Medicine:Tooth replantation
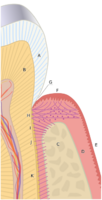
Tooth replantation is a form of restorative dentistry in which an avulsed or luxated tooth is reinserted[1] and secured into its socket through a combination of dental procedures. The purposes of tooth replantation is to resolve tooth loss and preserve the natural landscape of the teeth.[1][2] Whilst variations of the procedure exist including, Allotransplantation, where a tooth is transferred from one individual to another individual of the same species.[3] It is a largely defunct practice due to the improvements made within the field of dentistry and due to the risks and complications involved including the transmission of diseases such as syphilis,[4] histocompatibility,[5] as well as the low success rate of the procedure, has resulted in its practice being largely abandoned. Autotransplantation, otherwise known as intentional replantation in dentistry, is defined as the surgical movement of a tooth from one site on an individual to another location in the same individual.[6][7][8] While rare, modern dentistry uses replantation as a form of proactive care to prevent future complications and protect the natural dentition[9] in cases where root canal and surgical endodontic treatments are problematic. In the modern context, tooth replantation most often refers to reattachment of an avulsed or luxated permanent tooth into its original socket.
History
One of the first recorded surgeries with details on tooth replantation was made by Ambroise Paré in 1962.[10] However, earlier dental interventions of this nature documented in the 11th century ad were made by Abulcasis,[11] who described replantation and use of ligatures to splint the replanted tooth. The earliest instances of tooth replantation, however, can be traced back to ancient Egypt, where slaves were forced to give their teeth to the pharaoh. Tooth replantation saw further usage within the 17th and 18th century Europe, becoming popular nearing the end of the 18th century most often in the form of allotransplantation. In many cases, older wealthy patients whose teeth had decayed often paid poor people to have their teeth removed to be replanted in their own mouths.[12] Another instance of a similar situation occurred during the Napoleonic wars, where soldiers were forced to donate their teeth to the officers who had lost theirs in battle. In 1685, Charles Allen wrote of tooth transplantation in the first English dental textbook, The Operator for the Teeth, and encouraged the replantation of teeth from animals as he considered it to be “inhumane” to source them from people. In 1890, Scheff J. Die highlighted the role of the periodontal ligament in long term prognosis of replanted teeth. In 1955, Hammer H. highlighted the importance of leaving an intact PDL on intentionally replanted teeth. In 1974, Cvek M, Hollender L and Nord CE showed that the removal of the dental pulp following replantation was required to prevent root resorption and also demonstrated that storage of knocked out teeth in saline could improve the success of replanted teeth.[13]
Procedure
Dental avulsions are a dental emergency and replantations are generally performed by either dentists, endodontists, or oral surgeons.
Diagnosis
Prior to implantation the suitability of the avulsed tooth and the gum must be assessed to determine the correct procedure for tooth implantation.
Process
Prior to the beginning of the procedure, a local anaesthetic should be administered to both the palatal & lingual tissues to numb the surrounding area and minimise discomfort. Gentle irrigation with a saline solution should be performed on the tooth to remove blood clots and possible contaminants from the tooth. Following preparation, any injury to the gum is treated before the tooth is reinserted into the socket and kept stable through the use of splints to adjacent teeth.[14]
Aftercare
The patient may be given mild pain killers such as paracetamol for the pain. Antibiotics may also be prescribed to prevent infection. The patient should avoid rinsing the mouth, spitting, contact sports, or smoking for the first 24 hours after surgery and should limit food to a soft diet for the next few days. Following surgery, subsequent check ups may be required to evaluate the success of the procedure.
Complications and risk
Pulp necrosis
Root resorption
A leakage of toxins from the infected pulp through dentinal tubules will start a chain reaction that stimulates osteoclasts to resorb, not only from the cementum and dentin, but also alveolar bone. This starts an aggressive resorption process that can lead to loss of most of the root structure in a few months.
