Biology:Salmonella enterica subsp. enterica
| Salmonella enterica subsp. enterica | |
|---|---|
| |
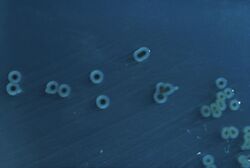
| Salmonella Typhimurium colonies on a Hektoen enteric agar plate | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Gammaproteobacteria |
| Order: | Enterobacterales |
| Family: | Enterobacteriaceae |
| Genus: | Salmonella |
| Species: | |
| Subspecies: | S. e. subsp. enterica
|
| Trinomial name | |
| Salmonella enterica subsp. enterica | |
Salmonella enterica subsp. enterica is a subspecies of Salmonella enterica, the rod-shaped, flagellated, aerobic, Gram-negative bacterium. Many of the pathogenic serovars of the S. enterica species are in this subspecies, including that responsible for typhoid.[1]
Serovars
Salmonella enterica subsp. enterica serovars are defined based on their somatic (O) and flagellar (H) antigens, with over 2,600 serovars in total; only about 50 of these serovars are common causes of infections in humans.[2] Most of these serovars are found in the environment and survive in plants, water, and soil; many serovars have broad host ranges that allow them to colonize different species in mammals, birds, reptiles, amphibians, and insects. Zoonotic diseases, like Salmonella, spread between the environment and people.[3]
A number of techniques are currently used to differentiate between serotypes. These include looking for the presence or absence of antigens, phage typing, molecular fingerprinting and biotyping, where serovars are differentiated by which nutrients they are able to ferment. A possible factor in determining the host range of particular serovars is phage-mediated acquisition of a small number of genetic elements that enable infection of a particular host.[4] It is further postulated that serovars which infect a narrow range of species have diverged from ancestors with a broad host range, and have since specialised and lost the ability to infect some hosts.[5]
The CDC publishes a Salmonella Annual Report with a list of serovars most commonly associated with human illness, the top 10 serovars are listed below:[6]
| Rank | Serotype | Percent |
|---|---|---|
| 1 | Enteritidis | 16.8 |
| 2 | Newport | 10.1 |
| 3 | Typhimurium | 9.8 |
| 4 | Javiana | 5.8 |
| 5 | I 4,[5],12:i:- | 4.7 |
| 6 | Infantis | 2.7 |
| 7 | Muenchen | 2.6 |
| 8 | Montevideo | 2.2 |
| 9 | Braenderup | 2.1 |
| 10 | Thompson | 1.7 |
| - | Other | 41.5 |
Studies have concluded most strains of Salmonella enterica subsp. enterica serovars possess serotype-specific virulence plasmids. These are plasmid-associated virulence characterized by low-copy-number plasmids and depending on the serovar, its size ranges from 50 to 100 kb.[7] In 2012, CDC's PulseNet became aware of a emergent multi-drug resistant Serovar Infantis SNP cluster, named REPJFX01. This SNP cluster has a large megaplasmid (pESI) that contains multiple drug-resistance genes.[8] The USDA NARMS stated that because of this pESI-plasmid, serovar Infantis is the leading serovar in poultry.[9] NCBI has over 12,500 isolates in the REPJFX01 SNP cluster, with over 3,700 being clinical isolates.[10] Serovar Enteritidis, which is the most common serovar isolated in human clinical cases, has also been found to produce endotoxins, coded by the stn and slyA genes, that attribute to the pathogenicity of Enteritidis.[11]
In November 2016, a new strain of extensively drug resistant (XDR) Salmonella enterica serovar Typhi emerged in Pakistan, primarily from the cities of Hyderabad and Karachi.[12] Multidrug resistant strains have been present since the late 1970s in Africa and Asia.[13] These XDR strains are resistant to all antibiotic treatment options: chloramphenicol, ampicillin, trimethoprim-sulfamethoxazole, fluoroquinolones, and third-generation cephalosporins. The outbreak has been ongoing since 2016.[14]
Nomenclature
