Medicine:Overdiagnosis
Overdiagnosis is the diagnosis of disease that will never cause symptoms or death during a patient's ordinarily expected lifetime[1] and thus presents no practical threat regardless of being pathologic. Overdiagnosis is a side effect of screening for early forms of disease. Although screening saves lives in some cases, in others it may turn people into patients unnecessarily and may lead to treatments that do no good and perhaps do harm. Given the tremendous variability that is normal in biology, it is inherent that the more one screens, the more incidental findings will generally be found. For a large percentage of them, the most appropriate medical response is to recognize them as something that does not require intervention; but determining which action a particular finding warrants ("ignoring", watchful waiting, or intervention) can be very difficult, whether because the differential diagnosis is uncertain or because the risk ratio is uncertain (risks posed by intervention, namely, adverse events, versus risks posed by not intervening).
Overdiagnosis occurs when a disease is diagnosed correctly, but the diagnosis is irrelevant. A correct diagnosis may be irrelevant because treatment for the disease is not available, not needed, or not wanted. Some people contend that the term "overdiagnosis" is inappropriate, and that "overtreatment" is more representative of the phenomenon.
Because most people who are diagnosed are also treated, it is difficult to assess whether overdiagnosis has occurred in an individual. Overdiagnosis in an individual cannot be determined during life. Overdiagnosis is only certain when an individual remains untreated, never develops symptoms of the disease and dies of something else. The distinction of "died with disease" versus "died of disease" is then important and relevant. Thus most of the inferences about overdiagnosis comes from the study of populations. Rapidly rising rates of testing and disease diagnosis in the setting of stable rates of the feared outcome of the disease (e.g. death) are highly suggestive of overdiagnosis. Most compelling, however, is evidence from a randomized trial of a screening test intended to detect pre-clinical disease. A persistent excess of detected disease in the tested group years after the trial is completed constitutes the best evidence that overdiagnosis has occurred.
Although overdiagnosis is potentially applicable to the diagnosis of any disease, the concept was first recognized and studied in cancer screening—the systematic evaluation of asymptomatic patients to detect early forms of cancer.[2] The central harm of cancer screening is overdiagnosis—the detection of abnormalities that meet the pathologic definition of cancer (under the microscope) but will never progress to cause symptoms or death during a patient's ordinarily expected lifetime.
In advanced age, such as 65 years or older, the concept of overdiagnosis takes on increasing importance as life expectancy decreases. There are various cancer types for which a standard contraindication to screening is life expectancy of less than 10 years, for the simple and logical reason that a person who already has medically complex health status (e.g., multiple comorbidities) and realistically can probably expect to live for less than 10 years is less likely to get a net benefit (balance of benefit versus harms) from diagnosing and treating that cancer, especially if it may be indolent anyway. Prostate cancer is a classic example, but the concept can apply to breast cancer and other types as well.
Overdiagnosis and the variability of cancer progression
Cancer screening is the effort to detect cancer early, during its pre-clinical phase—the time period that begins with an abnormal cell and ends when the patient notices symptoms from the cancer. It has long been known that some people have cancers with short pre-clinical phases (fast-growing, aggressive cancers), while others have cancers with long pre-clinical phases (slow-growing cancers). And this heterogeneity has an unfortunate implication: namely, screening tends to disproportionately detect slow-growing cancers (because they are accessible to be detected for a long period of time) and disproportionately miss the fast-growing cancers (because they are only accessible to be detected for a short period of time)—the very cancers we would most like to catch. For more information, see Screening.
This long-standing model has a hidden assumption: namely, that all cancers inevitably progress. But some pre-clinical cancers will not progress to cause problems for patients. And if screening (or testing for some other reason) detects these cancers, overdiagnosis has occurred.