Tooth discolouration
Following any type of trauma to a tooth, there is a possibility for the tooth to discolour. When teeth are damaged or injured in any way, as internal bleeding occurs in the pulp chamber, blood gets into the dentinal nerves and gets trapped into the pulp, staining the dentin. Post trauma, a tooth can discolour and turn black or grey within a few days and if the injury is mild the tooth may return to its original status. However, a severely traumatised tooth may darken gradually with each passing day indicating poor functioning of the dentinal nerves. The tooth ultimately loses its vitality within a few months or a year and will require nerve treatment.[15]
Replacement osseous resorption "Ankylosis"
Replacement osseous resorption otherwise known as "Ankylosis" of replanted teeth occurs when the root has been stripped of its periodontal membrane, when osteoclasts originating from the surrounding alveolar bone and subsequently osteoblasts, reach the root surface after crossing the damaged periodontal ligament (PDL) and precementum[16] allowing for the joining of the cementum and the bone.[17] Over a number of years, the adjacent bony socket will remodel the tooth, replacing the root with bone, leaving the tooth with no root. Once the root is replaced the visible part of the tooth, the crown, will eventually give way and be lost.[18]
Contraindications
Primary teeth
The replantation of primary teeth is uniformly cautioned against as primary teeth are in young patients whose facial development is usually incomplete and do not usually have long enough roots for successful replantation.[19] Due to the risks and poor prognosis replanting a primary tooth is cautioned also due to the possible harms it may pose on future permanent teeth.[14][16]
Storage medium
To delay and minimise the death of tooth root cells the avulsed tooth must be stored in a suitable medium.[20][21] Storage in improper mediums can cause further damage to the cells in the tooth, thereby decreasing the chance of successful replantations and increasing potential risks. When considering potential suitable mediums, factors such as fluid pressure and osmolarity need to be taken into account to maintain normal cell metabolism for extended periods of time. Some suitable storage mediums that suit this criteria include Hank's Balanced Salt Solution and whole milk.[22]
Time frame
Delayed replantation has a poor long term prognosis due to the death of the periodontal ligament,[14] increasing the likelihood of complications such as ankylosis, infection and pulp necrosis. Avulsed teeth should be replanted within the hour to increase the likelihood of a successful tooth replantation.[23]
Cell damage
Damage to the cells must be minimised during the handling and transportation of the avulsed tooth. Contact should be avoided with the root of the teeth and attempts to cleaning through the use of either soaps, chemicals or toothpaste must not occur.[20] Too much damage occur to the periodontal membrane or fibrolasts, tooth reimplantation may become unviable due to the complications that it presents due to ankylosis and root resorption.
References
- ↑ 1.0 1.1 "Clinical Practice Procedures: Trauma/Tooth Replantation". Queensland Government. https://www.ambulance.qld.gov.au/docs/clinical/cpp/CPP_Tooth%20replantation.pdf.
- ↑ Yu, Sang-Joun; Lee, Jung-Seok; Jung, Ui-Won; Park, Joo-Cheol; Kim, Byung-Ock; Choi, Seong-Ho (2015). "Effect of fibroblast growth factor on injured periodontal ligament and cementum after tooth replantation in dogs". Journal of Periodontal & Implant Science 45 (3): 111–9. doi:10.5051/jpis.2015.45.3.111. ISSN 2093-2278. PMID 26131371.
- ↑ Natiella, Joseph R.; Armitage, Jack E.; Greene, George W. (March 1970). "The replantation and transplantation of teeth". Oral Surgery, Oral Medicine, Oral Pathology 29 (3): 397–419. doi:10.1016/0030-4220(70)90143-X. PMID 4983973.
- ↑ "Transplanting of teeth". https://bda.org/museum/collections/dental-art/transplanting-of-teeth.
- ↑ Nimčenko, Tatjana; Omerca, Gražvydas; Varinauskas, Vaidas; Bramanti, Ennio; Signorino, Fabrizio; Cicciù, Marco (2013). "Tooth auto-transplantation as an alternative treatment option: A literature review". Dental Research Journal 10 (1): 1–6. doi:10.4103/1735-3327.111756. ISSN 1735-3327. PMID 23878556.
- ↑ Northway, W. M.; Konigsberg, S. (February 1980). "Autogenic tooth transplantation. The "state of the art"". American Journal of Orthodontics 77 (2): 146–162. doi:10.1016/0002-9416(80)90003-2. ISSN 0002-9416. PMID 6986782.
- ↑ Hale, M. L. (November 1965). "Autogenous transplants". The British Journal of Oral Surgery 3 (2): 109–113. doi:10.1016/s0007-117x(65)80016-6. ISSN 0007-117X. PMID 5222733.
- ↑ Clokie; Yau; Chano (2001). "Autogenous Tooth Transplantation: An Alternative to Dental Implant Placement". Journal of the Canadian Dental Association 67 (2): 92–6. PMID 11253297.
- ↑ Nagappa, G.; Aspalli, Shivanand; Devanoorkar, Archana; Shetty, Sudhir; Parab, Prachi (September 2013). "Intentional replantation of periodontally compromised hopeless tooth". Journal of Indian Society of Periodontology 17 (5): 665–669. doi:10.4103/0972-124X.119291. ISSN 0972-124X. PMID 24174765.
