Biology:Neisseria flavescens
| Neisseria flavescens | |
|---|---|
| |
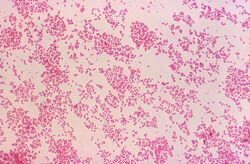
| A gram stain of Neisseria flavescens provided by CDC/Dr. W. A. Clark | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Betaproteobacteria |
| Order: | Neisseriales |
| Family: | Neisseriaceae |
| Genus: | Neisseria |
| Species: | N. flavescens
|
| Binomial name | |
| Neisseria flavescens Branham 1930[1]
| |
Neisseria flavescens was first isolated from cerebrospinal fluid in the midst of an epidemic meningitis outbreak in Chicago.[2] These gram-negative, aerobic bacteria reside in the mucosal membranes of the upper respiratory tract, functioning as commensals.[3] However, this species can also play a pathogenic role in immunocompromised and diabetic individuals.[4] In rare cases, it has been linked to meningitis, pneumonia, empyema, endocarditis, and sepsis.
Morphology
These bacteria are gram-negative and diplococcus, rendering them virtually indistinguishable from the other Neisseria species.[2] Yet, Neisseria flavescens remains distinct due to its signature pigmented colonies, yellow-gold in color.[5] And it is through this yellow-gold color that this bacteria earned its name, with flavescens precisely translating as "becoming a golden yellow."[2] This pigmentation also indicates N. flavescens' similarity to saccharolytic Neisseria species, which also exhibit pigmentation.[6] In addition, these pigmented species differ from meningococcus, which lack pigmentation.[2]
Biochemical processes
Similar to saccharolytic species, N. flavescens strains are capable of producing polysaccharides from sucrose and are colistin-susceptible.[6] This bacteria is also catalase and oxidase positive.[3] It is not capable of acid-production from glucose, maltose, fructose, sucrose, mannose, or lactose, in contrast to meningococcus, which are active-fermenters.[2] Furthermore, fundamental differences between these two species are again shown, as serological testing reveals N. flavescens' lack of cross-agglutination.[2] At the same time, biochemical testing distinguishes Neisseria flavescens from other gram-negative diplococci, with N. flavescens being DNase negative, weakly positive to Superoxol, and capable of prolyl aminopeptidase production in an enzyme-substrate test.[5]
Molecular biology
Though it shares many similarities with the saccharolytic species, Neisseria flavescens has a greater genetic relation to pathogenic Neisseria species,[6] as molecular studies have shown.[7] In addition, studies implicate that this species plays a role in penicillin-resistant strains of Neisseria meningitidis. The increasing selective pressure from penicillin treatment has led to N. meningitidis' uptake of an altered penicillin-binding protein gene, penA, from Neisseria flavescens via transformation.[8] This modified penicillin-binding protein, also known as mecA, inhibits Neisseria meningitidis' transpeptidases from binding to the β-lactam portion of penicillin.
Disease
Typically serving as a commensal, Neisseria flavescens has also played a pathogenic role, ever since its origin. Arising from an epidemic meningitis outbreak in Chicago, N. flavescens was isolated from the cerebrospinal fluid of infected individuals. In particular, out of forty-seven total cases of meningitis, fourteen individuals were found to carry N. flavescens, in contrast to carrying one of the typical four meningococci.[2] Additionally, the mortality rate among these fourteen individuals was close to thirty percent, indicating that this bacterium's role as a possible causative agent for meningitis should not be overlooked.[2] Since then, four other cases of meningitis have also found Neisseria flavescens to be the causative agent.[9]
Along with meningitis, this organism has also been linked to sepsis following surgery.[9] A patient presented with clinical signs typical of meningococcal-strains: fever, chills, headache, myalgia, arthralgia, and skin rash.[9] To identify the causative agent, smears from skin lesions and blood cultures were obtained from the patient.[9] Gram-negative, diplococci were present in the smear, narrowing the organism down to a Neisseria species. Ultimately, blood cultures revealed N. flavescens to be the culprit, due to observation of yellow-gold colony formation and no sugar fermentation.[9]
In addition to blood and CSF, Neisseria flavescens can also act as a pathogen in the lower respiratory tract.[4] Isolation via a transthoracic pulmonary fine-needle aspiration identified N. flavescens as the cause of pneumonia and empyema in a diabetic patient.[4] More specifically, the aspirate was sent off to the respiration department, where it underwent acid fast and gram staining, inoculation, and biochemical testing to identify N. flavescens.[4] Next, 16S rRNA sequencing was done, further confirming that Neisseria flavescens was indeed the causative agent.[4]
Lastly, this bacteria has also been the pathogen behind a case of endocarditis. Testing β-lactamase positive, Neisseria flavescens rendered penicillin an ineffective treatment for the patient and, instead, was targeted by cefotaxime.[10]
See also
References
- ↑ LPSN lpsn.dsmz.de
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Branham, Sara E. (1930-04-18). "A New Meningococcus-like Organism (Neisseria flavescens n. sp.) from Epidemic Meningitis". Public Health Reports 45 (16): 845–849. doi:10.2307/4579618.
