Medicine:Rectilinear scanner
| Rectilinear scanner | |
|---|---|
| Medical diagnostics | |
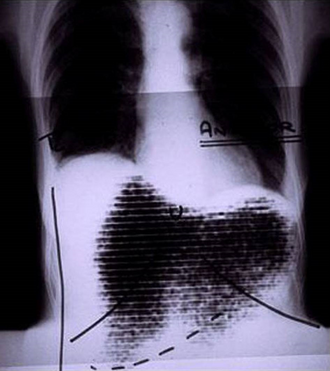 Manual image fusion of x-rayed and rectilinear scanned chest | |
| Purpose | capture emission from radiopharmaceuticals in nuclear medicine. |
A rectilinear scanner is an imaging device, used to capture emission from radiopharmaceuticals in nuclear medicine. The image is created by physically moving a radiation detector over the surface of a radioactive patient. It has become obsolete in medical imaging, largely replaced by the gamma camera since the late 1960s.[1][2][3]
History
One of the first rectilinear scanners was developed by Benedict Cassen in 1950. Before then hand-held detectors had been used to locate radioactive materials in patients, but the Cassen system (designed for Iodine-131) combined a motor driven photomultiplier tube and printing mechanism.[2][4] Subsequent developments improved the detection systems, movement, display and printing of images.[5][6]
Components
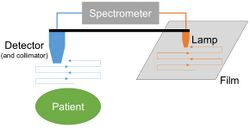
Cassen's original rectilinear scanner used calcium tungstate (CaWo4) crystal as the radiation detector. Later systems used a Sodium iodide (NaI) scintillator, as in a gamma camera.[7] The detector must be connected by mechanical or electronic means to an output system. This could be a simple light source over photographic film, dot matrix printer, oscilloscope or television screen.[8][9][10]
Mechanism
The patient is administered with a radioactive pharmaceutical agent, such as radio-iodine which will naturally collect in the thyroid. The detector moves in a raster pattern over studied area of the patient, making a constant count rate. A collimator restricts detection to a small area directly below its position so that by the end of the scan emission from the whole study area has been detected. The output method is designed such that positional and detection information is maintained. For example, when using a light source and film the light is moved in tandem with the detector, and the intensity of light produced increases with an increase in activity, producing dark areas on the film.[11][12]
Disadvantages include the very long imaging time (several minutes) due to the need to separately cover each target area, unlike a gamma camera which has a much larger field of view, and the motion artefacts this can result in.[13][14]
References
- ↑ Williams, Lawrence E. (12 June 2008). "Anniversary Paper: Nuclear medicine: Fifty years and still counting". Medical Physics 35 (7): 3020–3029. doi:10.1118/1.2936217. PMID 18697524. Bibcode: 2008MedPh..35.3020W.
- ↑ 2.0 2.1 Blahd, WH (July 1996). "Ben Cassen and the development of the rectilinear scanner.". Seminars in Nuclear Medicine 26 (3): 165–70. doi:10.1016/s0001-2998(96)80021-3. PMID 8829277.
- ↑ Feld, Michael; de Roo, Michel (2003). History of nuclear medicine in Europe. Stuttgart: Schattauer. p. 3. ISBN 9783794522347. https://books.google.com/books?id=MumQU40Pe04C&pg=PA8.
- ↑ Hutton, Brian F (2014). "The contribution of Medical Physics to Nuclear Medicine: looking back - a physicist's perspective". EJNMMI Physics 1 (1): 2. doi:10.1186/2197-7364-1-2. PMID 26501444.
- ↑ McCready, Ralph. "Early days in the Evolution of Radioisotope Imaging In the UK 1950-1970". http://www.bnms.org.uk/~bnms/images/stories/downloads/documents/microsoft_word_-_text_for_the_nukdoctor_web_page..pdf.
- ↑ McCready, Ralph (2016). "A History of Nuclear Medicine in the UK". A History of Radionuclide Studies in the UK. London: Springer. pp. 9–18. doi:10.1007/978-3-319-28624-2_2. ISBN 978-3-319-28623-5.
- ↑ Hendee, William R; Ritenour, E Russell (2002). Medical Imaging Physics, Fourth Edition. (4th ed.). Hoboken, NJ: John Wiley & Sons. p. 210. ISBN 9780471461135.
- ↑ Mayneord, WV; Turner, R C; Newbery, SP; Hodt, HJ (3 November 1951). "A Method of Making Visible the Distribution of Activity in a Source of Ionizing Radiation". Nature 168 (4279): 762–765. doi:10.1038/168762a0. Bibcode: 1951Natur.168..762M.
- ↑ Dowsett, DJ; Ritchie, DR (1 April 1971). "An off-line computer interface for a rectilinear scanner". Physics in Medicine and Biology 16 (2): 249–256. doi:10.1088/0031-9155/16/2/307. PMID 5581630. Bibcode: 1971PMB....16..249D.
- ↑ Reese, IC; Mishkin, FS (October 1976). "Direct recording on rectilinear scan images on 4x5-in. film.". Journal of Nuclear Medicine 17 (10): 937–8. PMID 966063. http://jnm.snmjournals.org/content/17/10/937.long.
- ↑ van Herk, G (1986). "Nuclear imaging: Advances and trends". IAEA Bulletin. https://www.iaea.org/sites/default/files/publications/magazines/bulletin/bull28-2/28205882025.pdf.
- ↑ Patton, Dennis D (1980). "Rectilinear Scanners". Nuclear Medicine, Ultrasonics,and Thermography. New York: Springer. pp. 89–118. doi:10.1007/978-1-4684-3671-6_3. ISBN 978-1-4684-3673-0.
- ↑ Cherry, Simon R; Sorenson, James A; Phelps, Michael E (2012). "The Gamma Camera: Basic Principles". Physics in nuclear medicine (4th ed.). Philadelphia: Elsevier/Saunders. pp. 195–208. doi:10.1016/B978-1-4160-5198-5.00013-7. ISBN 978-1-4160-5198-5. https://archive.org/details/physicsnuclearme00phds.
- ↑ Gottschalk, A; Harper, PV; Jiminez, FF; Petasnick, JP (April 1966). "Quantification of the respiratory motion artifact in radioisotope scanning with the rectilinear focused collimator scanner and the gamma scintillation camera.". Journal of Nuclear Medicine 7 (4): 243–51. PMID 5930230. http://jnm.snmjournals.org/content/7/4/243.long.
 |