Medicine:Traumatic cardiac arrest
| Traumatic cardiac arrest | |
|---|---|
 | |
| Human heart from an autopsy | |
| Specialty | Cardiology, Emergency Medicine, Critical Care, Trauma |
| Usual onset | Acute onset following trauma to the chest |
| Causes | Blunt or penetrating trauma to the chest |
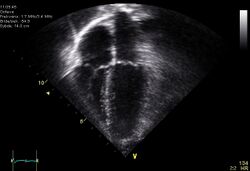
| Diagnostic method | ECG, chest x-ray, bedside echocardiogram |
| Differential diagnosis | Hemorrhagic shock, tension pneumothorax, hemothorax, cardiac tamponade, hypoxia |
| Treatment | Thoracotomy, thoracostomy, fluid resuscitation, decompression, pericardiocentesis |
| Prognosis | Poor |
Traumatic cardiac arrest (TCA) is a condition in which the heart has ceased to beat due to blunt or penetrating trauma, such as a stab wound to the thoracic area.[1] It is a medical emergency which will always result in death without prompt advanced medical care. Even with prompt medical intervention, survival without neurological complications is rare.[2] In recent years, protocols have been proposed to improve survival rate in patients with traumatic cardiac arrest, though the variable causes of this condition as well as many coexisting injuries can make these protocols difficult to standardize.[3] Traumatic cardiac arrest is a complex form of cardiac arrest often derailing from advanced cardiac life support in the sense that the emergency team must first establish the cause of the traumatic arrest and reverse these effects, for example hypovolemia and haemorrhagic shock due to a penetrating injury.[citation needed]
Mechanism
Traumatic cardiac arrest can occur in patients following any severe blunt or penetrating injury to the chest. Following the traumatic event, the heart ceases to pump blood through the body. Unlike medical cardiac arrest, there are several potentially reversible causes that may result in cardiac arrest in the setting of trauma. Clinicians will rapidly assess for these causes, and interventions will be directed to the specific cause.[4]
Massive hemorrhage
In both blunt and penetrating trauma, massive internal or external bleeding may decrease the volume of blood is available to be pumped by the heart to the body. This is considered preload dependent arrest.[4]
Tension pneumothorax
Tension pneumothorax is caused when air is able to enter the space between the lung and the chest wall, but is not able to escape. The increasing pressure within the chest cavity prevents blood from returning from the body to fill the heart.
Hemothorax
Hemothorax occurs when injury to the chest results in bleeding into the thoracic cavity. Similar to tension pneumothorax, increasing pressure prevents the return of blood from circulation to the heart.
Cardiac tamponade
In the setting of trauma, cardiac tamponade results from an acute pericardial effusion, the accumulation of blood within the sac that surrounds the heart. As this sac is filled with fluid, the pressure on the heart is increased, and the chambers of the heart are unable to fill with blood.
Hypoxia
Inability to maintain oxygenation in trauma patients may be a result of airway compromise due to mechanical injury or obstruction or due to loss of the respiratory drive from cervical spine or peripheral nerve injury.[4] These conditions result in the hypoxia that may lead to cardiac arrest.
Signs and symptoms
Patients will present following a traumatic event most often with pulseless electrical activity (PEA). Patients will exhibit low blood pressure with pulses that cannot be palpated. Patients will progress into asystole if the underlying condition is not reversed. Other non-specific signs and symptoms associated with impending traumatic cardiac arrest may include sweating, altered mental status, rapid or slow breathing, and signs of trauma (bruising, laceration, fractures, etc.).[4]
Diagnosis
Diagnosis of traumatic cardiac arrest is initially made with electrocardiogram with EMS or in the emergency department. Clinicians will also order diagnostic testing that may include chest x-ray, bedside ultrasound and echocardiogram, and blood gas levels. A type and cross will be ordered to match the patient to receive blood transfusion if necessary.
Other work-up involved in diagnosis of a trauma patient may include e-FAST, RUSH exam, CBC, pelvic X-ray, and CT of the head, neck, chest, abdomen, and pelvis.
Treatment
Treatment of traumatic cardiac arrest is guided by advanced trauma life support guidelines. Standard advanced cardiac life support guidelines are inappropriate for use in traumatic cardiac arrest, as they are directed primarily at treating pathology originating within the heart itself.[5] As clinicians begin to intervene, they will simultaneously seek reversible causes of the arrest. Management begins by establishing multiple points of IV access and evaluating the patient's airway and breathing. Other interventions may include thoracostomy and thoracotomy, as well as treatment of the underlying cause of arrest.