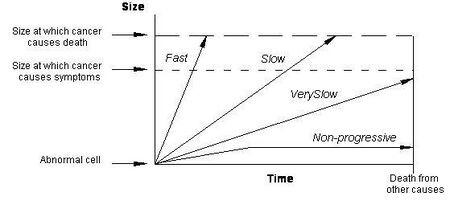
The figure below depicts the heterogeneity of cancer progression using 4 arrows to represent 4 categories of cancer progression.
The arrow labeled "Fast" represents a fast-growing cancer, one that quickly leads to symptoms and to death. These are the worst forms of cancer and unfortunately often appear in the interval between screening tests. The arrow labeled "Slow" represents a slow-growing cancer, one that leads to symptoms and death but only after many years. These are the cancers for which screening has arguably the greatest beneficial impact.
The arrow labeled "Very Slow" represents a cancer that never causes problems because it is growing very slowly. If a cancer grows slowly enough, then patients will die of some other cause before the cancer gets big enough to produce symptoms.
The arrow labeled "Non-progressive" represents a cancer that never causes problems because it is not growing at all. In other words, there are cellular abnormalities that meet the pathologic definition of cancer but never grow to cause symptoms—alternatively, they may grow and then regress. Although the concept of non-progressive cancers may seem implausible, basic scientists have begun to uncover biologic mechanisms that halt the progression of cancer.[3][4][5] Some cancers outgrow their blood supply (and are starved), others are recognized by the host's immune system (and are successfully contained), and some are not that aggressive in the first place.
Cancer that grows too slowly to be likely to harm the patient is usually referred to as a benign tumor. Although some types of benign tumor may require intervention, they are often simply monitored for malignant transformation.[6][7]
Evidence for overdiagnosis in cancer
The phenomenon of overdiagnosis is most widely understood in prostate cancer.[8] A dramatic increase in the number of new cases of prostate cancer was observed following the introduction of the PSA (prostate specific antigen) screening test. Because of the problem of overdiagnosis, most organizations recommend against prostate cancer screening in men with limited life expectancy—generally defined as less than 10 years (see also prostate cancer screening).
Overdiagnosis has been identified in mammographic screening for breast cancer.[9][10] Long-term follow-up of the Malmo randomized trial of mammography found a persistent excess of 115 breast cancers in the screened group 15 years after the trial was completed (a 10% rate of overdiagnosis).[11] In a letter to the editor, authors not associated with the original study of the data from the randomized clinical trial argued that one-quarter of mammographically detected breast cancers represent overdiagnosis.[12] A systematic review of mammography screening programs reported an overdiagnosis rate of around 50%, which is the same of saying that a third of diagnosed cases of breast cancer are overdiagnosed.[13]
Overdiagnosis has also been identified in chest x-ray screening for lung cancer.[14] Long-term follow-up of the Mayo Clinic randomized trial of screening with chest x-rays and sputum cytology found a persistent excess of 46 lung cancer cases in the screened group 13 years after the trial was completed,[15] suggesting that 20–40% of lung cancers detected by conventional x-ray screening represent overdiagnosis. There is considerable evidence that the problem of overdiagnosis is much greater for lung cancer screening using spiral-CT scans.[16]
Overdiagnosis has also been associated with early detection in a variety of other cancers, including neuroblastoma,[17][18] melanoma,[19] and thyroid cancer.[20] In fact, some degree of overdiagnosis in cancer early detection is probably the rule, not the exception.[citation needed]
Evidence for overdiagnosis of infectious diseases
Issues with overdiagnosis of infectious diseases, such as malaria or typhoid fever, persist in many regions around the world. For example, malaria overdiagnosis is well-documented in African countries.[21][22] and results in over-inflation of actual malaria rates reported at the local and national levels.[23] Health facilities tend to over-diagnose malaria in patients presenting with symptoms such as fever, due to traditional perceptions (for example any fever being equivalent to malaria) and issues related to laboratory testing (see Diagnosis of malaria).[24][25] Therefore, malaria overdiagnosis leads to under-management of other fever-inducing conditions,[22] but also to over-prescription of antimalarial drugs.[26]
Harms of overdiagnosis
Overdiagnosed patients cannot benefit from the detection and treatment of their "cancer" because the cancer was never destined to cause symptoms or death. They can only be harmed. There are three categories of harm associated with overdiagnosis:
- Physical effects of unnecessary diagnosis and treatment: All medical interventions have side effects. This is particularly true of cancer treatments. Surgery, radiation and chemotherapy all pose varying morbidity and mortality risks.
