited.[12] This conclusion is supported by more recent studies.[13] A study in 2015 showed OCT influenced physician decisions, but it is unclear if their changed decision was for the better or worse[11] Studies on plaque healing had conflicting results, though not surprising being primarily registry studies with little basic work on what a healed plaque (or even thrombus) appear on OCT.[14][15] Some authors have found these registry data is core length in ACS patients.[16] A major change occurred in 2023 with prospective trials, as Abbott acquiring LightLab in 2017. In 2023, after double blind prospective trails were ultimately performed demonstrating morbidity and mortality benefits "Among patients with complex coronary-artery bifurcation lesions, OCT-guided PCI was associated with a lower incidence of MACE at 2 years than angiography-guided PCI."[17] Several other studies are expected out in 2023.
Data published in late 2016 showed that approximately 100,000 intracoronary optical coherence tomography procedures are performed every year, and its adoption is rapidly growing at a rate of ~ 20% every year.[citation needed]
Assessment of artery lumen morphology is the cornerstone of intravascular imaging criteria to evaluate disease severity and guide intervention. The high-resolution of OCT imaging allows to assess with high accuracy vessel lumen area, wall microstructure, intracoronary stent apposition and expansion. OCT has an improved ability with respect to intravascular ultrasound to penetrate and delineate calcium in the vessel wall that makes it well suited to guide complex interventional strategies in vessels with superficial calcification. OCT has the capability of visualize coronary plaque erosion and fibrotic caps overlying atheromas.[2]
Technology
The technology of most interest to clinicians and non-physicians are the catheter, technology for faster imaging (SS-OCT versus TD-OCT), the light source, and the potential for a guidewire. The most critical technological advance (besides identifying the optimal wavelength) was the catheter. The fiber optic catheter/endoscope required rapid alignment of two optical fibers with 8 µm cores (one rotating) across free space. The fiber itself is 120 microns so can be made into a guidewire unlike IVUS. The distal end has a focusing component (GRIN lens typically) and light directing component (usually prism). The fiber is fragile and needs external casing as a recent study using a Lightlab catheter in a joint had a high breakage rate.[18]
State-of-the-art intracoronary optical coherence tomography uses a swept-source laser to make OCT images at high-speed (i.e., approximately 80,000 kHz - A-scan lines per second) to complete acquisition of a 3D OCT volume of coronary segments in a few-seconds.[19] The first intravascular FD-OCT was introduced to the market in 2009 (EU and Asia) and in 2012 (US). In 2018, two intracoronary OCT catheters are clinically available for use in the coronary arteries, having a size in diameter between 2.4F and 2.7F. [citation needed]
The axial resolution of state-of-the-art commercial systems is less than 20 micrometers, which is decoupled from the catheter lateral resolution. The highest resolution of OCT allows for the in vivo imaging of vessel microstructural features at an unprecedented level, enabling visualization of vessel wall atherosclerosis, pathology, and interaction with therapeutic devices at a microscopic level.[20][citation needed]
Basic research
The field, and current clinical trials, are limited by the need for more basic research, particularly characterizing plaque necrotic cores. A core to much of the basic research done and to be done is micron scale matching of OCT images to histopathology, covered in the Optical Coherence Tomography: Principles and Applications chapter 12.[5] There are only a small number of groups which have this capability. For the retina, micron scale matching was not performed but as prospective trials are being finally considered, more refined interpretation of images is needed.[21] Micron scale matching was performed in the first OCT artery paper, where pathologist James Southern MD,PhD of MGH played a major role.[2]
Safety
Safety of intravascular imaging, including intracoronary OCT and intravascular ultrasound, has been investigated by several studies. Recent clinical trials reported a very low rate of self-limiting, minor complications on over 3,000 patients where in all cases no harm or prolongation of hospital stay was observed. Intracoronary optical coherence tomography was demonstrated to be safe among heterogeneous groups of patients presenting varying clinical setting.[22]
See also
References
- ↑ "Intracoronary optical coherence tomography: a comprehensive review clinical and research applications". JACC. Cardiovascular Interventions 2 (11): 1035–1046. November 2009. doi:10.1016/j.jcin.2009.06.019. PMID 19926041.
- ↑ 2.0 2.1 2.2 2.3 "Optical coherence tomography for optical biopsy. Properties and demonstration of vascular pathology". Circulation 93 (6): 1206–1213. March 1996. doi:10.1161/01.CIR.93.6.1206. PMID 8653843.
- ↑ 3.0 3.1 "Experimental confirmation of potential swept source optical coherence tomography performance limitations". Applied Optics 47 (33): 6151–6158. November 2008. doi:10.1364/AO.47.006151. PMID 19023378. Bibcode: 2008ApOpt..47.6151Z.
- ↑ "Sensitivity advantage of swept source and Fourier domain optical coherence tomography". Optics Express 11 (18): 2183–2189. September 2003. doi:10.1364/OE.11.002183. PMID 19466106. Bibcode: 2003OExpr..11.2183C.
- ↑ 5.0 5.1 Optical Coherence Tomography: Principles and Applications. Amsterdam, Boston: Academic Press. 2006. ISBN 978-0-12-133570-0.