- ↑ 3.0 3.1 "What does Neisseria flavescens mean? Definition, meaning and sense (The Titi Tudorancea Encyclopedia)". https://www.tititudorancea.com/z/neisseria_flavescens.htm.
- ↑ 4.0 4.1 4.2 4.3 4.4 Huang, Ling; Ma, Lan; Fan, Kun; Li, Yang; Xie, Le; Xia, Wenying; Gu, Bing; Liu, Genyan (2014-05-01). "Necrotizing pneumonia and empyema caused by Neisseria flavescens infection". Journal of Thoracic Disease 6 (5): 553–557. doi:10.3978/j.issn.2072-1439.2014.02.16. ISSN 2072-1439. PMID 24822118.
- ↑ 5.0 5.1 "Neisseria flavescens - Gonorrhea - STD Information from CDC". https://www.cdc.gov/std/gonorrhea/lab/nflavesc.htm.
- ↑ 6.0 6.1 6.2 Knapp, J. S. (1988). "Historical perspectives and identification of Neisseria and related species". Clinical Microbiology Reviews 1 (4): 415–431. doi:10.1128/CMR.1.4.415. PMID 3069201. PMC 358063. http://cmr.asm.org/content/1/4/415.full.pdf.
- ↑ HOKE, C.; VEDROS, N. A. (1982). "Taxonomy of the Neisseriae: Deoxyribonucleic Acid Base Composition, Interspecific Transformation, and Deoxyribonucleic Acid Hybridization". International Journal of Systematic Bacteriology 32 (1): 57–66. doi:10.1099/00207713-32-1-57.
- ↑ Spratt, B G; Zhang, Q Y; Jones, D M; Hutchison, A; Brannigan, J A; Dowson, C G (1989-11-01). "Recruitment of a penicillin-binding protein gene from Neisseria flavescens during the emergence of penicillin resistance in Neisseria meningitidis.". Proceedings of the National Academy of Sciences of the United States of America 86 (22): 8988–8992. doi:10.1073/pnas.86.22.8988. ISSN 0027-8424. PMID 2510173. Bibcode: 1989PNAS...86.8988S.
- ↑ 9.0 9.1 9.2 9.3 9.4 Wertlake, Paul T.; Williams, Temple W. (1968-07-01). "Septicaemia caused by Neisseria flavescens". Journal of Clinical Pathology 21 (4): 437–439. doi:10.1136/jcp.21.4.437. ISSN 0021-9746. PMID 4972296.
- ↑ Sinave, Christian P.; Ratzan, Kenneth R. (1987). "Infective endocarditis caused by Neisseria flavescens". The American Journal of Medicine 82 (1): 163–164. doi:10.1016/0002-9343(87)90399-8. PMID 3799678. http://www.amjmed.com/article/0002-9343(87)90399-8/pdf. Retrieved 2015-11-28.
External links
Wikidata ☰ Q22286328 entry
 |