- Psychological effects: there is a burden for an individual simply being labeled as "diseased" (e.g. the burden of being labeled a "cancer patient") and an associated increased sense of vulnerability.
- Economic burden: Not only the associated cost of treatment (from which the patient cannot benefit, because the disease posed no threat), but also—at least, in the current health care system in the United States—a potential increase in the cost of health insurance or even an inability to procure it (e.g. the diagnosis creates a pre-existing condition that affects health insurance). Similar issues may arise with life insurance. Unlike health insurance, life insurance does not fall under the scope of the Affordable Care Act, thus insurers have even more leeway in denying or reducing coverage or inflating premiums due to the patient's condition.
While many identify false positive results as the major downside to cancer screening, there are data to suggest that—when patients are informed about overdiagnosis—they are much more concerned about overdiagnosis than false positive results.[27]
Distinction among overdiagnosis, misdiagnosis, and false positive results
Overdiagnosis is often confused with the term "false positive" test results and with misdiagnosis, but they are three distinct concepts.[28] A false positive test result refers to a test that suggests the presence of disease, but is ultimately proved to be in error (usually by a second, more precise test). Patients with false positive test results may be told that they have a disease and erroneously treated; overdiagnosed patients are told they have disease and generally receive treatment. Misdiagnosed patients do not have the condition at all, or have a totally different condition, but are treated anyway.
Overdiagnosis is also distinct from overtesting. Overtesting is the phenomenon where patients receive a medical test that they don't need; it will not benefit them.[29] For instance, a patient that receives a lumbar spine x-ray when they have low back pain without any sinister signs or symptoms (weight loss, fever, lower limb paresthesia, etc.) and symptoms have been present for less than 4 weeks. Most tests are subject to overtesting, but echocardiograms (ultrasounds of the heart) have been shown to be particularly prone to overtesting.[29] The detection of overtesting is difficult; recently, many population-level estimates have emerged to try to detect potential overtesting. The most common of these estimates is geographical variation in test use. These estimates detect regions, hospitals or general practices that order many more tests, compared to their peers, irrespective of differences in patient demographics between regions.[30][31] Further methods that have been used include identifying general practices that order a higher proportion of tests that return a normal result,[30] and the identification of tests with large temporal increases in their use, without a justifiable reason.[32]
| Overdiagnosis | False Positive Results | Misdiagnosis | |
|---|---|---|---|
| Definition | Detection of a "disease" that will never cause symptoms or death during a patient's lifetime | A "false alarm"—an initial test result that suggests the presence of disease, but later proved false (no disease is present) | Diagnosis of a disease that the patient does not in fact have (either they are "normal" or they have a different condition) |
| Patient experience | Told they have the disease | Told that the test was wrong and they do not have the disease (usually after being first told they have the disease or at least may have it) | Told they have the disease |
| Physician action | Generally, initiates treatment | Reassurance | Generally, initiates treatment |
| Potential Harms |
|
|
|
Solutions to overdiagnosis
The concept of undiagnosing is a strategy to review diagnostic labels and remove those that are unnecessary or no longer beneficial. It is important that the medical record is updated to reflect the removal of the diagnosis.[33]
Removing cancer from names of low-risk diagnoses
It has been proposed that some conditions that are indolent (i.e., unlikely to cause appreciable harm during the patient's lifetime) should have the words "cancer" or "carcinoma" removed from their accepted/preferred medical name.[34] Such a proposal is to name conditions as indolent lesions of epithelial origin or IDLE.[34]
See also
- Disease mongering
- False positive
- Medicalization
- Interventionism
- Patient education
- Schooliosis
- Screening
References
- ↑ Welch, H. G.; Black, W. C. (5 May 2010). "Overdiagnosis in Cancer". JNCI Journal of the National Cancer Institute 102 (9): 605–613. doi:10.1093/jnci/djq099. PMID 20413742.