- ↑ "Optical properties of rat liver between 350 and 2200 nm" (in EN). Applied Optics 28 (12): 2325–2330. June 1989. doi:10.1364/AO.28.002325. PMID 20555519. Bibcode: 1989ApOpt..28.2325P.
- ↑ "Assessing atherosclerotic plaque morphology: comparison of optical coherence tomography and high frequency intravascular ultrasound". Heart 77 (5): 397–403. May 1997. doi:10.1136/hrt.77.5.397. PMID 9196405.
- ↑ "High resolution in vivo intra-arterial imaging with optical coherence tomography". Heart 82 (2): 128–133. August 1999. doi:10.1136/hrt.82.2.128. PMID 10409522.
- ↑ "Index matching to improve optical coherence tomography imaging through blood". Circulation 103 (15): 1999–2003. April 2001. doi:10.1161/01.CIR.103.15.1999. PMID 11306530.
- ↑ "Evaluation of intracoronary stenting by intravascular optical coherence tomography". Heart 89 (3): 317–320. March 2003. doi:10.1136/heart.89.3.317. PMID 12591841.
- ↑ 11.0 11.1 "Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study". European Heart Journal 36 (47): 3346–3355. December 2015. doi:10.1093/eurheartj/ehv367. PMID 26242713.
- ↑ "Impact of frequency-domain optical coherence tomography guidance for optimal coronary stent implantation in comparison with intravascular ultrasound guidance". Circulation. Cardiovascular Interventions 5 (2): 193–201. April 2012. doi:10.1161/CIRCINTERVENTIONS.111.965111. PMID 22456026.
- ↑ Wijns, William; Shite, Junya; Jones, Michael R.; Lee, Stephen W.-L.; Price, Matthew J.; Fabbiocchi, Franco; Barbato, Emanuele; Akasaka, Takashi et al. (2015-12-14). "Optical coherence tomography imaging during percutaneous coronary intervention impacts physician decision-making: ILUMIEN I study" (in en). European Heart Journal 36 (47): 3346–3355. doi:10.1093/eurheartj/ehv367. ISSN 0195-668X. PMID 26242713.
- ↑ "Coronary Atherosclerotic Phenotype and Plaque Healing in Patients With Recurrent Acute Coronary Syndromes Compared With Patients With Long-term Clinical Stability: An In Vivo Optical Coherence Tomography Study". JAMA Cardiology 4 (4): 321–329. April 2019. doi:10.1001/jamacardio.2019.0275. PMID 30865212.
- ↑ "Association between non-culprit healed plaque and plaque progression in acute coronary syndrome patients: an optical coherence tomography study". Journal of Geriatric Cardiology 18 (8): 631–644. August 2021. doi:10.11909/j.issn.1671-5411.2021.08.001. PMID 34527029.
- ↑ "Comparing the Risk Factors of Plaque Rupture and Failed Plaque Healing in Acute Coronary Syndrome". JAMA Cardiology 4 (4): 329–331. April 2019. doi:10.1001/jamacardio.2019.0312. PMID 30865209.
- ↑ "OCT or Angiography Guidance for PCI in Complex Bifurcation Lesions". The New England Journal of Medicine 389 (16): 1477–1487. October 2023. doi:10.1056/NEJMoa2307770. PMID 37634149.
- ↑ Martin, S.; Rashidifard, C.; Norris, D.; Goncalves, A.; Vercollone, C.; Brezinski, M.E. (December 2022). "Minimally Invasive Polarization Sensitive Optical Coherence Tomography (PS-OCT) for assessing Pre-OA, a pilot study on technical feasibility". Osteoarthritis and Cartilage Open 4 (4): 100313. doi:10.1016/j.ocarto.2022.100313. ISSN 2665-9131. PMID 36263247. PMC 9576017. https://doi.org/10.1016/j.ocarto.2022.100313.
- ↑ "Pulsed-source and swept-source spectral-domain optical coherence tomography with reduced motion artifacts". Optics Express 12 (23): 5614–5624. November 2004. doi:10.1364/opex.12.005614. PMID 19488195. Bibcode: 2004OExpr..12.5614Y.
- ↑ Brezinski, Mark E.; Tearney, Guillermo J.; Bouma, Brett E.; Izatt, Joseph A.; Hee, Michael R.; Swanson, Eric A.; Southern, James F.; Fujimoto, James G. (1996-03-15). "Optical Coherence Tomography for Optical Biopsy: Properties and Demonstration of Vascular Pathology" (in en). Circulation 93 (6): 1206–1213. doi:10.1161/01.CIR.93.6.1206. ISSN 0009-7322. PMID 8653843. https://www.ahajournals.org/doi/10.1161/01.CIR.93.6.1206.
- ↑ "OCT Signs of Early Atrophy in Age-Related Macular Degeneration: Interreader Agreement: Classification of Atrophy Meetings Report 6". Ophthalmology. Retina 6 (1): 4–14. January 2022. doi:10.1016/j.oret.2021.03.008. PMID 33766801.
- ↑ "Safety of optical coherence tomography in daily practice: a comparison with intravascular ultrasound". European Heart Journal. Cardiovascular Imaging 18 (4): 467–474. April 2017. doi:10.1093/ehjci/jew037. PMID 26992420.
 |