Medicine:Scoliosis
| Scoliosis | |
|---|---|
 | |
| Pronunciation | |
| Specialty | Orthopedic surgery |
| Symptoms | Sideways curve in the back[2] |
| Usual onset | 10–20 years old[2] |
| Causes | Usually unknown[3] |
| Risk factors | Family history, cerebral palsy, Marfan syndrome, tumors such as neurofibromatosis[2] |
| Diagnostic method | X-ray[2] |
| Treatment | Watchful waiting, bracing, exercises, surgery[2][4] |
| Frequency | 3%[5][6] |
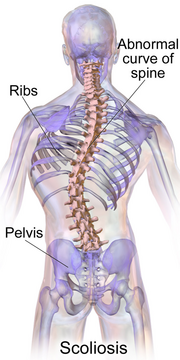
Scoliosis (pl.: scolioses) is a condition in which a person's spine has an abnormal curve.[2] The curve is usually S- or C-shaped over three dimensions.[2][7] In some, the degree of curve is stable, while in others, it increases over time.[3] Mild scoliosis does not typically cause problems, but more severe cases can affect breathing and movement.[3][8] Pain is usually present in adults, and can worsen with age.[9] As the condition progresses, it may impact a person's life and hence, can also be considered a disability.[10]
The cause of most cases is unknown, but it is believed to involve a combination of genetic and environmental factors.[3] Risk factors include other affected family members.[2] It can also occur due to another condition such as muscle spasms, cerebral palsy, Marfan syndrome, and tumors such as neurofibromatosis.[2] Diagnosis is confirmed with X-rays.[2] Scoliosis is typically classified as either structural in which the curve is fixed, or functional in which the underlying spine is normal.[2] Left-right asymmetries, of the vertebrae and their musculature, especially in the thoracic region,[11] may cause mechanical instability of the spinal column.
Treatment depends on the degree of curve, location, and cause.[2] The age of the patient is also important, since some treatments are ineffective in adults, who are no longer growing. Minor curves may simply be watched periodically.[2] Treatments may include bracing, specific exercises, posture checking, and surgery.[2][4] The brace must be fitted to the person and used daily until growing stops.[2] Specific exercises, such as exercises that focus on the core, may be used to try to decrease the risk of worsening.[4] They may be done alone or along with other treatments such as bracing.[12][13] Evidence that chiropractic manipulation, dietary supplements, or exercises can prevent the condition from worsening is weak.[2][14] However, exercise is still recommended due to its other health benefits.[2]
Scoliosis occurs in about 3% of people.[5] It most commonly develops between the ages of ten and twenty.[2] Females typically are more severely affected than males with a ratio of 4:1.[2][3] The term is from grc σκολίωσις (skolíōsis), which means "a bending".[15]
Signs and symptoms
Symptoms associated with scoliosis can include:
- Pain in the back at the site of the curve, which may radiate to the legs[16]
- Respiratory or cardiac problems in severe cases[17]
- Constipation due to curvature causing "tightening" of the stomach, intestines, etc.[18]
The signs of scoliosis can include:
- Uneven musculature on one side of the spine[19]
- Rib prominence or a prominent shoulder blade, caused by rotation of the rib cage in thoracic scoliosis[20]
- Uneven posture[20]
- Heart and lung problems in severe cases[17]
- Calcium deposits in the cartilage endplate and sometimes in the disc itself[21]
Course
People who have reached skeletal maturity are less likely to have a worsening case.[22] Some severe cases of scoliosis can lead to diminishing lung capacity, pressure exerted on the heart, and restricted physical activities.[23]
Longitudinal studies have revealed that the most common form of the condition, late-onset idiopathic scoliosis, causes little physical impairment other than back pain and cosmetic concerns, even when untreated, with mortality rates similar to the general population.[24][25] Older beliefs that untreated idiopathic scoliosis necessarily progressed into severe (cardiopulmonary) disability by old age have been refuted.[26]
Causes
An estimated 65% of scoliosis cases are idiopathic (cause unknown), about 15% are congenital, and about 10% are secondary to a neuromuscular disease.[27]
