Medicine:Negative pressure ventilator
A negative pressure ventilator (NPV) is a type of mechanical ventilator that stimulates an ill person's breathing by periodically applying negative air pressure to their body to expand and contract the chest cavity.[1][2][3][4][5][6]
Description
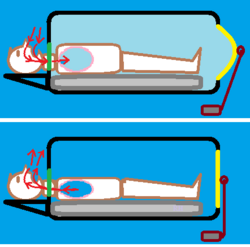
In most NPVs (such as the iron lung in the diagram), the negative pressure is applied to the patient's torso, or entire body below the neck, to cause their chest to expand, expanding their lungs, drawing air into the patient's lungs through their airway, assisting (or forcing) inhalation. When negative pressure is released, the chest naturally contracts, compressing the lungs, causing exhalation. In some cases, positive external pressure may be applied to the torso to further stimulate exhalation.[1][2][3][4][5][6]
Another form of NPV device (such as the Pulmotor) is placed at the patient's airway, and alternates negative pressure with positive pressure to pump air into their lungs (inhale under positive pressure), then suck it back out (exhale under negative pressure).[2][7][8][9][10]
Usage
Negative pressure ventilators, while widely used in the early-to-mid 20th Century (particularly for victims of the Polio epidemics), are now largely replaced by Positive-pressure airway ventilators, which force air (or oxygen) directly into the patient's airway.[1][2][3][4][5]
However, researchers and clinicians still find some uses for NPVs, owing to their specific advantages.[1][2]
Research and developments in artificial ventilation, both negative-pressure and positive-pressure, result in evolving assessments of the benefits and hazards of negative-pressure ventilators (NPVs). Different researchers and clinicians have made varying assessments, over time, about the primary positive and negative aspects of NPVs. A sampling includes:
Advantages
Generally, NPVs are best with patients who have neuromuscular diseases, but normal lung compliance (a measure of the lungs' ability to expand and contract).(1988: Grum & Morganroth, Journal of Intensive Care Medicine)[2] They are effective for various conditions, especially neuromuscular and skeletal disorders, particularly for long-term night-time ventilation.[1] They are effective in patients who have severe respiratory acidosis, impaired consciousness, are unable to tolerate a facial mask (due to facial deformity, or claustrophobia, or excess airway secretions), and in children.[11] Continuous external negative pressure ventilation (CENPV) was found in a 2015 study to "[improve] oxygenation under [a greater number of] physiological conditions", concurrent with lower "airway," "transpulmonary," and "intra-abdominal" pressures, than experienced with continuous positive pressure ventilation (CPPV), in study of Adult respiratory distress syndrome (ARDS) patients, possibly reducing high ARDS mortality.[12]
Disadvantages
NPVs do not work well if patient's lung compliance is decreased, or their lung resistance is increased.[2] They result in a greater vulnerability of the airway to aspiration, such as inhalation of vomit or swallowed liquids, than with intermittent positive pressure ventilation.[1] They exacerbate obstructive sleep apnea. The device is not portable and its installation may be difficult. Patients must sleep in a supine position.[13]
Types of NPVs
There are several types of NPVs, including:[1][2][3][4][5]
- Iron lung, also known as a tank ventilator, Drinker tank or Emerson tank;[1][2][3][4][6]
- Cuirass ventilator, also known as a chest shell, turtle shell or tortoise shell;[1][2][3][4]
- exovent;[14][15]
- jacket ventilator, also known as a poncho or raincoat ventilator;[1][2][12]
- Pulmotor.[7][8][9][10]
Iron lung
The iron lung, also known as the tank ventilator, Drinker tank or Emerson tank, was the first common pure-NPV device when it was developed in the 1920s by Drinker, Shaw and Mason. It is a large, sealed horizontal cylinder (or "tank") in which the patient lies, with their head protruding from a sealed opening at one end of the tank. An air pump or flexible diaphragm (usually motor-driven) varies the air pressure inside the tank, in continuous alternations, lowering and raising the air pressure in the cylinder. This causes the patient's chest to rise and fall, stimulating inhalation and exhalation through the patient's nose and mouth (which are outside the cylinder, exposed to ambient air pressure).[1][2][3][4][6]
Cuirass ventilator
The cuirass ventilator, also known as the chest shell, turtle shell or tortoise shell, is a more compact variation of the iron lung which only encloses the patient's torso and is sealed around their neck and waist, and depressurized and repressurized by an external pump or portable ventilator.[1][2][3][4][16]
Exovent
The exovent is a modern device similar to the cuirass ventilator, but developed in 2020, in response to the COVID-19 pandemic.[14][15]
Jacket ventilator