The nomenclature of Salmonella enterica has long been a topic of debate in the microbiology community.[15] Originally in the 1880s, Salmonella species were named after the disease, host, or geological location they were associated with; however, this taxonomic characterization was contested due to genus members being categorized incompatibly with their genetic similarities. In the 1980s, the emergence of nucleotide sequencing and DNA hybridization led many established bacteriologists such as Le Minor and Popoff (1987), Euzéby (1999), and Ezaki and Yabuuchi (2000) to put forth their proposals for nomenclature changes.[16] It was not until 2005, that Le Minor and Popoff reproposed and established that "Salmonella enterica" would be the approved species name – excluding Salmonella bongori – and that Salmonella enterica contains six subspecies, of which Salmonella enterica subsp. enterica contains the most serovars.[17] Technological advancements allow researchers to use whole genome sequencing data to identify and group serovars using two methods: sequence typing and antigen recognition.[18]
Serovar names are capitalized but not italicized or underlined. Serovars may be designated in full form or short form (includes just the genus and serovar names). For example, in full designation Salmonella enterica subsp. enterica serovar Typhi is written as such, but in short designation it is written as Salmonella Typhi.[19] Each serovar can have many strains, as well, which allows for a rapid increase in the total number of antigenically variable bacteria.[20]
Epidemiology
The World Health Organization characterizes salmonellosis as a foodborne disease whose symptoms include diarrhea, fever, nausea, vomiting, and in severe cases death.[21] Salmonellosis has been assessed to primarily occur in human hosts due to bacterial colonization of the intestinal tract after the consumption of contaminated food or water, but it is also known to spread from person-to-person via the fecal-oral route.[22] To reduce the risk associated with contracting this disease, proper food safety measures should be applied to high-risk food products including poultry, beef, pork, lamb, eggs, and fresh produce.[23] Food manufacturers, ingredient suppliers, restaurants, and home cooks should practice sanitary processing procedures, store foods below 5 °C, and thoroughly cook all foods to their designated safe-to-eat temperatures.[23] It has become increasingly difficult to mitigate the presence of salmonellosis infections across the human population due to the unique nature of multidrug-resistant serovars as a result of the counterproductive effects to use antibiotics as a broad spectrum treatment.[24] Key host immune deficiencies associated with HIV, malaria and malnutrition have contributed to a wide spread of this disease and the need to use expensive antimicrobial drugs in the poorest health services in the world.[25] But also bacterial factors, such as upregulated activity of the virulence gene pgtE, due to a single nucleotide polymorphism (SNP) in its promoter region, have been shown to have a great impact upon the pathogenesis of this particular Salmonella sequence type.[26]
Survival and stress
There are factors that can decrease the infection risk. These include a higher pH in the stomach, gastric resection, and treatment with anti acid buffering.[27] If the stomach has a lower pH, then this helps as a defensive technique to potentially fight off this infection.[28]
This strain is mesophilic and some can survive extremely low or high temperatures which can range from 2 °C – 54 °C.[29] Sigma factors inside the cell control the gene expression and they can sense the changes in the environment from the outer membrane by activation of genes that then respond to heat stress and adapt accordingly.[30] S. enterica also can quickly respond to cold temperatures by cold shock proteins (CSP) by synthesizing themselves so that the cell can later resume growth.[31] Chlorine can be a chemical stressor to S. enterica because once chlorine is present, S. enterica can produce a biofilm that provides itself with a exopolysaccharide matrix that has the ability of a chemical attack against chlorine.[32] From this, chlorine has preventative measures for biofilm formation in poultry drinking systems and this reduces the risk of S. enterica.[33] Successful adaptation allows S. enterica to withstand more acidic conditions, counteracting stomach antibacterial effects.[34]
References
- ↑ Medical Microbiology (6th ed.). Philadelphia, PA: Mosby Elsevier. 2009. p. 307.