- ↑ Welch, H. Gilbert (2006). Should I Be Tested for Cancer?: Maybe Not and Here's Why. University of California Press. ISBN 978-0-520-24836-6.[page needed]
- ↑ Mooi, W.J.; Peeper, D.S. (7 September 2006). "Oncogene-Induced Cell Senescence — Halting on the Road to Cancer". New England Journal of Medicine 355 (10): 1037–1046. doi:10.1056/NEJMra062285. PMID 16957149.
- ↑ Folkman, Judah; Kalluri, Raghu (February 2004). "Cancer without disease". Nature 427 (6977): 787. doi:10.1038/427787a. PMID 14985739. Bibcode: 2004Natur.427..787F.
- ↑ Serrano, Manuel (10 May 2007). "Cancer Regression by Senescence". New England Journal of Medicine 356 (19): 1996–1997. doi:10.1056/NEJMcibr071461. PMID 17494935.
- ↑ Lam, Yee (June 2020). "Bone Tumors: Benign Bone Tumors". FP Essentials 493: 11–21. PMID 32573182.
- ↑ Stachs, Angrit; Stubert, Johannes; Reimer, Toralf; Hartmann, Steffi (19 August 2019). "Benign Breast Disease in Women". Deutsches Ärzteblatt International 116 (33–34): 565–574. doi:10.3238/arztebl.2019.0565. PMID 31554551.
- ↑ Etzioni, Ruth; Penson, David F.; Legler, Julie M.; di Tommaso, Dante; Boer, Rob; Gann, Peter H.; Feuer, Eric J. (3 July 2002). "Overdiagnosis due to prostate-specific antigen screening: lessons from U.S. prostate cancer incidence trends". Journal of the National Cancer Institute 94 (13): 981–990. doi:10.1093/jnci/94.13.981. PMID 12096083.
- ↑ Zahl, Per-Henrik; Strand, Bjørn Heine; Maehlen, Jan (17 April 2004). "Incidence of breast cancer in Norway and Sweden during introduction of nationwide screening: prospective cohort study". BMJ 328 (7445): 921–924. doi:10.1136/bmj.38044.666157.63. PMID 15013948.
- ↑ Gøtzsche, Peter C; Jørgensen, Karsten Juhl (4 June 2013). "Screening for breast cancer with mammography". Cochrane Database of Systematic Reviews 2013 (6): CD001877. doi:10.1002/14651858.CD001877.pub5. PMID 23737396.
- ↑ Zackrisson, Sophia; Andersson, Ingvar; Janzon, Lars; Manjer, Jonas; Garne, Jens Peter (25 March 2006). "Rate of over-diagnosis of breast cancer 15 years after end of Malmö mammographic screening trial: follow-up study". BMJ 332 (7543): 689–692. doi:10.1136/bmj.38764.572569.7C. PMID 16517548.
- ↑ Welch, H Gilbert; Schwartz, Lisa M; Woloshin, Steven (25 March 2006). "Ramifications of screening for breast cancer: 1 in 4 cancers detected by mammography are pseudocancers". BMJ 332 (7543): 727.1. doi:10.1136/bmj.332.7543.727. PMID 16565136.
- ↑ Jorgensen, K. J.; Gotzsche, P. C (9 July 2009). "Overdiagnosis in publicly organised mammography screening programmes: systematic review of incidence trends". BMJ 339: b2587. doi:10.1136/bmj.b2587. PMID 19589821.
- ↑ Black, W. C. (16 August 2000). "Overdiagnosis: An Underrecognized Cause of Confusion and Harm in Cancer Screening". JNCI Journal of the National Cancer Institute 92 (16): 1280–1282. doi:10.1093/jnci/92.16.1280. PMID 10944539.