The jacket ventilator, also known as a poncho or raincoat ventilator, is a lighter version of the iron lung or the cuirass ventilator, constructed of an airtight material (such as plastic or rubber) arranged over a light metal or plastic frame, or screen, and depressurized and repressurized by a portable ventilator.[1][2][12][17]
Positive-and-negative pressure ventilator
Pulmotor
The Pulmotor is a device developed in the early 1900s which was the forerunner of modern mechanical ventilators. It used pressure from a tank of compressed oxygen to operate a valve system that alternately forced air into and out of a person's airway, using alternating positive and negative air pressure. Although portable, and able to be used by lay persons and non-medical emergency responders, some medical personnel criticized it as dangerous (in part due to the risks of barotrauma or vomiting) and inefficient.[7][8][9][10][16]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Shneerson, Dr. John M., Newmarket General Hospital, (Newmarket, Suffolk, U.K.), "Non-invasive and domiciliary ventilation: negative pressure techniques," #5 of series "Assisted ventilation" in Thorax, 1991;46: pp.131-135, retrieved April 12, 2020
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 Grum, Cyril M., MD, and Melvin L. Morganroth, MD, "Initiating Mechanical Ventilation," in Intensive Care Medicine 1988;3:6-20, retrieved April 12, 2020
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Rockoff, Mark, M.D., "The Iron Lung and Polio,", video (8 minutes), January 11, 2016, OPENPediatrics and Boston Children's Hospital on YouTube, retrieved April 11, 2020 (historical background and images, explanatory diagrams, and live demonstrations)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 "The Iron Lung," Science Museum Group, Kensington, London, England, U.K., retrieved April 11, 2020
- ↑ 5.0 5.1 5.2 5.3 "How Does Iron Lung Work?: Polio Survivor, 82, Among Last to Use Breathing Equipment," August 21, 2018, Newsweek retrieved April 11, 2020
- ↑ 6.0 6.1 6.2 6.3 Jackson, Christopher D., MD, Dept. of Internal Medicine, and Muthiah P Muthiah, MD, FCCP, D-ABSM, Assoc. Prof. of Medicine, Div. of Pulmonary / Critical Care / Sleep Medicine, Univ. of Tennessee College of Medicine-Memphis, et.al., "What is the background of the iron lung form of mechanical ventilation?," April 11, 2019, Medscape, retrieved April 12, 2020 (short summary of iron history and technology, with photo)
- ↑ 7.0 7.1 7.2 Bottrell, John, "1907: The first mechanical ventilator: The Pulmotor," April 19, 2017, Asthma History blog, retrieved April 12, 2020
- ↑ 8.0 8.1 8.2 "Draeger Pulmotor", Wood Library-Museum of Anesthesiology
- ↑ 9.0 9.1 9.2 "The Return of the Pulmotor as a 'Resuscitator': A Back-Step toward the Death of Thousands," by Yandell Henderson, December 1943, Science.
- ↑ 10.0 10.1 10.2 Bahns, Ernst, It began with the Pulmotor: One Hundred Years of Artificial Ventilation, Dräger Medical AG & Co. KG, Lübeck, Germany (original manufacturers of the Pulmotor).
- ↑ Corrado, A.; Gorini, M.: "Negative-pressure ventilation: is there still a role?," European Respiratory Journal 2002, 20: pp.187-197;, also in PDF retrieved April 17, 2020
- ↑ 12.0 12.1 12.2 Raymondos, Konstantinos; Jörg Ahrens; Ulrich Molitoris: "Combined Negative- and Positive-Pressure Ventilation for the Treatment of ARDS", in Case Reports in Critical Care 2015; 2015: 714902. Published online July 28, 2015, from NCBI, National Institutes of Health, retrieved April 12, 2020.
- ↑ Walkey, Allan M.D. and Ross Summer M.D., "Negative pressure" in "E. Noninvasive Mechanical Ventilation," in Boston Medical Center ICU Manual, 2008, Boston University, p.17, retrieved April 12, 2020.
- ↑ 14.0 14.1 "Modern iron lung designed to address ventilator shortage,", April 06, 2020, New Atlas, retrieved April 11, 2020 (note detailed reader comment, , April 7, 2020, by Christopher Smith, with clinical application details.)
- ↑ 15.0 15.1 "The 'iron lung' and the modern 'ventilation'," Oxy.gen, retrieved April 11, 2020
- ↑ 16.0 16.1 Matioc, Adrian A., M.D., University of Wisconsin School of Medicine & Public Health, William S. Middleton Memorial Veterans Hospital, Madison, Wisconsin, "Early Positive and Alternate Pressure Machines" in "An Anesthesiologist’s Perspective on the History of Basic Airway Management: The 'Progressive' Era, 1904 to 1960," submitted May 27, 2017, published February 2018, Anesthesiology, Vol. 128, No 2
- ↑ "Poncho,"[yes|permanent dead link|dead link}}] by medical device manufacturer Dima Italia S.r.l. of Bologna, Italy (picture of jacket ventilator ("poncho"), and other information.), retrieved April 12, 2020
External links
- It began with the Pulmotor: One Hundred Years of Artificial Ventilation by Ernst Bahns, published by Dräger Medical AG & Co. KG, Lübeck, Germany (original manufacturers of the Pulmotor, and many other ventilation items, to the present day) (a lengthy, illustrated history of the development of artificial ventilation, interwoven with the publishers' own apparently self-promotional corporate history).
 |