- ↑ Weinberger, Bernhard Wolf (1948). An introduction to the history of dentistry. St. Louis: C.V. Mosby Co..
- ↑ Kingsbury, Bernard C.; Wiesenbaugh, Joseph M. (November 1971). "Intentional Replantation of Mandibular Premolars and Molars". The Journal of the American Dental Association 83 (5): 1053–1057. doi:10.14219/jada.archive.1971.0425. ISSN 0002-8177. PMID 5286134.
- ↑ "Transplanting of Teeth". British Dental Association. https://bda.org/museum/collections/dental-art/transplanting-of-teeth.
- ↑ Cvek, M.; Hollender, L.; Nord, C. E. (1976). "Treatment of non-vital permanent incisors with calcium hydroxide. VI. A clinical, microbiological and radiological evaluation of treatment in one sitting of teeth with mature or immature root". Odontologisk Revy 27 (2): 93–108. ISSN 0029-8441. PMID 1064826.
- ↑ 14.0 14.1 14.2 Trope, Martin (August 2011). "Avulsion of permanent teeth: theory to practice: Avulsion of permanent teeth". Dental Traumatology 27 (4): 281–294. doi:10.1111/j.1600-9657.2011.01003.x. PMID 21635689.
- ↑ Heithersay, G. S.; Hirsch, R. S. (September 1993). "Tooth discoloration and resolution following a luxation injury: significance of blood pigment in dentin to laser Doppler flowmetry readings". Quintessence International 24 (9): 669–676. ISSN 0033-6572. PMID 8272505.
- ↑ 16.0 16.1 Holan, Gideon (June 2013). "Replantation of avulsed primary incisors: a critical review of a controversial treatment". Dental Traumatology 29 (3): 178–184. doi:10.1111/edt.12038. PMID 23480044.
- ↑ Campbell, Karen M.; Casas, Michael J.; Kenny, David J. (2005). "Ankylosis of Traumatized Permanent Incisors: Pathogenesis and Current Approaches to Diagnosis and Management". Journal of the Canadian Dental Association 71 (10): 763–8. PMID 16324230. https://cda-adc.ca/jcda/vol-71/issue-10/763.pdf.
- ↑ Day, Peter F; Duggal, Monty; Nazzal, Hani (2019-02-05). Cochrane Oral Health Group. ed. "Interventions for treating traumatised permanent front teeth: avulsed (knocked out) and replanted". Cochrane Database of Systematic Reviews 2019 (2): CD006542. doi:10.1002/14651858.CD006542.pub3. PMID 30720860.
- ↑ Zamon, Erica L.; Kenny, David J. (2001). "Replantation of Avulsed Primary Incisors: A Risk–Benefit Assessment". Journal (Canadian Dental Association) 67 (7): 386. PMID 11468096. https://www.cda-adc.ca/jcda/vol-67/issue-7/386.html.
- ↑ 20.0 20.1 Khinda, Vineet IS; Kaur, Gurpreet; Brar, Gurlal S; Kallar, Shiminder; Khurana, Heena (2017). Marwah, Nikhil. ed. "Clinical and Practical Implications of Storage Media used for Tooth Avulsion". International Journal of Clinical Pediatric Dentistry 10 (2): 158–165. doi:10.5005/jp-journals-10005-1427. PMID 28890616.
- ↑ Hassel, Henry J. Van; Harrington, Gerald W.; Oswald, Robert J. (1980-05-01). "A postreplantation evaluation of air-dried and saliva-stored avulsed teeth" (in en). Journal of Endodontics 6 (5): 546–551. doi:10.1016/S0099-2399(80)80148-8. ISSN 0099-2399. PMID 6935358. https://www.jendodon.com/article/S0099-2399(80)80148-8/abstract.
- ↑ Pohl, Yango; Filippi, Andreas; Kirschner, Horst (2005). "Results after replantation of avulsed permanent teeth. II. Periodontal healing and the role of physiologic storage and antiresorptive-regenerative therapy". Dental Traumatology 21 (2): 93–101. doi:10.1111/j.1600-9657.2004.00298.x. ISSN 1600-9657. PMID 15773888.
- ↑ Flores, Marie Therese; Andersson, Lars; Andreasen, Jens Ove; Bakland, Leif K.; Malmgren, Barbro; Barnett, Frederick; Bourguignon, Cecilia; DiAngelis, Anthony et al. (2007). "Guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth". Dental Traumatology 23 (3): 130–136. doi:10.1111/j.1600-9657.2007.00605.x. ISSN 1600-9657. PMID 17511833.
 |