Medicine:Medical ventilator
| Medical ventilator | |
|---|---|
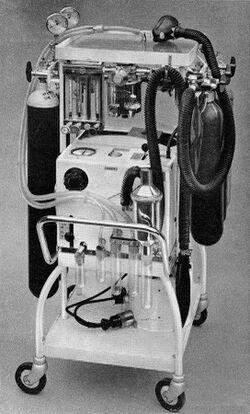
 The Bird VIP Infant ventilator | |
| Specialty | pulmonology |
A medical ventilator (or simply ventilator in context) is a machine designed to provide mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently.
While modern ventilators are computerized machines, patients can be ventilated with a simple, hand-operated bag valve mask.
Ventilators are chiefly used in intensive care medicine, home care, and emergency medicine (as standalone units) and in anesthesiology (as a component of an anesthesia machine).
Medical ventilators are sometimes colloquially called "respirators", a term stemming from commonly used devices in the 1950s (particularly the "Bird Respirator"). However, in modern hospital and medical terminology, these machines are never referred to as respirators, and use of "respirator" in this context is now a deprecated anachronism signaling technical unfamiliarity. In the present-day medical field, the word "respirator" refers to a protective face mask.[1]
Function
In its simplest form, a modern positive pressure ventilator consists of a compressible air reservoir or turbine, air and oxygen supplies, a set of valves and tubes, and a disposable or reusable "patient circuit". The air reservoir is pneumatically compressed several times a minute to deliver room-air, or in most cases, an air/oxygen mixture to the patient. If a turbine is used, the turbine pushes air through the ventilator, with a flow valve adjusting pressure to meet patient-specific parameters. When over pressure is released, the patient will exhale passively due to the lungs' elasticity, the exhaled air being released usually through a one-way valve within the patient circuit called the patient manifold.
Ventilators may also be equipped with monitoring and alarm systems for patient-related parameters (e.g. pressure, volume, and flow) and ventilator function (e.g. air leakage, power failure, mechanical failure), backup batteries, oxygen tanks, and remote control. The pneumatic system is nowadays often replaced by a computer-controlled turbopump.
Modern ventilators are electronically controlled by a small embedded system to allow exact adaptation of pressure and flow characteristics to an individual patient's needs. Fine-tuned ventilator settings also serve to make ventilation more tolerable and comfortable for the patient. In Canada and the United States, respiratory therapists are responsible for tuning these settings, while biomedical technologists are responsible for the maintenance. In the United Kingdom and Europe the management of the patient's interaction with the ventilator is done by critical care nurses.
The patient circuit usually consists of a set of three durable, yet lightweight plastic tubes, separated by function (e.g. inhaled air, patient pressure, exhaled air). Determined by the type of ventilation needed, the patient-end of the circuit may be either noninvasive or invasive.
Noninvasive methods, such as Continuous positive airway pressure (CPAP) and Non-invasive ventilation, which are adequate for patients who require a ventilator only while sleeping and resting, mainly employ a nasal mask. Invasive methods require intubation, which for long-term ventilator dependence will normally be a tracheotomy cannula, as this is much more comfortable and practical for long-term care than is larynx or nasal intubation.
Life-critical system
Because failure may result in death, mechanical ventilation systems are classified as a life-critical system, and precautions must be taken to ensure that they are highly reliable, including their power-supply.
Mechanical ventilators are therefore carefully designed so that no single point of failure can endanger the patient. They may have manual backup mechanisms to enable hand-driven respiration in the absence of power (such as the mechanical ventilator integrated into an anaesthetic machine). They may also have safety valves, which open to atmosphere in the absence of power to act as an anti-suffocation valve for spontaneous breathing of the patient. Some systems are also equipped with compressed-gas tanks, air compressors, and/or backup batteries to provide ventilation in case of power failure or defective gas supplies, and methods to operate or call for help if their mechanisms or software fail.
History
The history of mechanical ventilation begins with various versions of what was eventually called the iron lung, a form of noninvasive negative pressure ventilator widely used during the polio epidemics of the 20th century after the introduction of the "Drinker respirator" in 1928, improvements introduced by John Haven Emerson in 1931,[2] and the Both respirator in 1937. Other forms of noninvasive ventilators, also used widely for polio patients, include Biphasic Cuirass Ventilation, the rocking bed, and rather primitive positive pressure machines.[2]
In 1949, John Haven Emerson developed a mechanical assister for anesthesia with the cooperation of the anesthesia department at Harvard University. Mechanical ventilators began to be used increasingly in anesthesia and intensive care during the 1950s. Their development was stimulated both by the need to treat polio patients and the increasing use of muscle relaxants during anesthesia. Relaxant drugs paralyze the patient and improve operating conditions for the surgeon but also paralyze the respiratory muscles.
In the United Kingdom, the East Radcliffe and Beaver models were early examples, the latter using an automotive wiper motor to drive the bellows used to inflate the lungs.[3] Electric motors were, however, a problem in the operating theatres of that time, as their use caused an explosion hazard in the presence of flammable anesthetics such as ether and cyclopropane. In 1952, Roger Manley of the Westminster Hospital, London, developed a ventilator which was entirely gas driven, and became the most popular model used in Europe. It was an elegant design, and became a great favourite with European anesthetists for four decades, prior to the introduction of models controlled by electronics. It was independent of electrical power, and caused no explosion hazard. The original Mark I unit was developed to become the Manley Mark II in collaboration with the Blease company, who manufactured many thousands of these units. Its principle of operation was very simple, an incoming gas flow was used to lift a weighted bellows unit, which fell intermittently under gravity, forcing breathing gases into the patient's lungs. The inflation pressure could be varied by sliding the movable weight on top of the bellows. The volume of gas delivered was adjustable using a curved slider, which restricted bellows excursion. Residual pressure after the completion of expiration was also configurable, using a small weighted arm visible to the lower right of the front panel. This was a robust unit and its availability encouraged the introduction of positive pressure ventilation techniques into mainstream European anesthetic practice.