About 38% of variance in scoliosis risk is due to genetic factors, and 62% is due to the environment.[28] The genetics are likely complex, however, given the inconsistent inheritance and discordance among monozygotic twins.[28] The specific genes that contribute to development of scoliosis have not been conclusively identified. At least one gene, CHD7, has been associated with the idiopathic form of scoliosis.[29] Several candidate gene studies have found associations between idiopathic scoliosis and genes mediating bone formation, bone metabolism, and connective tissue structure.[28] Several genome-wide studies have identified a number of loci as significantly linked to idiopathic scoliosis.[28] In 2006, idiopathic scoliosis was linked with three microsatellite polymorphisms in the MATN1 gene (encoding for matrilin 1, cartilage matrix protein).[30] Fifty-three single nucleotide polymorphism markers in the DNA that are significantly associated with adolescent idiopathic scoliosis were identified through a genome-wide association study.[31]
Adolescent idiopathic scoliosis has no clear causal agent, and is generally believed to be multifactorial; leading to "progressive functional limitations" for individuals.[32][33][34][29][35] Research suggests that Posterior Spinal Fusion (PSF) can be used to correct the more severe deformities caused by adolescent idiopathic scoliosis.[36][37][38][39][40] Such procedures can result in a return to physical activity in about 6 months, which is very promising, although minimal back pain is still to be expected in the most severe cases.[41][42][43][44][40] The prevalence of scoliosis is 1–2% among adolescents, but the likelihood of progression among adolescents with a Cobb angle less than 20° is about 10–20%.[45]
Congenital scoliosis can be attributed to a malformation of the spine during weeks three to six in utero due to a failure of formation, a failure of segmentation, or a combination of stimuli.[46] Incomplete and abnormal segmentation results in an abnormally shaped vertebra, at times fused to a normal vertebra or unilaterally fused vertebrae, leading to the abnormal lateral curvature of the spine.[47]
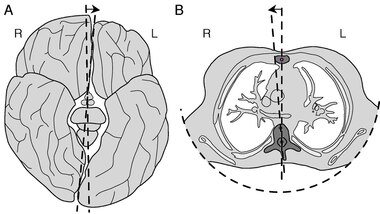
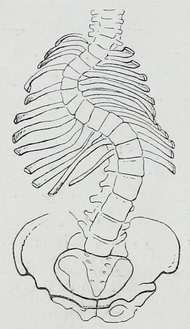
Vertebrae of the spine, especially in the thoracic region, are, on average, asymmetric.[11] The mid-axis of these vertebral bodies tends to point systematically to the right of the median body plane. A strong asymmetry of the vertebrae and their musculature, may lead to mechanical instability of the column, especially during phases of rapid growth. The asymmetry is thought to be caused by an embryological twist of the body.[49]
Resulting from other conditions
Secondary scoliosis due to neuropathic and myopathic conditions can lead to a loss of muscular support for the spinal column so that the spinal column is pulled in abnormal directions.[citation needed] Some conditions which may cause secondary scoliosis include muscular dystrophy, spinal muscular atrophy, poliomyelitis, cerebral palsy, spinal cord trauma, and myotonia.[50][51] Scoliosis often presents itself, or worsens, during an adolescent's growth spurt and is more often diagnosed in females than males.[45]
Scoliosis associated with known syndromes is often subclassified as "syndromic scoliosis".[52] Scoliosis can be associated with amniotic band syndrome,[53] Arnold–Chiari malformation,[54] Charcot–Marie–Tooth disease,[55] cerebral palsy,[56] congenital diaphragmatic hernia,[57] connective tissue disorders,[58] muscular dystrophy,[59] familial dysautonomia,[60] CHARGE syndrome,[61] Ehlers–Danlos syndrome[58] (hyperflexibility, "floppy baby" syndrome, and other variants of the condition), fragile X syndrome,[62][63] Friedreich's ataxia,[64] hemihypertrophy,[65] Loeys–Dietz syndrome,[66] Marfan syndrome,[58] nail–patella syndrome,[67] neurofibromatosis,[68] osteogenesis imperfecta,[69] Prader–Willi syndrome,[70] proteus syndrome,[71] spina bifida,[72] spinal muscular atrophy,[73] syringomyelia,[74] and pectus carinatum.[75]
Another form of secondary scoliosis is degenerative scoliosis, also known as de novo scoliosis, which develops later in life secondary to degenerative (may or may not be associated with aging) changes. This is a type of deformity that starts and progresses because of the collapse of the vertebral column in an asymmetrical manner. As bones start to become weaker and the ligaments and discs located in the spine become worn as a result of age-related changes, the spine begins to curve.[76]
Diagnosis
People who initially present with scoliosis undergo a physical examination to determine whether the deformity has an underlying cause and to exclude the possibility of the underlying condition more serious than simple scoliosis.[citation needed]Lua error: not enough memory.
