Biology:Cervical collar
| Cervical collar | |
|---|---|
 A side view of a person wearing a C spine collar. |
A cervical collar, also known as a neck brace, is a medical device used to support and immobilize a person's neck. It is also applied by emergency personnel to those who have had traumatic head or neck injuries,[1] and can be used to treat chronic medical conditions.
Whenever people have a traumatic head or neck injury, they may have a cervical fracture. This makes them at high risk for spinal cord injury, which could be exacerbated by movement of the person and could lead to paralysis or death. A common scenario for this injury would be a person suspected of having whiplash because of a car accident.[2] In order to prevent further injury, such people may have a collar placed by medical professionals until X-rays can be taken to determine if a cervical spine fracture exists.[3] Medical professionals will often use the NEXUS criteria and/or the Canadian C-spine rules to clear a cervical collar and determine the need for imaging. The cervical collar only stabilizes the top seven vertebrae, C1 through C7. (Other immobilizing devices such as a Kendrick Extrication Device or a backboard can be used to stabilize the remainder of the spinal column.[1])
The routine use of a cervical collar by a first aid provider is not recommended.[4]
Cervical collars are also used therapeutically to help realign the spinal cord and relieve pain,[5] although they are usually not worn for long periods of time.[6] Another use of the cervical collar is for strains, sprains, or whiplash.[2][3] If pain is persistent, the collar might be required to remain attached to help in the healing process.[3][5] A person may also need a cervical collar, or may require a halo fixation device to support the neck during recovery after surgery such as cervical spinal fusion.[7]
Types
A soft collar is fairly flexible and is the least limiting but can carry a high risk of further breakage, especially in people with osteoporosis. They are usually made of felt. It can be used for minor injuries or after healing has allowed the neck to become more stable.[citation needed]
A range of manufactured rigid collars are also used, usually comprising (a) a firm plastic bi-valved shell secured with Velcro straps and (b) removable padded liners. The also contain a back pad, back panel, front pad, front panel, and chin pad. There is are air holes throughout the device to provide ventilation to the area but also to allow access for a tracheostomy if needed. The rigidness is provided by plexiglass in some models. The most frequently prescribed are the Aspen, Malibu, Miami J, and Philadelphia collars. All these can be used with additional chest and head extension pieces to increase stability.[citation needed]
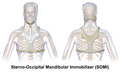
Cervical collars are incorporated into rigid braces that constrain the head and chest together.[8] Examples include the Sterno-Occipital Mandibular Immobilization Device (SOMI), Lerman Minerva and Yale types. Special cases, such as very young children or non-cooperative adults, are sometimes still immobilized in medical plaster of paris casts, such as the Minerva cast.
Rigid collars are most restrictive when flexing the neck and least restrictive with lateral rotation when compared to soft collars.[9] Despite this, subjects have similar range of motion when asked to perform activities of daily living. It is thought that these collars provide a proprioceptive guide on how much to move one's neck and when patients are preoccupied with performing an activity they are able to move their neck more.[10] This is why in more minor injuries, cervical collars are still placed to remind patients of their injury so they can restrict any activities that may worsen their condition.