Basic life support
Basic life support is commonly initiated by bystanders and first responders, but the role of basic life support in traumatic cardiac arrest is unclear. Basic life support is targeted to maintain oxygenation and circulation throughout the body, which can be lifesaving in cases of medical cardiac arrest, but does not address the frequent large volume blood loss encounters in many cases of traumatic cardiac arrest.[5]
Chest compressions
Chest compressions are considered the most important initial intervention in cases of medical cardiac arrest, however studies evaluating their efficacy have excluded patients with traumatic cardiac arrest. Chest compressions work to replace the cardiac function of pumping blood throughout the body, however cases where the heart is either unable to fill with blood or the total blood volume is depleted, this intervention may be ineffective. Additionally, as many of the interventions targeted at specific causes of arrest are centered around procedures performed around the patient's chest, head, and neck, compressions may interfere with definitive management.[5]
Management of reversible causes
| Condition | Goal of Treatment | Initial Treatment | Definitive Treatment |
|---|---|---|---|
| Hypovolemia | Restore circulating volume | Providers will initially establish IV access to provide large volume fluid resuscitation and may use tourniquets or bandages to control bleeding | These patients will likely require blood transfusion for definitive management |
| Tension pneumothorax | Relieve pressure within the chest cavity | Initial treatment may include needle decompression | Definitive treatment for most patients will include tube thoracostomy |
| Hemothorax | Relieve pressure within the chest cavity | Management requires tube thoracostomy | |
| Cardiac tamponade | Relieve pressure within the pericardium | Initial treatment may require pericardiocentesis. This procedure may be sufficient to resolve the tamponade, or further management may be required. | Patient with cardiac tamponade following penetrating trauma may be good candidates for thoracotomy |
| Hypoxia | Increase oxygen content of the blood | Treatment of hypoxia is aimed at maintaining the patient's airway and controlling breathing. Initial treatment may include bag-valve mask, nasopharyngeal airway, oropharyngeal airway, or other airway devices | Definitive management may require intubation or cricothyrotomy |
Future directions
Current guidelines tailored to treatment of specific causes of traumatic cardiac arrest have improved outcomes for patients, however these guidelines may be difficult to apply in a standardized manner due to differences in pre-hospital care and the wide variety of causes of traumatic cardiac arrest compared to medical cardiac arrest.[3] Evolving algorithms are directed at quickly identifying incidences of cardiac arrest with a traumatic source and rapidly intervening to address reversible causes.[3]
Prognosis
Historically, traumatic cardiac arrest was thought to lead invariably to death. More recently, evolutions of advanced trauma life support guidelines and improved understanding of the underlying causes of traumatic cardiac arrest have improved outcomes for patients.[5] Recent studies suggest that the survival rate for traumatic cardiac arrest is similar to that of all-cause cardiac arrest.[6] There is wide variability in the estimated survival rate based on factors that include initiation of pre-hospital care and nature of injury.[7]
Many patients who survive traumatic cardiac arrest may develop long-term neurological damage resulting from lack of circulation to the nervous system during the arrest. This damage may range from moderate disability to a persistent vegetative state. A 2012 review suggests that while survival rates of traumatic cardiac arrest are higher in children, so is the incidence of neurological complication.[8]
References
- ↑ "Emergency thoracotomy in thoracic trauma-a review". Injury 37 (1): 1–19. January 2006. doi:10.1016/j.injury.2005.02.014. PMID 16410079.
- ↑ "Cardiopulmonary resuscitation traumatic cardiac arrest--there are survivors. An analysis of two national emergency registries". Critical Care 15 (6): R276. 2011. doi:10.1186/cc10558. PMID 22108048.
- ↑ 3.0 3.1 3.2 Lockey, David J.; Lyon, Richard M.; Davies, Gareth E. (June 2013). "Development of a simple algorithm to guide the effective management of traumatic cardiac arrest" (in en). Resuscitation 84 (6): 738–742. doi:10.1016/j.resuscitation.2012.12.003. PMID 23228555.
- ↑ 4.0 4.1 4.2 4.3 "Traumatic Cardiac Arrest" (in en). 2015-12-10. http://www.emdocs.net/traumatic-cardiac-arrest/.
- ↑ 5.0 5.1 5.2 5.3 5.4 Smith, Jason E; Rickard, Annette; Wise, David (January 2015). "Traumatic cardiac arrest" (in en). Journal of the Royal Society of Medicine 108 (1): 11–16. doi:10.1177/0141076814560837. ISSN 0141-0768. PMID 25572990.
- ↑ Lockey, David; Crewdson, Kate; Davies, Gareth (September 2006). "Traumatic Cardiac Arrest: Who Are the Survivors?" (in en). Annals of Emergency Medicine 48 (3): 240–244. doi:10.1016/j.annemergmed.2006.03.015. PMID 16934644. https://linkinghub.elsevier.com/retrieve/pii/S0196064406004124.
- ↑ Barnard, Ed; Yates, David; Edwards, Antoinette; Fragoso-Iñiguez, Marisol; Jenks, Tom; Smith, Jason E. (January 2017). "Epidemiology and aetiology of traumatic cardiac arrest in England and Wales — A retrospective database analysis" (in en). Resuscitation 110: 90–94. doi:10.1016/j.resuscitation.2016.11.001. PMID 27855275. https://linkinghub.elsevier.com/retrieve/pii/S030095721630538X.
- ↑ Zwingmann, Jörn; Mehlhorn, Alexander T; Hammer, Thorsten; Bayer, Jörg; Südkamp, Norbert P; Strohm, Peter C (2012). "Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: a systematic review" (in en). Critical Care 16 (4): R117. doi:10.1186/cc11410. ISSN 1364-8535. PMID 22770439.
 |