The person's gait is assessed, with an exam for signs of other abnormalities (e.g., spina bifida as evidenced by a dimple, hairy patch, lipoma, or hemangioma). A thorough neurological examination is also performed, the skin for café au lait spots, indicative of neurofibromatosis, the feet for cavovarus deformity, abdominal reflexes and muscle tone for spasticity.Lua error: not enough memory.
When a person can cooperate, he or she is asked to bend forward as far as possible. This is known as the Adams forward bend test[77] and is often performed on school students. If a prominence is noted, then scoliosis is a possibility and an X-ray may be done to confirm the diagnosis.
As an alternative, a scoliometer may be used to diagnose the condition.[78]
When scoliosis is suspected, weight-bearing, full-spine AP/coronal (front-back view) and lateral/sagittal (side view) X-rays are usually taken to assess the scoliosis curves and the kyphosis and lordosis, as these can also be affected in individuals with scoliosis. Full-length standing spine X-rays are the standard method for evaluating the severity and progression of scoliosis, and whether it is congenital or idiopathic in nature. In growing individuals, serial radiographs are obtained at 3- to 12-month intervals to follow curve progression, and, in some instances, MRI investigation is warranted to look at the spinal cord.[79] An average scoliosis patient has been in contact with around 50–300 mGy of radiation due to these radiographs during this time period.[80]
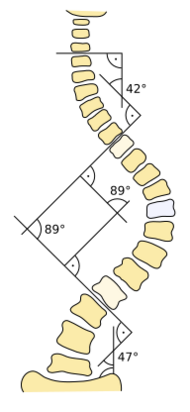
The standard method for assessing the curvature quantitatively is measuring the Cobb angle, which is the angle between two lines, drawn perpendicular to the upper endplate of the uppermost vertebra involved and the lower endplate of the lowest vertebra involved. For people with two curves, Cobb angles are followed for both curves. In some people, lateral-bending X-rays are obtained to assess the flexibility of the curves or the primary and compensatory curves.Lua error: Internal error: The interpreter exited with status 1.
Congenital and idiopathic scoliosis that develops before the age of 10 is referred to as early-onset scoliosis.[81] Progressive idiopathic early-onset scoliosis can be a life-threatening condition with negative effects on pulmonary function.[82][83] Scoliosis that develops after 10 is referred to as adolescent idiopathic scoliosis.[3] Screening adolescents without symptoms for scoliosis is of unclear benefit.[84]
Definition
Scoliosis is defined as a three-dimensional deviation in the axis of a person's spine.[45][7] Most instances, including the Scoliosis Research Society, define scoliosis as a Cobb angle of more than 10° to the right or left as the examiner faces the person, i.e. in the coronal plane.[85]
Scoliosis has been described as a biomechanical deformity, the progression of which depends on asymmetric forces otherwise known as the Hueter–Volkmann Law.[31]
Management
Scoliosis curves do not straighten out on their own. Many children have slight curves that do not need treatment. In these cases, the children grow up to lead normal body posture by itself, even though their small curves never go away. If the patient is still growing and has a larger curve, it is important to monitor the curve for change by periodic examination and standing x-rays as needed. The rise in spinal abnormalities require examination by an Neurosurgeon to determine if active treatment is needed.[86]
The traditional medical management of scoliosis is complex and is determined by the severity of the curvature and skeletal maturity, which together help predict the likelihood of progression. The conventional options for children and adolescents are:[87]
- Observation
- Bracing
- Surgery
- Physical therapy. Evidence suggests use of scoliosis specific exercises might prevent the progression of the curve along with possible bracing and surgery avoidance.[88]
For adults, treatment usually focuses on relieving any pain:[89][90]
- Pain medication
- Posture checking
- Bracing
- Surgery[91]
Treatment for idiopathic scoliosis also depends upon the severity of the curvature, the spine's potential for further growth, and the risk that the curvature will progress. Mild scoliosis (less than 30° deviation) and moderate scoliosis (30–45°) can typically be treated conservatively with bracing in conjunction with scoliosis-specific exercises.[4] Severe curvatures that rapidly progress may require surgery with spinal rod placement and spinal fusion. In all cases, early intervention offers the best results.Lua error: Internal error: The interpreter exited with status 1.