The 1955 release of Forrest Bird's "Bird Universal Medical Respirator" in the United States changed the way mechanical ventilation was performed, with the small green box becoming a familiar piece of medical equipment.[4] The unit was sold as the Bird Mark 7 Respirator and informally called the "Bird". It was a pneumatic device and therefore required no electrical power source to operate.
In 1965, the Army Emergency Respirator was developed in collaboration with the Harry Diamond Laboratories (now part of the U.S. Army Research Laboratory) and Walter Reed Army Institute of Research. Its design incorporated the principle of fluid amplification in order to govern pneumatic functions. Fluid amplification allowed the respirator to be manufactured entirely without moving parts yet capable of complex resuscitative functions. [5] Elimination of moving parts increased performance reliability and minimized maintenance. [6] The mask is composed of a poly(methyl methacrylate) (also known as lucite) block, about the size of a pack of cards, with machined channels and a cemented and/or screwed-in cover plate. [7] The reduction of moving parts cut manufacturing costs and increased durability. [6]
The bistable fluid amplifier design allowed the respirator to function as both a respiratory assistor and controller. It could functionally transition between assistor and controller automatically based on the patient’s needs. [7] [6] The dynamic pressure and turbulent jet flow of gas from inhalation to exhalation allowed the respirator to synchronize with the breathing of the patient. [8]
Intensive care environments around the world revolutionized in 1971 by the introduction of the first SERVO 900 ventilator (Elema-Schönander). It was a small, silent and effective electronic ventilator, with the famous SERVO feedback system controlling what had been set and regulating delivery. For the first time, the machine could deliver the set volume in volume control ventilation.
Ventilators used under increased pressure (hyperbaric) require special precautions and few ventilators can operate under these conditions.[9] In 1979, Sechrist Industries introduced their Model 500A ventilator which was specifically designed for use with hyperbaric chambers.[10]
In 1991 the SERVO 300 ventilator series was introduced. The platform of the SERVO 300 series enabled treatment of all patient categories, from adult to neonate, with one single ventilator. The SERVO 300 series provided a completely new and unique gas delivery system, with rapid flow-triggering response.
In 1999 the LTV (Laptop Ventilator) Series was introduced into the market. The new ventilator was significantly smaller than the ventilators of that time weighing ~14 lbs and around the size of a laptop computer. This new design kept the same functionality of the in hospital ventilators, while now opening up a world of opportunity of mobility for the patients.
A modular concept, meaning that the hospital has one ventilator model throughout the ICU department instead of a fleet with different models and brands for the different user needs, was introduced with SERVO-i in 2001. With this modular concept the ICU departments could choose the modes and options, software and hardware needed for a particular patient category.
In the twenty-first century small portable ventilators, for example the SAVe II, have been manufactured for forward combat use. [11]
See also
- Artificial ventilation
- Mechanical ventilation
- Respiratory therapy
- Robert Martensen
References
- ↑ Health, Center for Devices and Radiological (2019-02-08). "Personal Protective Equipment for Infection Control - Masks and N95 Respirators" (in en). FDA. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/GeneralHospitalDevicesandSupplies/PersonalProtectiveEquipment/ucm055977.htm. Retrieved 2017-03-08.
- ↑ 2.0 2.1 Geddes LA (2007). "The history of artificial respiration". IEEE Engineering in Medicine and Biology Magazine 26 (6): 38–41. doi:10.1109/EMB.2007.907081. PMID 18189086.
- ↑ "Radcliffe respiration pumps". The Lancet 270 (6922): 539–41. April 1956. doi:10.1016/s0140-6736(56)90597-9. PMID 13320798.
- ↑ Bellis, Mary. "Forrest Bird invented a fluid control device, respirator & pediatric ventilator". About.com. http://inventors.about.com/od/bstartinventors/a/Forrest_Bird.htm. Retrieved 2009-06-04.
- ↑ (in en) Army R, D & A.. Development and Engineering Directorate, HQ, U.S. Army Materiel Development and Readiness Command. 1965. https://books.google.com/?id=sTrO77DCgkwC&pg=RA6-PA33&lpg=RA6-PA33&dq=Army+Emergency+Respirator,+HDL#v=onepage&q=Army%20Emergency%20Respirator,%20HDL&f=false.
- ↑ 6.0 6.1 6.2 Mon, George; Woodward, Kenneth E.; Straub, Henrik; Joyce, James; Meyer, James (1966). "Fluid Amplifier-Controlled Medical Devices". SAE Transactions 74: 217–222. ISSN 0096-736X.
- ↑ 7.0 7.1 "Army Research and Development Monthly Magazine, Vol. 6, No. 9". https://asc.army.mil/docs/pubs/alt/archives/1965/Sep_1965.PDF.
- ↑ "Fluid Amplification Symposium, October 1965, Vol. III". https://apps.dtic.mil/dtic/tr/fulltext/u2/623457.pdf.
- ↑ Skinner, M (1998). "Ventilator function under hyperbaric conditions". South Pacific Underwater Medicine Society Journal 28 (2). http://archive.rubicon-foundation.org/5927. Retrieved 2009-06-04.
- ↑ "Performance of the Seachrist 500A Hyperbaric Ventilator in a Monoplace Hyperbaric Chamber". Journal of Hyperbaric Medicine 3 (4): 215–225. 1988. http://archive.rubicon-foundation.org/4377. Retrieved 2009-06-04.
- ↑ "SAVe II The Smallest and Easiest to Use Pre-hospital Ventilator". Automedx. http://automedx.com/save-ii/.
