Medicine:Sézary disease
| Sézary disease | |
|---|---|
| Other names | Sézary's disease, Sézary('s) syndrome |
 | |
| The bright red rash of Sezary syndrome | |
| Pronunciation | |
| Specialty | Oncology, dermatology |
Sézary disease, or Sézary syndrome,[1] is a type of cutaneous T-cell lymphoma that was first described by Albert Sézary.[2] The affected T cells, known as Sézary's cells or Lutzner cells, have pathological quantities of mucopolysaccharides. Sézary disease is sometimes considered a late stage of mycosis fungoides with lymphadenopathy.[3][4]
Signs and symptoms
Sézary disease and mycosis fungoides are cutaneous T-cell lymphomas having a primary manifestation in the skin.[5] The disease's origin is a peripheral CD4+ T-lymphocyte,[3] although rarer CD8+/CD4- cases have been observed.[3] Epidermotropism (lymphocytes residing in the epidermis)[6] by neoplastic CD4+ lymphocytes with the formation of Pautrier's microabscesses is the hallmark sign of the disease. Although the condition can affect people of all ages, it is commonly diagnosed in adults over age 60.[7][3] The dominant signs and symptoms of the disease are:
- Generalized erythroderma– redness of the skin[3]
- Lymphadenopathy – swollen, enlarged lymph nodes[3]
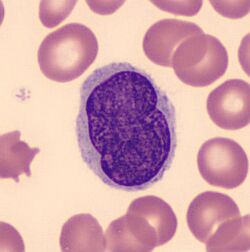
- Atypical T cells – malignant lymphocytes known as "Sézary cells" seen in the peripheral blood with typical cerebriform nuclei (brain-shaped, convoluted nuclei)[8][3]
- Hepatosplenomegaly– enlarged liver and spleen[9]
- Palmoplantar keratoderma – thickening of the palms of the hands, and soles of the feet[10][11]
Diagnosis
Those who have Sézary disease often present skin lesions that do not heal with normal medication.[12] A blood test generally reveals any change in the levels of lymphocytes in the blood, which is often associated with a cutaneous T-cell lymphoma.[12] Finally, a biopsy of a skin lesion can be performed to rule out any other causes.[12]
The immunohistochemical features are very similar to those presented in mycosis fungoides except for the following differences:[13]
- More monotonous cellular infiltrates (large, clustered atypical pagetoid cells) in Sézary syndrome
- Sometimes absent epidermotropism
- Increased lymph node involvement with infiltrates of Sézary syndrome.
Treatment
Treatment typically includes some combination of photodynamic therapy, radiation therapy, chemotherapy, and biologic therapy.[14]
Treatments are often used in combination with phototherapy and chemotherapy, though pure chemotherapy is rarely used today.[3] No single treatment type has revealed clear-cut benefits in comparison to others, treatment for all cases remains problematic.[15]
Radiation therapy
A number of types of radiation therapy may be used including total skin electron therapy.[16] While this therapy does not generally result in systemic toxic effects it can produce side effects involving the skin.[16] It is only available at a few institutions.[16]
Chemotherapy
Romidepsin, vorinostat and a few others are a second-line drug for cutaneous T-cell lymphoma.[17] Mogamulizumab has been approved in Japan[18] and the United States.[19]
Epidemiology
In the Western population, there are around 3 cases of Sézary syndrome per 1,000,000 people.[3] Sézary disease is more common in males with a ratio of 2:1,[3] and the mean age of diagnosis is between 55 and 60 years of age.[3][9]
See also
- List of cutaneous conditions
References
- ↑ Reference, Genetics Home. "Sézary syndrome" (in en). https://ghr.nlm.nih.gov/condition/sezary-syndrome.
- ↑ Sézary's cell at Who Named It?
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Cuneo, A; Castoldi, GL (2005). "Mycosis fungoidses/Sezary's syndrome". Atlas Genet Cytogenet Oncol Haematol. 9 (3): 242–243. http://atlasgeneticsoncology.org/Anomalies/MycosFungID2039.html. Retrieved 2008-02-15.
- ↑ "Recurring Structural Chromosome Abnormalities in Peripheral Blood Lymphocytes of Patients With Mycosis Fungoides/Sézary Syndrome". Blood 89 (9): 3371–7. May 1997. doi:10.1182/blood.V89.9.3371. PMID 9129044. http://www.bloodjournal.org/content/89/9/3371.full.