Application and care
When applying a cervical collar, it must be tight enough to immobilize the neck but must be loose enough to avoid pressure on the vasculature of the neck, strangulation, and pressure ulcers. Ideally, any clothing or jewelry in the neck area should be removed before applying the collar. Next, a collar size must be chosen according to the patient's size and build. The practitioner will then measure the length of the neck. The collar is then placed by one practitioner while the other holds the neck still. Then, the collar should be locked to the ideal neck length according to the specific manufacturer's manual. The chin must be in the chin piece and the collar must extend down to the sternal notch. If the patient has a tracheostomy hole, medical professionals must assure that the hole is midline and accessible in a patient with a cervical collar. Some common errors include incorrect chosen collar size, incorrect technique in placing collar, and incorrect measurement of neck length. [11]
Cervical collars and patient's necks should be evaluated and cleaned frequently for hygienic purposes as well as to avoid pressure ulcers. When the neck area is being cleaned, it is again important for two people to help remove the collar. One person must help hold the neck and keep it aligned while the other unfastens the straps and removes the collar. The area is then cleaned with soap, water, and washcloths. If there is evidence of skin breakdown, other topical agents and even antibiotics may be used if there is evidence of infection as well.[12]
History
The cervical collar was invented in 1966 by George Cottrell during the Vietnam war as a way to provide neck immobilization in American soldiers with potential unstable neck injuries.[13] Its use in the prehospital setting in the United States was popularized by orthopedic surgeon, Dr. JD Farrington. In his paper, "Death in a Ditch", Farrington described seeing "sloppy and inefficient removal of victim[s] from their vehicle." He explained how a standardized approach of applying cervical collars before extracting motor vehicle collision victims from their vehicles is necessary to prevent this. [14]
Use over time
As a result of several small randomized clinical trials over the last decade, hospitals and ambulance staff have seen a significant reduction in the number of patients that are being immobilized.[15][16] This has been due to complications such as increased intracranial pressure with traumatic brain injury, along with access issues for airway management in obtunded patients.[17] Other risks and complications include increased testing and imaging, increased incidence in displacement of spinal fractures in the elderly, limited physical examination of patients, neck pain, pressure ulcers, and increased length in hospital stay.[18] Because of these potential complications, cervical collars are not recommended in trauma patients with isolated penetrating injury and no neurological deficits.[19] This is because the benefit of a potential secondary cervical injury being prevented with a cervical collar is much less than the risks associated with a cervical collar; with the most concerning being trouble accessing a patient's airway. Some medical professionals have even been calling for a ban on cervical collars, stating that they cause more harm than good.[20] There is also very little evidence that shows cervical collars to be actually making a difference in traumatic cervical spine injury.[citation needed]
Other uses
Cervical collars are used much less commonly for things outside of cervical injury and precaution. These uses include cervical radiculopathy, sleep apnea, and patients on CPAP ventilation. Most studies for these conditions are small scale and limited.[citation needed]
In a 2009 study, it was shown that patients with a confirmed recent diagnosis of cervical radiculopathy who had a cervical collar applied had greater decrease in pain after 6 weeks compared to patients who did not have one applied. When these patients were followed up after six months, almost all of the subjects had complete or near complete resolution of any pain and/or disability, regardless if they had a cervical collar applied or not.[21]
Sleep apnea can be worsened by anterior flexion of the neck or posterior movement of the mandible when sleeping supine. Cervical collars are used to prevent these movements when sleeping in these patients. Small scale studies have failed to show any improvement in oxygenation, snoring, and/or apneic episodes with the use of cervical collars at night. These patients can experience discomfort and feelings of strangulation at night if the collar is not fastened properly.[22] Despite this, some practitioners still apply cervical collars for sleep apnea.[citation needed]
Patients on CPAP ventilation can often have suboptimal positioning due to pain, discomfort, or lack of knowledge. Similarly to patients with sleep apnea, patients on CPAP need optimization of their neck position to keep their airway clear of any obstruction. Specifically, posterior movement of the mandible is to be avoided as to not cause the strap of the CPAP to come off. Also, limited head movement while on CPAP is desired to optimize oxygen flow in and out of the device. Cervical soft collars are used to try to achieve both of these goals. In a small study analyzing the use of cervical collars in patients on CPAP ventilation with a history of sleep apnea, a significant benefit was observed.[23]
Sport
In high-risk motorsports such as Motocross, go-kart racing and speed-boat racing, racers often wear a protective collar to avoid whiplash and other neck injuries.[citation needed]
Designs range from simple foam collars to complex composite devices.[24]
Additional images
See also
- Vertebrae
- Orthotics
- Dental braces
- Orthopedic cast
- Kendrick Extrication Device
- Long spine board
- Halo (medicine)
- Spinal fusion
- Back brace
References
- ↑ 1.0 1.1 Brady Prehospital Emergency Care (6 ed.). Upper Saddle River, NJ: Prentice-Hall. 2000. pp. 662. ISBN 978-0-8359-6064-9. https://archive.org/details/prehospitalemer000hafe/page/662.
- ↑ 2.0 2.1 "Whiplash". WebMD. 14 April 2021. http://www.webmd.com/a-to-z-guides/whiplash.
- ↑ 3.0 3.1 3.2 "Neck Strains". WebMD. http://www.webmd.com/a-to-z-guides/neck-strain.
- ↑ "European Resuscitation Council Guidelines for Resuscitation 2015 Section 9. First aid". Resuscitation 95: 278–287. October 2015. doi:10.1016/j.resuscitation.2015.07.031. PMID 26477417. https://ercguidelines.elsevierresource.com/european-resuscitation-council-guidelines-resuscitation-2015-section-9-first-aid/fulltext.