- ↑ Marcus, P. M.; Bergstralh, E. J.; Fagerstrom, R. M.; Williams, D. E.; Fontana, R.; Taylor, W. F.; Prorok, P. C. (16 August 2000). "Lung Cancer Mortality in the Mayo Lung Project: Impact of Extended Follow-up". JNCI Journal of the National Cancer Institute 92 (16): 1308–1316. doi:10.1093/jnci/92.16.1308. PMID 10944552.
- ↑ Welch, H. Gilbert; Woloshin, Steven; Schwartz, Lisa M.; Gordis, Leon; Gøtzsche, Peter C.; Harris, Russell; Kramer, Barnett S.; Ransohoff, David F. (26 November 2007). "Overstating the Evidence for Lung Cancer Screening: The International Early Lung Cancer Action Program (I-ELCAP) Study". Archives of Internal Medicine 167 (21): 2289–2295. doi:10.1001/archinte.167.21.2289. PMID 18039986.
- ↑ Schilling, Freimut H.; Spix, Claudia; Berthold, Frank; Erttmann, Rudolf; Fehse, Natalja; Hero, Barbara; Klein, Gisela; Sander, Johannes et al. (4 April 2002). "Neuroblastoma Screening at One Year of Age". New England Journal of Medicine 346 (14): 1047–1053. doi:10.1056/NEJMoa012277. PMID 11932471.
- ↑ Yamamoto, K; Hanada, R; Kikuchi, A; Ichikawa, M; Aihara, T; Oguma, E; Moritani, T; Shimanuki, Y et al. (April 1998). "Spontaneous regression of localized neuroblastoma detected by mass screening.". Journal of Clinical Oncology 16 (4): 1265–1269. doi:10.1200/JCO.1998.16.4.1265. PMID 9552024.
- ↑ Welch, H Gilbert; Woloshin, Steven; Schwartz, Lisa M (3 September 2005). "Skin biopsy rates and incidence of melanoma: population based ecological study". BMJ 331 (7515): 481. doi:10.1136/bmj.38516.649537.E0. PMID 16081427.
- ↑ Davies, Louise; Welch, H. Gilbert (10 May 2006). "Increasing Incidence of Thyroid Cancer in the United States, 1973-2002". JAMA 295 (18): 2164–2167. doi:10.1001/jama.295.18.2164. PMID 16684987.
- ↑ Ghai, Ria R.; Thurber, Mary I.; El Bakry, Azza; Chapman, Colin A.; Goldberg, Tony L. (December 2016). "Multi-method assessment of patients with febrile illness reveals over-diagnosis of malaria in rural Uganda". Malaria Journal 15 (1): 460. doi:10.1186/s12936-016-1502-4. PMID 27604542.
- ↑ 22.0 22.1 Reyburn, Hugh; Mbatia, Redepmta; Drakeley, Chris; Carneiro, Ilona; Mwakasungula, Emmanuel; Mwerinde, Ombeni; Saganda, Kapalala; Shao, John et al. (20 November 2004). "Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study". BMJ 329 (7476): 1212. doi:10.1136/bmj.38251.658229.55. PMID 15542534.
- ↑ Salomão, Cristolde A.; Sacarlal, Jahit; Chilundo, Baltazar; Gudo, Eduardo Samo (December 2015). "Prescription practices for malaria in Mozambique: poor adherence to the national protocols for malaria treatment in 22 public health facilities". Malaria Journal 14 (1): 483. doi:10.1186/s12936-015-0996-5. PMID 26628068.
- ↑ Yegorov, Sergey; Galiwango, Ronald M.; Ssemaganda, Aloysious; Muwanga, Moses; Wesonga, Irene; Miiro, George; Drajole, David A.; Kain, Kevin C. et al. (December 2016). "Low prevalence of laboratory-confirmed malaria in clinically diagnosed adult women from the Wakiso district of Uganda". Malaria Journal 15 (1): 555. doi:10.1186/s12936-016-1604-z. PMID 27842555.