A specific type of physical therapy may be useful.[92][4] Evidence to support its use, however, is weak.[2][14] Low quality evidence suggests scoliosis-specific exercises (SSE) may be more effective than electrostimulation.[93] Evidence for the Schroth method is insufficient to support its use.[94] Significant improvement in function, vertebral angles and trunk asymmetries have been recorded following the implementation of Schroth method in terms of conservative management of scoliosis. Some other forms of exercises interventions have been latelyLua error: Internal error: The interpreter exited with status 1. used in the clinical practice for therapeutic management of scoliosis such as global postural reeducation and the Klapp method.[88]
Bracing

Bracing is normally done when the person has bone growth remaining and is, in general, implemented to hold the curve and prevent it from progressing to the point where surgery is recommended. In some cases with juveniles, bracing has reduced curves significantly, going from a 40° (of the curve, mentioned in length above) out of the brace to 18°. Braces are sometimes prescribed for adults to relieve pain related to scoliosis. Bracing involves fitting the person with a device that covers the torso; in some cases, it extends to the neck (example being the Milwaukee Brace).[95]

The most commonly used brace is a TLSO, such as a Boston brace, a corset-like an appliance that fits from armpits to hips and is custom-made from fiberglass or plastic. It is typically recommended to be worn 22–23 hours a day, and applies pressure on the curves in the spine. The effectiveness of the brace depends on not only brace design and orthotist skill, but also people's compliance and amount of wear per day. An alternative form of brace is a nighttime only brace, that is worn only at night whilst the child sleeps, and which overcorrects the deformity.[96] Whilst nighttime braces are more convenient for children and families, it is unknown if the effectiveness of the brace is as good as conventional braces. The UK government have funded a large clinical trial (called the BASIS study) to resolve this uncertainty.[97] The BASIS study is ongoing throughout the UK in all of the leading UK children's hospitals that treat scoliosis, with families encouraged to take part.
Indications for bracing: people who are still growing who present with Cobb angles less than 20° should be closely monitored. People who are still growing who present with Cobb angles of 20 to 29° should be braced according to the risk of progression by considering age, Cobb angle increase over a six-month period, Risser sign, and clinical presentation. People who are still growing who present with Cobb angles greater than 30° should be braced. However, these are guidelines and not every person will fit into this table.
For example, a person who is still growing with a 17° Cobb angle and significant thoracic rotation or flatback could be considered for nighttime bracing. On the opposite end of the growth spectrum, a 29° Cobb angle and a Risser sign three or four might not need to be braced because the potential for progression is reduced.[98] The Scoliosis Research Society's recommendations for bracing include curves progressing to larger than 25°, curves presenting between 30 and 45°, Risser sign 0, 1, or 2 (an X-ray measurement of a pelvic growth area), and less than six months from the onset of menses in girls.[99]
Evidence supports that bracing prevents worsening of disease, but whether it changes quality of life, appearance, or back pain is unclear.[100]
Surgery
Lua error: Internal error: The interpreter exited with status 1. Surgery is usually recommended by orthopedists for curves with a high likelihood of progression (i.e., greater than 45–50° of magnitude), curves that would be cosmetically unacceptable as an adult, curves in people with spina bifida and cerebral palsy that interfere with sitting and care, and curves that affect physiological functions such as breathing.[101][102]
Surgery is indicated by the Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) at 45–50°[4] and by the Scoliosis Research Society (SRS) at a Cobb angle of 45°.[103] SOSORT uses the 45–50° threshold as a result of the well-documented, plus or minus 5° measurement error that can occur while measuring Cobb angles.[103]
Surgeons who are specialized in spine surgery perform surgery for scoliosis. To completely straighten a scoliotic spine is usually impossible, but for the most part, significant corrections are achieved.[104]
The two main types of surgery are:[105]
- Anterior fusion: This surgical approach is through an incision at the side of the chest wall.
