Medicine:Asystole
| Asystole | |
|---|---|
| Other names | Cardiac flatline, asystolic arrest |
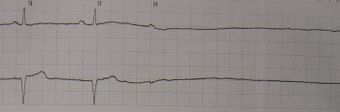 | |
| A rhythm strip showing two beats of normal sinus rhythm followed by an atrial beat and asystole | |
| Pronunciation | |
Asystole (New Latin, from Greek privative a "not, without" + systolē "contraction"[1][2]) is the absence of ventricular contractions in the context of a lethal heart arrhythmia (in contrast to an induced asystole on a cooled patient on a heart-lung machine and general anesthesia during surgery necessitating stopping the heart). Asystole is the most serious form of cardiac arrest and is usually irreversible. Also referred to as cardiac flatline, asystole is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.
Asystole should not be confused with very brief pauses below 3 seconds in the heart's electrical activity that can occur in certain less severe abnormal rhythms. Asystole is different from very fine occurrences of ventricular fibrillation, though both have a poor prognosis, and untreated fine VF will lead to asystole. Faulty wiring, disconnection of electrodes and leads, and power disruptions should be ruled out.
Asystolic patients (as opposed to those with a "shockable rhythm" such as coarse or fine ventricular fibrillation, or unstable ventricular tachycardia that is not producing a pulse, which can potentially be treated with defibrillation) usually present with a very poor prognosis. Asystole is found initially in only about 28% of cardiac arrest cases in hospitalized patients,[3] but only 15% of these survive, even with the benefit of an intensive care unit, with the rate being lower (6%) for those already prescribed drugs for high blood pressure.[4]
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline).[5] Sometimes an underlying reversible cause can be detected and treated (the so-called "Hs and Ts", an example of which is hypokalaemia). Several interventions previously recommended—such as defibrillation (known to be ineffective on asystole, but previously performed in case the rhythm was actually very fine ventricular fibrillation) and intravenous atropine—are no longer part of the routine protocols recommended by most major international bodies.[6] 1 mg epinephrine by IV every 3–5 minutes is given for asystole.[7]
Survival rates in a cardiac arrest patient with asystole are much lower than a patient with a rhythm amenable to defibrillation; asystole is itself not a "shockable" rhythm. Even in those cases where an individual suffers a cardiac arrest with asystole and it is converted to a less severe shockable rhythm (ventricular fibrillation, or ventricular tachycardia), this does not necessarily improve the person's chances of survival to discharge from the hospital, though if the case was witnessed by a civilian, or better, a paramedic, who gave good CPR and cardiac drugs, this is an important confounding factor to be considered in certain select cases.[8] Out-of-hospital survival rates (even with emergency intervention) are less than 2 percent.[9]
Cause
Possible underlying causes, which may be treatable and reversible in certain cases, include the Hs and Ts.[10][11][12]
- Hypovolemia
- Hypoxia
- Hydrogen ions (acidosis)
- Hypothermia
- Hyperkalemia or hypokalemia
- Toxins (e.g. drug overdose)
- Cardiac tamponade
- Tension pneumothorax
- Thrombosis (myocardial infarction or pulmonary embolism)
While the heart is asystolic, there is no blood flow to the brain unless CPR or internal cardiac massage (when the chest is opened and the heart is manually compressed) is performed, and even then it is a small amount. After many emergency treatments have been applied but the heart is still unresponsive, it is time to consider pronouncing the patient dead. Even in the rare case that a rhythm reappears, if asystole has persisted for fifteen minutes or more, the brain will have been deprived of oxygen long enough to cause severe hypoxic brain damage, resulting in brain death or persistent vegetative state.[13]
-
ECG lead showing asystole (flatline)
-
Asystole
-
Ventricular fibrillation
See also
- Agonal heart rhythm
- Ictal asystole
References
- ↑ Harper, Douglas. "asystole". Online Etymology Dictionary. https://www.etymonline.com/?term=asystole.
- ↑ συστολή. Liddell, Henry George; Scott, Robert; A Greek–English Lexicon at the Perseus Project.
- ↑ Baldzizhar, Aksana; Manuylova, Ekaterina; Marchenko, Roman; Kryvalap, Yury; Carey, Mary G. (September 2016). "Ventricular Tachycardias". Critical Care Nursing Clinics of North America 28 (3): 317–329. doi:10.1016/j.cnc.2016.04.004. PMID 27484660.
- ↑ Kutsogiannis, Demetrios J.; Bagshaw, Sean M.; Laing, Bryce; Brindley, Peter G. (4 October 2011). "Predictors of survival after cardiac or respiratory arrest in critical care units". CMAJ: Canadian Medical Association Journal 183 (14): 1589–1595. doi:10.1503/cmaj.100034. PMID 21844108.
- ↑ Kempton, Hannah; Vlok, Ruan; Thang, Christopher; Melhuish, Thomas; White, Leigh (March 2019). "Standard dose epinephrine versus placebo in out of hospital cardiac arrest: A systematic review and meta-analysis". The American Journal of Emergency Medicine 37 (3): 511–517. doi:10.1016/j.ajem.2018.12.055. PMID 30658877.
- ↑ Neumar, R. W.; Otto, C. W.; Link, M. S.; Kronick, S. L.; Shuster, M.; Callaway, C. W.; Kudenchuk, P. J.; Ornato, J. P. et al. (17 October 2010). "Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation 122 (18_suppl_3): S729–S767. doi:10.1161/CIRCULATIONAHA.110.970988. PMID 20956224.
- ↑ Jordan, Matthew; Lopez, Richard; Morrisonponce, Daphne (2022) (in en). Asystole. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430866/.
- ↑ Thomas, Andrew; Newgard, Craig; Fu, Rongwei; Zive, Dana; Daya, Mohamud (2013). "Survival in Out-of-Hospital Cardiac Arrests with Initial Asystole or Pulseless Electrical Activity and Subsequent Shockable Rhythms". Resuscitation 84 (9): 1261–1266. doi:10.1016/j.resuscitation.2013.02.016. PMID 23454257.
- ↑ "Medical Futility in Asystolic Out-of-Hospital Cardiac Arrest". Survey of Anesthesiology 52 (5): 261–262. October 2008. doi:10.1097/01.SA.0000318635.97636.a6.
- ↑ Mazur G (2004). ACLS: Principles And Practice. Dallas: American Heart Association. pp. 71–87. ISBN 978-0-87493-341-3.
- ↑ ACLS for experienced providers. Dallas: American Heart Association. 2003. pp. 3–5. ISBN 978-0-87493-424-3. https://archive.org/details/aclsforexperienc00amer_0/page/3.
- ↑ ECC Committee, Subcommittees and Task Forces of the American Heart Association (December 2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care – Part 7.2: Management of Cardiac Arrest". Circulation 112 (24 Suppl): IV1–203 (7.2 IV58–66). doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375.
- ↑ Shah, Sandy (16 October 2021). Asystole: Background, Pathophysiology, Etiology. https://emedicine.medscape.com/article/757257-overview#a2.
External links
| Classification |
|---|
 |


