Medicine:Myelolipoma
Myelolipoma (myelo-, from the Ancient Greek μυελός 'marrow'; lipo, 'of, or pertaining to, fat'; -oma 'tumor or mass'; also myolipoma) is a benign tumor-like lesion composed of mature adipose (fat) tissue and haematopoietic (blood-forming) elements in various proportions.[1]
Myelolipomas can present in the adrenal gland,[2] or outside of the gland.[3]
Signs and symptoms
The majority of myelolipomas are asymptomatic. Most do not produce any adrenal hormones. Most are only discovered as a result of investigation for another problem.[4]
When myelolipomas do produce symptoms, it is usually because they have become large, and are pressing on other organs or tissues nearby. Symptoms include pain in the abdomen or flank, blood in the urine, a palpable lump or high blood pressure.[1]
As they are benign tumors, myelolipomas do not spread to other body parts. Larger myelolipomas are at risk of localised tissue death and bleeding, which may cause a retroperitoneal haemorrhage.[1]
Causes
Although several hypotheses have been proposed as to the cause of myelolipoma, the causative process is still not clearly understood.[5] Recent experimental evidence suggests that both the myeloid and lipomatous elements have a monoclonal origin, which strongly supports the hypothesis that myelolipomas are neoplastic lesions.[5]
Older theories proposing a non-neoplastic origin include the following:
- Adrenal cortical cells, or other cells within the stroma of the adrenal cortex that are able to differentiate, may reversibly change into fat or blood-forming cells. This might occur because of the actions of adrenal cortex hormones, or of hormones released by the pituitary gland that act on the adrenal glands, such as adrenocorticotropic hormone (ACTH).[6]
- The blood-forming cells may arise by differentiation of cells within the capillaries of the adrenal gland.[4]
- Myelolipoma simply represents a site of normal blood formation outside the bone marrow.[4]
Pathology
Macroscopic features
Myelolipomas are usually found to occur alone in one adrenal gland, but not both. They can vary widely in size, from as small as a few millimetres to as large as 34 centimeters in diameter. The cut surface has colours varying from yellow to red to mahogany brown, depending on the distribution of fat, blood, and blood-forming cells. The cut surface of larger myelolipomas may contain haemorrhage or infarction.[1]
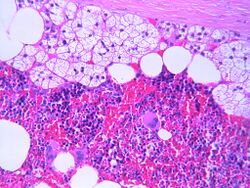
Microscopic features
The typical microscopic features of myelolipomas are shown in the image. There is a mixture of normal adrenal tissue, fat, and a full trilineage maturation of the three major blood-forming elements: myeloid (white blood cell forming), erythroid (red blood cell forming), and megakaryocytic (platelet forming) lines.[1]
Diagnosis
Most myelolipomas are unexpected findings on CT scans and MRI scans of the abdomen. They may sometimes be seen on a plain X-ray films.[4]
Fine needle aspiration may be performed to obtain cells for microscopic diagnosis.[1]
Treatment
Small myelolipomas generally do not produce symptoms, and do not require treatment. Ongoing surveillance of these lesions by a doctor is recommended. Surgical excision (removal) is recommended for large myelolipomas because of the risk of bleeding complications.[6]
Epidemiology

Myelolipomas are rare. They have been reported to be found unexpectedly at autopsy in 0.08% to 0.4% of cases (i.e.: somewhere between 8 per 10,000 and 4 per 1,000 autopsies). They most commonly occur in the adrenal gland, and comprise about 8% of all adrenal tumours.[8] They may also occur in other sites, such as the mediastinum, the liver and the gastrointestinal tract.[1]
There is no gender predilection, males and females are affected equally. The peak age range at diagnosis is between 40 and 79 years of age.[1]
References
- ↑ Jump up to: 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Thompson, LDR (2006). Endocrine Pathology. Foundations in Diagnostic Pathology. ISBN 978-0-443-06685-6.
- ↑ "Myelolipoma within a non-functional adrenal cortical adenoma". Singapore Med J 48 (7): e200–2. July 2007. PMID 17609815. http://smj.sma.org.sg/4807/4807cr6.pdf.
- ↑ "Simultaneous adrenal and extra-adrenal myelolipoma — an uncommon incident: case report and review of the literature". World J Surg Oncol 6: 72. 2008. doi:10.1186/1477-7819-6-72. PMID 18601731.
- ↑ Jump up to: 4.0 4.1 4.2 4.3 Ramchandani, P. Adrenal Myelolipoma Imaging at eMedicine
- ↑ Jump up to: 5.0 5.1 McNicol AM (Winter 2008). "A diagnostic approach to adrenal cortical lesions". Endocr Pathol 19 (4): 241–251. doi:10.1007/s12022-008-9055-x. PMID 19089656.
- ↑ Jump up to: 6.0 6.1 "Myelolipoma". J Urol 176 (3): 1188. September 2006. doi:10.1016/j.juro.2006.06.095. PMID 16890722.
- ↑ Data and references for pie chart are located at file description page in Wikimedia Commons.
- ↑ Mantero, Franco; Albiger, Nora (2004). "A comprehensive approach to adrenal incidentalomas". Arquivos Brasileiros de Endocrinologia & Metabologia 48 (5): 583–591. doi:10.1590/S0004-27302004000500003. ISSN 0004-2730.
External links
 |