- Posterior fusion: This surgical approach is through an incision on the back and involves the use of metal instrumentation to correct the curve.
One or both of these surgical procedures may be needed. The surgery may be done in one or two stages and, on average, takes four to eight hours.
A new tethering procedure (anterior vertebral body tethering) may be appropriate for some patients.[106]
Spine surgery can be painful and may also be associated with post-surgical pain.[102] Different approaches for pain management are used in surgery including epidural administration and systemic analgesia (also known as general analgesia).[102] Epidural analgesia medication are often used surgically including combinations of local anesthetics and pain medications injected via an epidural injection.[102] Evidence comparing different approaches for analgesia, side effects or benefits, and which approach results in greater pain relief and for how long after this type of surgery is of low to moderate quality.[102]
Prognosis
A 50-year follow-up study published in the Journal of the American Medical Association (2003) asserted the lifelong physical health, including cardiopulmonary and neurological functions, and mental health of people with idiopathic scoliosis are comparable to those of the general population. Scoliosis that interferes with normal systemic functions is "exceptional"[107] and "rare", and "untreated [scoliosis] people had similar death rates and were just as functional and likely to lead productive lives 50 years after diagnosis as people with normal spines."[24][108] In an earlier University of Iowa follow-up study, 91% of people with idiopathic scoliosis displayed normal pulmonary function, and their life expectancy was found to be 2% more than that of the general population.[25] Later (2006–) studies corroborate these findings, adding that they are "reassuring for the adult patient who has adolescent onset idiopathic scoliosis in approximately the 50–70° range."[109] These modern landmark studies supersede earlier studies (e.g. Mankin-Graham-Schauk 1964) that did implicate moderate idiopathic scoliosis in impaired pulmonary function.Lua error: Internal error: The interpreter exited with status 1.
Generally, the prognosis of scoliosis depends on the likelihood of progression. The general rules of progression are larger curves carry a higher risk of progression than smaller curves, and thoracic and double primary curves carry a higher risk of progression than single lumbar or thoracolumbar curves. In addition, people not having yet reached skeletal maturity have a higher likelihood of progression (i.e., if the person has not yet completed the adolescent growth spurt).[110]
Epidemiology
Scoliosis affects 2–3% of the United States population, or about five to nine million cases.[4] A scoliosis (spinal column curve) of 10° or less affects 1.5–3% of individuals.[99] The age of onset is usually between 10 years and 15 years (but can occur younger) in children and adolescents, making up to 85% of those diagnosed. This is due to rapid growth spurts during puberty when spinal development is most susceptible to genetic and environmental influences.[111] Because female adolescents undergo growth spurts before postural musculoskeletal maturity, scoliosis is more prevalent among females.[112]
Although fewer cases are present since using Cobb angle analysis for diagnosis, scoliosis remains significant, appearing in otherwise healthy children. Despite the fact that scoliosis is a disfigurement of the spine, it has been shown to influence the pneumonic function, balance while standing and stride execution in children. The impact of carrying backpacks on these three side effects have been broadly researched.[113] Incidence of idiopathic scoliosis (IS) stops after puberty when skeletal maturity is attained, however further curvature may occur during late adulthood due to vertebral osteoporosis and weakened musculature.[4]
History


Ever since the condition was discovered by the Greek physician Hippocrates, a cure has been sought. Treatments such as bracing and the insertion of rods into the spine were employed during the 1900s. In the mid-20th century, new treatments and improved screening methods have been developed to reduce the progression of scoliosis in patients and alleviate their associated pain. School children were during this period believed to develop poor posture as a result of working at their desks, and many were diagnosed with scoliosis. It was also considered to be caused by tuberculosis or poliomyelitis, diseases that were successfully managed using vaccines and antibiotics.Lua error: Internal error: The interpreter exited with status 1.
The American orthopaedic surgeon Alfred Shands Jr. discovered that two percent of patients had non-disease related scoliosis, later termed idiopathic scoliosis, or the "cancer of orthopaedic surgery". These patients were treated with questionable remedies.[115] A theory at the time—now discredited—was that the condition needed to be detected early to halt its progression, and so some schools made screening for scoliosis mandatory. Measurements of shoulder height, leg length and spinal curvature were made, and the ability to bend forwards, along with body posture, was tested, but students were sometimes misdiagnosed because of their poor posture.Lua error: Internal error: The interpreter exited with status 1.