- ↑ "Antigenic formulae of the Salmonella serovars". WHO Collaborating Centre for Reference and Research on Salmonella 9: 1–66. November 2007. https://www.academia.edu/20495783.
- ↑ "One Health and Food-Borne Disease: Salmonella Transmission between Humans, Animals, and Plants". Microbiology Spectrum 2 (1): OH-0020-2013. February 2014. doi:10.1128/microbiolspec.OH-0020-2013. PMID 26082128.
- ↑ "Salmonella enterica serotype Typhimurium and its host-adapted variants". Infection and Immunity 70 (5): 2249–2255. May 2002. doi:10.1128/IAI.70.5.2249-2255.2002. PMID 11953356.
- ↑ "Patterns of genome evolution that have accompanied host adaptation in Salmonella". Proceedings of the National Academy of Sciences of the United States of America 112 (3): 863–868. January 2015. doi:10.1073/pnas.1416707112. PMID 25535353. Bibcode: 2015PNAS..112..863L.
- ↑ "National Enteric Disease Surveillance: Salmonella Annual Report, 2016". 2016. https://www.cdc.gov/nationalsurveillance/pdfs/2016-Salmonella-report-508.pdf.
- ↑ "The virulence plasmids of Salmonella". International Microbiology 2 (3): 177–184. September 1999. PMID 10943411. https://core.ac.uk/download/pdf/159083976.pdf.
- ↑ CDC (2023-07-21). "Persistent Strain of Salmonella Infantis (REPJFX01) Linked to Chicken" (in en-us). https://www.cdc.gov/ncezid/dfwed/outbreak-response/rep-strains/repjfx01.html.
- ↑ "FSIS NARMS Multi-Year Report – 2014-2019". 2023-02-10. https://www.fsis.usda.gov/news-events/publications/fsis-narms-multi-year-report-2014-2019.
- ↑ "Isolates Browser - Pathogen Detection - NCBI". https://www.ncbi.nlm.nih.gov/pathogens/isolates/#PNUSAS212095.
- ↑ "Quantitative analysis and partial characterization of cytotoxin production by Salmonella strains". Infection and Immunity 56 (12): 3089–3094. December 1988. doi:10.1128/iai.56.12.3089-3094.1988. PMID 3182072.
- ↑ "Typhoid Outbreak in Pakistan Linked to Extensively Drug-Resistant Bacteria" (in en). 21 February 2018. https://www.the-scientist.com/the-nutshell/typhoid-outbreak-in-pakistan-linked-to-extensively-drug-resistant-bacteria-30090.
- ↑ "Emergence of an Extensively Drug-Resistant Salmonella enterica Serovar Typhi Clone Harboring a Promiscuous Plasmid Encoding Resistance to Fluoroquinolones and Third-Generation Cephalosporins". mBio 9 (1). February 2018. doi:10.1128/mBio.00105-18. PMID 29463654.
- ↑ "Extensively Drug-Resistant Typhoid Fever in Pakistan – Alert – Level 2, Practice Enhanced Precautions" (in en-us). Travel Health Notices. U.S. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/notices/alert/xdr-typhoid-fever-pakistan.
- ↑ "Salmonella: clinical importance and evolution of nomenclature". Chang Gung Medical Journal 30 (3): 210–219. 2007. PMID 17760271. http://cgmj.cgu.edu.tw/3003/300302.pdf.
- ↑ "Evolution of Salmonella nomenclature: a critical note". Folia Microbiologica 56 (6): 497–503. November 2011. doi:10.1007/s12223-011-0075-4. PMID 22052214.
- ↑ "Salmonella nomenclature". Journal of Clinical Microbiology 38 (7): 2465–2467. July 2000. doi:10.1128/JCM.38.7.2465-2467.2000. PMID 10878026.
- ↑ "Salmonella nomenclature in the genomic era: a time for change". Scientific Reports 11 (1): 7494. April 2021. doi:10.1038/s41598-021-86243-w. PMID 33820940. Bibcode: 2021NatSR..11.7494C.