- ↑ Bell, David; Wongsrichanalai, Chansuda; Barnwell, John W. (September 2006). "Ensuring quality and access for malaria diagnosis: how can it be achieved?". Nature Reviews Microbiology 4 (9): 682–695. doi:10.1038/nrmicro1474. PMID 16912713.
- ↑ Mwanziva, Charles; Shekalaghe, Seif; Ndaro, Arnold; Mengerink, Bianca; Megiroo, Simon; Mosha, Frank; Sauerwein, Robert; Drakeley, Chris et al. (December 2008). "Overuse of artemisinin-combination therapy in Mto wa Mbu (river of mosquitoes), an area misinterpreted as high endemic for malaria". Malaria Journal 7 (1): 232. doi:10.1186/1475-2875-7-232. PMID 18986520.
- ↑ Schwartz, LM; Woloshin, S; Sox, HC; Fischhoff, B; Welch, HG (17 June 2000). "US women's attitudes to false positive mammography results and detection of ductal carcinoma in situ: cross sectional survey". BMJ 320 (7250): 1635–1640. doi:10.1136/bmj.320.7250.1635. PMID 10856064.
- ↑ Brodersen, John; Schwartz, Lisa M; Heneghan, Carl; O'Sullivan, Jack William; Aronson, Jeffrey K; Woloshin, Steven (February 2018). "Overdiagnosis: what it is and what it isn't". BMJ Evidence-Based Medicine 23 (1): 1–3. doi:10.1136/ebmed-2017-110886. PMID 29367314.
- ↑ 29.0 29.1 O'Sullivan, Jack W; Albasri, Ali; Nicholson, Brian D; Perera, Rafael; Aronson, Jeffrey K; Roberts, Nia; Heneghan, Carl (11 February 2018). "Overtesting and undertesting in primary care: a systematic review and meta-analysis". BMJ Open 8 (2): e018557. doi:10.1136/bmjopen-2017-018557. PMID 29440142.
- ↑ 30.0 30.1 O'Sullivan, Jack W.; Heneghan, Carl; Perera, Rafael; Oke, Jason; Aronson, Jeffrey K.; Shine, Brian; Goldacre, Ben (December 2018). "Variation in diagnostic test requests and outcomes: a preliminary metric for OpenPathology.net". Scientific Reports 8 (1): 4752. doi:10.1038/s41598-018-23263-z. PMID 29556075. Bibcode: 2018NatSR...8.4752O.
- ↑ Wennberg, John E.; Fisher, Elliott S.; Skinner, Jonathan S. (January 2002). "Geography And The Debate Over Medicare Reform". Health Affairs 21 (Suppl1): W96–W112. doi:10.1377/hlthaff.w2.96. PMID 12703563.
- ↑ O'Sullivan, Jack W; Stevens, Sarah; Hobbs, F D Richard; Salisbury, Chris; Little, Paul; Goldacre, Ben; Bankhead, Clare; Aronson, Jeffrey K et al. (28 November 2018). "Temporal trends in use of tests in UK primary care, 2000-15: retrospective analysis of 250 million tests". BMJ 363: k4666. doi:10.1136/bmj.k4666. PMID 30487169.
- ↑ Hosking, Sarah M.; Etherton-Beer, Christopher; Page, Amy T. (July 2019). "Undiagnosing: Correcting the medical record to prevent over-intervention". Case Reports in Women's Health 23: e00133. doi:10.1016/j.crwh.2019.e00133. PMID 31384565.
- ↑ 34.0 34.1 "Overdiagnosis and Overtreatment in Cancer: An Opportunity for Improvement". JAMA 310 (8): 797–8. 2013. doi:10.1001/jama.2013.108415. PMID 23896967.
Further reading
- Welch, H. Gilbert, Schwartz, Lisa. Overdiagnosed: Making People Sick in the Pursuit of Health. Beacon Press; 2011-01-18. ISBN:9780807022009.
 |