An early treatment was the Milwaukee brace, a rigid contraption of metal rods attached to a plastic or leather girdle, designed to straighten the spine. Because of the constant pressure applied to the spine, the brace was uncomfortable. It caused jaw and muscle pain, skin irritation, as well as low self-esteem.Lua error: Internal error: The interpreter exited with status 1.
Surgery
In 1962, the American orthopaedic surgeon Paul Harrington introduced a metal spinal system of instrumentation that assisted with straightening the spine, as well as holding it rigid while fusion took place. The now obsolete Harrington rod operated on a ratchet system, attached by hooks to the spine at the top and bottom of the curvature that when cranked would distract—or straighten—the curve. The Harrington rod obviates the need for prolonged casting, allowing patients greater mobility in the postoperative period and significantly reducing the quality of life burden of fusion surgery. The Harrington rod was the precursor to most modern spinal instrumentation systems. A major shortcoming was that it failed to produce a posture wherein the skull would be in proper alignment with the pelvis, and it did not address rotational deformity. As the person aged, there would be increased wear and tear, early onset arthritis, disc degeneration, muscular stiffness, and acute pain. "Flatback" became the medical name for a related complication, especially for those who had lumbar scoliosis.[116]
In the 1960s, the gold standard for idiopathic scoliosis was a posterior approach using a single Harrington rod. Post-operative recovery involved bed rest, casts, and braces. Poor results became apparent over time.[117]
In the 1970s, an improved technique was developed using two rods and wires attached at each level of the spine. This segmented instrumentation system allowed patients to become mobile soon after surgery.[117]
In the 1980s, Cotrel–Dubousset instrumentation improved fixation and addressed sagittal imbalance and rotational defects unresolved by the Harrington rod system. This technique used multiple hooks with rods to give stronger fixation in three dimensions, usually eliminating the need for postoperative bracing.[117]
Evolution

There are links between human spinal morphology, bipedality, and scoliosis which suggest an evolutionary basis for the condition. Scoliosis has not been found in chimpanzees or gorillas.[118] Thus, it has been hypothesized that scoliosis may actually be related to humans' morphological differences from these apes.[118] Other apes have a shorter and less mobile lower spine than humans. Some of the lumbar vertebrae in Pan are "captured", meaning that they are held fast between the ilium bones of the pelvis. Compared to humans, Old World monkeys have far larger erector spinae muscles, which are the muscles which hold the spine steady.[118] These factors make the lumbar spine of most primates less flexible and far less likely to deviate than those of humans. While this may explicitly relate only to lumbar scolioses, small imbalances in the lumbar spine could precipitate thoracic problems as well.[118]
Scoliosis may be a byproduct of strong selection for bipedalism. For a bipedal stance, a highly mobile, elongated lower spine is very beneficial.[118] For instance, the human spine takes on an S-shaped curve with lumbar lordosis, which allows for better balance and support of an upright trunk.[119] Selection for bipedality was likely strong enough to justify the maintenance of such a disorder. Bipedality is hypothesized to have emerged for a variety of different reasons, many of which would have certainly conferred fitness advantages. It may increase viewing distance, which can be beneficial in hunting and foraging as well as protection from predators or other humans; it makes long-distance travel more efficient for foraging or hunting; and it facilitates terrestrial feeding from grasses, trees, and bushes.[120] Given the many benefits of bipedality which depends on a particularly formed spine, it is likely that selection for bipedalism played a large role in the development of the spine as we see it today, in spite of the potential for "scoliotic deviations".[118] According to the fossil record, scoliosis may have been more prevalent among earlier hominids such as Australopithecus and Homo erectus, when bipedality was first emerging. Their fossils indicate that there may have been selected over time for a slight reduction in lumbar length to what we see today, favouring a spine that could efficiently support bipedality with a lower risk of scoliosis.[118]
Society and culture
The cost of scoliosis involves both monetary loss and lifestyle limitations that increase with severity. Respiratory deficiencies may arise from thoracic deformities and cause abnormal breathing.[121] This directly affects capacity for exercise and work, decreasing the overall quality of life.[4]
In the United States, the average hospital cost for cases involving surgical procedures was $30,000 to $60,000 per person in 2010.[122] As of 2006, the cost of bracing was up to $5,000 during rapid growth periods, when braces must be consistently replaced across multiple follow-ups.[4]
The month of June is recognized as Scoliosis Awareness Month to highlight and spread awareness of scoliosis. It emphasizes its wide impact and the need for early detection.[123]
Research
Genetic testing for adolescent idiopathic scoliosis, which became available in 2009 and is still under investigation, attempts to gauge the likelihood of curve progression.[124]Lua error: Internal error: The interpreter exited with status 1.