- ↑ 5.0 5.1 "Physical Therapy and Other Options for Neck Pain". WebMD. 21 April 2021. http://www.webmd.com/a-to-z-guides/physical-therapy-other-options.
- ↑ "Office Ergonomics - Other Treatment for Injuries Related to the Workstation". WebMD. http://women.webmd.com/tc/office-ergonomics-other-treatment-for-injuries-related-to-the-workstation.
- ↑ "Cervical spinal fusion". WebMD. http://www.webmd.com/a-to-z-guides/cervical-spinal-fusion.
- ↑ "Spinal Orthotics". Medscape. 1 November 2018. http://emedicine.medscape.com/article/314921-overview.
- ↑ "The Effect of Soft and Rigid Cervical Collars on Head and Neck Immobilization in Healthy Subjects". Asian Spine Journal 11 (3): 390–395. June 2017. doi:10.4184/asj.2017.11.3.390. PMID 28670406.
- ↑ "Soft and rigid collars provide similar restriction in cervical range of motion during fifteen activities of daily living". Spine 35 (13): 1271–1278. June 2010. doi:10.1097/BRS.0b013e3181c0ddad. PMID 20512025.
- ↑ "Application of Cervical Collars - An Analysis of Practical Skills of Professional Emergency Medical Care Providers". PLOS ONE 10 (11): e0143409. 2015-11-20. doi:10.1371/journal.pone.0143409. PMID 26587650. Bibcode: 2015PLoSO..1043409K.
- ↑ "Cervical Collar: Skin Care Needs of the Patient Wearing a Cervical Collar". Barnes-Jewish Hospital. October 2015. https://www.mnhospitals.org/Portals/0/Documents/patientsafety/PU_Med_dev/Sample_Policy_Cervical_Collar.pdf.
- ↑ , George W."Cervical collar" patent US3285244A, issued 1966-11-15
- ↑ "No place for the rigid cervical collar in pre-hospital care" (in en). https://www.internationaljpp.com/features/article/no-place-for-the-rigid-cervical-collar-in-pre-hospital-care.
- ↑ "No place for the rigid cervical collar in pre-hospital care". International Paramedic Practice 7 (1): 12–15. 2017. doi:10.12968/ippr.2017.7.1.12. ISSN 2052-4889.
- ↑ "Prehospital use of cervical collars in trauma patients: a critical review". Journal of Neurotrauma 31 (6): 531–540. March 2014. doi:10.1089/neu.2013.3094. PMID 23962031.
- ↑ "Cervical spine collar clearance in the obtunded adult blunt trauma patient: a systematic review and practice management guideline from the Eastern Association for the Surgery of Trauma". The Journal of Trauma and Acute Care Surgery 78 (2): 430–441. February 2015. doi:10.1097/ta.0000000000000503. PMID 25757133.
- ↑ "New clinical guidelines on the spinal stabilisation of adult trauma patients - consensus and evidence based". Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 27 (1): 77. August 2019. doi:10.1186/s13049-019-0655-x. PMID 31426850.
- ↑ "Is spinal immobilisation necessary for all patients sustaining isolated penetrating trauma?". Injury 34 (12): 912–914. December 2003. doi:10.1016/S0020-1383(03)00070-6. PMID 14636733.
- ↑ "Cervical collars: probably useless; definitely cause harm!". The Journal of Emergency Medicine 44 (1): e143. January 2013. doi:10.1016/j.jemermed.2012.05.031. PMID 22883718.
- ↑ "PT or cervical collar for cervical radiculopathy?". The Journal of Family Practice 59 (5): 269–272. May 2010. PMID 20544046.
- ↑ "Soft cervical collar in obstructive sleep apnoea: a pilot study". ERJ Open Research 7 (1): 00431–2020. January 2021. doi:10.1183/23120541.00431-2020. PMID 33732743.
- ↑ "Efficacy of the Addition of a Cervical Collar in the Treatment of Persistent Obstructive Apneas Despite Continuous Positive Airway Pressure". Journal of Clinical Sleep Medicine 13 (12): 1473–1476. December 2017. doi:10.5664/jcsm.6852. PMID 28728616.
- ↑ "Valhalla Adult 360 Plus Device Karting Neck Brace". http://www.valhallaracing.com/360Plus2.cfm.
 |