- ↑ Cerroni, Lorenzo; Kevin Gatter; Helmut Kerl (2005). An illustrated guide to Skin Lymphomas. Malden, Massachusetts: Blackwell Publishing. pp. 39. ISBN 978-1-4051-1376-2.
- ↑ Mutasim, Diya F. (2015). "What is Dermatitis with Epidermotropism?" (in en). Practical Skin Pathology. Springer International Publishing. pp. 37–39. doi:10.1007/978-3-319-14729-1_8. ISBN 978-3-319-14728-4.
- ↑ "Sezary syndrome". https://rarediseases.info.nih.gov/diseases/7629/sezary-syndrome.
- ↑ Park, HS; McIntosh, L; Braschi-Amirfarzan, M; Shinagare, AB; Krajewski, KM (January 2017). "T-Cell Non-Hodgkin Lymphomas: Spectrum of Disease and the Role of Imaging in the Management of Common Subtypes.". Korean Journal of Radiology 18 (1): 71–83. doi:10.3348/kjr.2017.18.1.71. PMID 28096719.
- ↑ 9.0 9.1 Lorincz, A. I.. "Sezary syndrome". http://www.gpnotebook.co.uk/simplepage.cfm?ID=584056846.
- ↑ Fragkos, Konstantinos C. (2017). "Plantar keratoderma of Sézary syndrome" (in en). Clinical Case Reports 5 (10): 1726–1727. doi:10.1002/ccr3.1168. ISSN 2050-0904. PMID 29026585.
- ↑ Martin, Stephanie J.; Duvic, Madeleine (2012-10-01). "Prevalence and treatment of palmoplantar keratoderma and tinea pedis in patients with Sézary syndrome" (in en). International Journal of Dermatology 51 (10): 1195–1198. doi:10.1111/j.1365-4632.2011.05204.x. ISSN 1365-4632. PMID 22994666.
- ↑ 12.0 12.1 12.2 "Diagnosis". http://www.sezary.com/sezary-syndrome-diagnosis.html.
- ↑ Beigi, Pooya Khan Mohammad (2017). "Diagnosis and Management" (in en). Clinician's Guide to Mycosis Fungoides. 35. Springer International Publishing. 13–18. doi:10.1007/978-3-319-47907-1_4. ISBN 9783319479064.
- ↑ "Mycosis Fungoides (Including Sézary Syndrome) Treatment" (in en). 7 September 2017. https://www.cancer.gov/types/lymphoma/patient/mycosis-fungoides-treatment-pdq#link/_50.
- ↑ Cerroni, Lorenzo; Kevin Gatter; Helmut Kerl (2005). An illustrated guide to Skin Lymphomas. Malden, Massachusetts: Blackwell Publishing. pp. 41. ISBN 978-1-4051-1376-2.
- ↑ 16.0 16.1 16.2 "Mycosis Fungoides (Including Sézary Syndrome) Treatment" (in en). 12 July 2017. https://www.cancer.gov/types/lymphoma/hp/mycosis-fungoides-treatment-pdq#link/_449_toc.
- ↑ Jawed, SI; Myskowski, PL; Horwitz, S; Moskowitz, A; Querfeld, C (February 2014). "Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part II. Prognosis, management, and future directions.". Journal of the American Academy of Dermatology 70 (2): 223.e1–17; quiz 240–2. doi:10.1016/j.jaad.2013.08.033. PMID 24438970.
- ↑ Subramaniam, Joshuan M.; Whiteside, Glenn; McKeage, Kate; Croxtall, Jamie C. (2012-06-18). "Mogamulizumab: first global approval". Drugs 72 (9): 1293–1298. doi:10.2165/11631090-000000000-00000. ISSN 1179-1950. PMID 22686619. https://pubmed.ncbi.nlm.nih.gov/22686619/.
- ↑ "FDA approves mogamulizumab-kpkc for mycosis fungoides or Sézary syndrome". 2018-08-08. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-mogamulizumab-kpkc-mycosis-fungoides-or-sezary-syndrome.
External links
| Classification | |
|---|---|
| External resources |
 |