- ↑ "Scientific Nomenclature". Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/eid/page/scientific-nomenclature.
- ↑ "Salmonella spp. comparative sequencing". Wellcome Trust Genome Campus. https://web.archive.org/web/20071114165837/http://www.sanger.ac.uk/Projects/Salmonella/.
- ↑ "Salmonella (non-typhoidal)" (in en). https://www.who.int/news-room/fact-sheets/detail/salmonella-(non-typhoidal).
- ↑ Giannella, Ralph A. (1996), Baron, Samuel, ed., "Salmonella", Medical Microbiology (Galveston (TX): University of Texas Medical Branch at Galveston), ISBN 978-0-9631172-1-2, PMID 21413334, http://www.ncbi.nlm.nih.gov/books/NBK8435/, retrieved 2023-10-26
- ↑ 23.0 23.1 Ehuwa O, Jaiswal AK, Jaiswal S. Salmonella, food safety and food handling practices. Foods. 2021;10(5). doi:https://www.mdpi.com/2304-8158/10/5/907/htm
- ↑ Glynn, M. Kathleen; Bopp, Cheryl; Dewitt, Wallis; Dabney, Paul; Mokhtar, Mohammad; Angulo, Frederick J. (May 7, 1998). "Emergence of Multidrug-Resistant Salmonella enterica SerotypeTyphimurium DT104 Infections in the United States". New England Journal of Medicine 338 (19): 1333–1339. doi:10.1056/NEJM199805073381901. PMID 9571252.
- ↑ "Invasive non-typhoidal salmonella disease: an emerging and neglected tropical disease in Africa". Lancet 379 (9835): 2489–2499. June 2012. doi:10.1016/s0140-6736(11)61752-2. PMID 22587967.
- ↑ "Role of a single noncoding nucleotide in the evolution of an epidemic African clade of Salmonella". Proceedings of the National Academy of Sciences of the United States of America 115 (11): E2614–E2623. March 2018. doi:10.1073/pnas.1714718115. PMID 29487214. Bibcode: 2018PNAS..115E2614H.
- ↑ Garcia del Portillo, F., J.W. Foster and B.B. Finlay. 1993. The role of acid tolerance response genes in Salmonella typhimurium virulence. Infection and Immunity 61:4489- 4492
- ↑ Foster, J.W. and H.K. Hall. 1990. Adaptive acidification tolerance response of Salmonella typhimurium. Journal of Bacteriology 173:771 -778
- ↑ M. J. Kazmierczak, M. Wiedmann, and K. J. Boor, "Alternative sigma factors and their roles in bacterial virulence," Microbiology and Molecular Biology Reviews, vol. 69, no. 4, pp. 527–543, 2005
- ↑ M. P. Spector and W. J. Kenyon, "Resistance and survival strategies of Salmonella enterica to environmental stresses," Food Research International, vol. 45, no. 2, pp. 455–481, 2012
- ↑ J. E. Craig, D. Boyle, K. P. Francis, and M. P. Gallagher, "Expression of the cold-shock gene cspB in Salmonella typhimurium occurs below a threshold temperature," Microbiology, vol. 144, no. 3, pp. 697–704, 1998
- ↑ G. McDonnell and A. D. Russell, "Antiseptics and disinfectants: activity, action, and resistance," Clinical Microbiology Reviews, vol. 12, no. 1, pp. 147–179, 1999
- ↑ J. A. Byrd, J. R. DeLoach, D. E. Corrier, D. J. Nisbet, and L. H. Stanker, "Evaluation of Salmonella serotype distributions from commercial broiler hatcheries and grower houses," Avian Diseases, vol. 43, no. 1, pp. 39–47, 1999
- ↑ I. Rychlik and P. A. Barrow, "Salmonella stress management and its relevance to behaviour during intestinal colonisation and infection," FEMS Microbiology Reviews, vol. 29, no. 5, pp. 1021–1040, 2005
Wikidata ☰ Q21600865 entry
 |

