Medicine:RAS-associated autoimmune leukoproliferative disorder
| RAS-associated autoimmune leukoproliferative disorder | |
|---|---|
| Other names | Autoimmune lymphoproliferative syndrome type 4 |
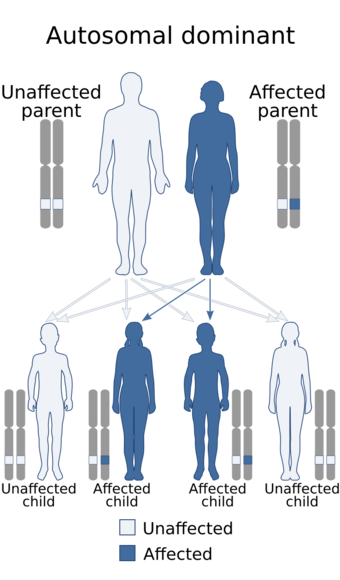 | |
| This condition is inherited in an autosomal recessive manner | |
RAS-associated autoimmune leukoproliferative disorder (RALD) is a rare genetic disorder of the immune system. RALD is characterized by lymphadenopathy, splenomegaly, autoimmunity, and elevation in granulocytes and monocytes. It shares many features with autoimmune lymphoproliferative syndrome and is caused by somatic mutations in NRAS or KRAS. This was first described by investigators João Oliveira and Michael Lenardo from the National Institutes of Health.[1]
Presentation
Clinically, RALD is characterized by splenomegaly, a relatively mild degree of peripheral lymphadenopathy, and autoimmunity. The autoimmune phenotype can present in childhood or adulthood and primarily includes autoimmune hemolytic anemia, ITP, and neutropenia. Some patients have a history of recurrent respiratory tract infections. It is unclear if increased risk for malignancy is part of RALD.[citation needed]
Importantly, however, the clinical and laboratory phenotype resembles juvenile myelomonocytic leukemia. The high fatality rate of this childhood blood cancer puts it in sharp contrast when compared to the relatively benign and chronic course of RALD. Approximately 15-30% of patients diagnosed with JMML have somatic, activating RAS mutations.[2][3] However, due to the difficulty in distinguishing JMML from RALD, it is possible a subset of patients treated for JMML actually have RALD and could therefore avoid the aggressive JMML treatment. This distinction is under investigation.[4]
Genetics
RALD is caused by gain-of-function somatic mutations in the genes NRAS or KRAS. NRAS and KRAS are members of the RAS subfamily and are implicated in many types of cancer.[5] Somatic mutations are changes in DNA that occur after conception. Although generally somatic mutations can develop in any cell of the body, in RALD the somatic mutations only reside in the blood cells. Because these mutations are acquired and not in the germline, they cannot be inherited or passed on to children.[citation needed]
Function
Somatic RAS mutations greatly diminish the GTPase activity within the cell. The reduced GTPase activity locks the cells in an activated state and degrades the pro-apoptotic BIM protein, thus making the cells resistant to apoptosis. In contrast to ALPS, this apoptosis defect does not involve the FAS pathway.[6][7][8][9][10]
Diagnosis
RALD patients show normal to modestly decreased total lymphocytes, mild to no elevation in αβ-double negative T cells, a relative expansion of B cells, and elevated granulocytes and monocytes. The absolute or relative monocytosis in particular is an important characteristic of this disorder and help differentiate it from ALPS. Autoantibodies are also common.[7][8][9][10]
Management
Research
Investigators at the National Institute of Allergy and Infectious Diseases at the US National Institutes of Health currently have clinical protocols to study new approaches to the diagnosis and treatment of this disorder.[11]
References
- ↑ Oliveira JB; Bidère N; Niemela JE; Zheng L; Sakai K; Nix CP; Danner RL; Barb J et al. (2007). "NRAS mutation causes a human autoimmune lymphoproliferative syndrome". Proc. Natl. Acad. Sci. USA 104 (21): 8953–8958. doi:10.1073/pnas.0702975104. PMID 17517660. Bibcode: 2007PNAS..104.8953O.
- ↑ Flotho C; Valcamonica S; Mach-Pascual S; Schmahl G; Corral L; Ritterbach J; Hasle H; Aricò M et al. (1999). "RAS mutations and clonality analysis in children with juvenile myelomonocytic leukemia (JMML)". Leukemia 13 (1): 32–37. doi:10.1038/sj.leu.2401240. PMID 10049057.
- ↑ Flotho C; Kratz C; Niemeyer CM (2007). "Targeting RAS Signaling Pathways in Juvenile Myelomonocytic Leukemia". Current Drug Targets 8 (6): 715–725. doi:10.2174/138945007780830773. PMID 17584027.
- ↑ Calvo, K. R.; Price, S.; Braylan, R. C.; Oliveira, J. B.; Lenardo, M.; Fleisher, T. A.; Rao, V. K. (2015). "JMML and RALD (Ras-associated autoimmune leukoproliferative disorder): common genetic etiology yet clinically distinct entities". Blood 125 (18): 2753–2758. doi:10.1182/blood-2014-11-567917. ISSN 0006-4971. PMID 25691160.
- ↑ "NEUROBLASTOMA RAS VIRAL ONCOGENE HOMOLOG; NRAS". OMIM. http://omim.org/entry/164790. Retrieved 8 April 2014.
- ↑ de Vos AM et al. (1988). "Three-dimensional structure of an oncogene protein: catalytic domain of human c-H-ras p21". Science 239 (888–893): 888–93. doi:10.1126/science.2448879. PMID 2448879. Bibcode: 1988Sci...239..888D.
- ↑ 7.0 7.1 Fleisher TA; Oliveira JB (2012). "Monogenic defects in lymphocyte apoptosis". Current Opinion in Allergy and Clinical Immunology 12 (6): 609–615. doi:10.1097/ACI.0b013e3283588da0. PMID 22918222.
- ↑ 8.0 8.1 Niemela JE; Lu L; Fleisher TA; Davis J; Caminha I; Natter M; Beer LA; Dowdell KC et al. (2011). "Somatic KRAS mutations associated with a human nonmalignant syndrome of autoimmunity and abnormal leukocyte homeostasis". Blood 117 (10): 2883–2886. doi:10.1182/blood-2010-07-295501. PMID 21079152.
- ↑ 9.0 9.1 Oliveira JB (2013). "The expanding spectrum of the autoimmune lymphoproliferative syndromes". Current Opinion in Pediatrics 25 (6): 722–729. doi:10.1097/mop.0000000000000032. PMID 24240292.
- ↑ 10.0 10.1 Takagi, M.; Shinoda, K.; Piao, J.; Mitsuiki, N.; Takagi, M.; Matsuda, K.; Muramatsu, H.; Doisaki, S. et al. (2010). "Autoimmune lymphoproliferative syndrome-like disease with somatic KRAS mutation". Blood 117 (10): 2887–2890. doi:10.1182/blood-2010-08-301515. ISSN 0006-4971. PMID 21063026.
- ↑ http://www.clinicaltrials.gov, study ID NCT00246857, NCT00001467, and others
External links
| Classification | |
|---|---|
| External resources |
 |