See also
- Back brace
- Kyphosis
- Lordosis
- Neuromechanics of idiopathic scoliosis
- Pott disease
- Scheuermann's disease
- Schooliosis
- Scoliosis Research Society
References
- ↑ "Scoliosis". http://www.merriam-webster.com/dictionary/scoliosis.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 "Questions and Answers about Scoliosis in Children and Adolescents". December 2015. http://www.niams.nih.gov/health_info/scoliosis/.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 "Adolescent idiopathic scoliosis". September 2013. https://ghr.nlm.nih.gov/condition/adolescent-idiopathic-scoliosis#expand-collapse-start.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 "2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth". Scoliosis and Spinal Disorders 13: 3. 2018. doi:10.1186/s13013-017-0145-8. PMID 29435499.
- ↑ 5.0 5.1 "Scoliosis: review of types of curves, etiological theories and conservative treatment". Journal of Back and Musculoskeletal Rehabilitation 27 (2): 111–115. 2014. doi:10.3233/bmr-130438. PMID 24284269.
- ↑ "Scoliosis - Symptoms, Diagnosis and Treatment". https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Scoliosis.
- ↑ 7.0 7.1 "The third dimension of scoliosis: The forgotten axial plane". Orthopaedics & Traumatology, Surgery & Research 105 (2): 351–359. April 2019. doi:10.1016/j.otsr.2018.10.021. PMID 30665877.
- ↑ "Early-Onset Scoliosis: A Review of History, Current Treatment, and Future Directions". Pediatrics 137 (1): e20150709. January 2016. doi:10.1542/peds.2015-0709. PMID 26644484.
- ↑ "Natural History of Adolescent Idiopathic Scoliosis in Skeletally Mature Patients: A Critical Review". The Journal of the American Academy of Orthopaedic Surgeons 23 (12): 714–723. December 2015. doi:10.5435/jaaos-d-14-00037. PMID 26510624.
- ↑ "Disability for Scoliosis | Bross & Frankel" (in en-US). https://brossfrankel.com/disability-qualifications/disability-for-scoliosis/.
- ↑ 11.0 11.1 11.2 Kouwenhoven, Jan-Willem; Vincken, Koen L.; Bartels, Lambertus W.; Castelein, Rene M. (2006). "Analysis of preexistent vertebral rotation in the normal spine.". Spine 31 (13): 1467–1472. doi:10.1097/01.brs.0000219938.14686.b3. PMID 16741456.
- ↑ "Physiotherapy scoliosis-specific exercises - a comprehensive review of seven major schools". Scoliosis and Spinal Disorders 11: 20. 2016. doi:10.1186/s13013-016-0076-9. PMID 27525315.
- ↑ "Effects of the Schroth exercise on idiopathic scoliosis: a meta-analysis". European Journal of Physical and Rehabilitation Medicine 54 (3): 440–449. June 2018. doi:10.23736/S1973-9087.17.04461-6. PMID 28976171.
- ↑ 14.0 14.1 "Effectiveness of scoliosis-specific exercises for adolescent idiopathic scoliosis compared with other non-surgical interventions: a systematic review and meta-analysis". Physiotherapy 105 (2): 214–234. June 2019. doi:10.1016/j.physio.2018.10.004. PMID 30824243. https://ora.ox.ac.uk/objects/uuid:71063c94-7706-41a5-94f7-ca31f097d6ce.
- ↑ Lua error: Internal error: The interpreter exited with status 1. "scoliosis". Dictionary.com Unabridged. Random House. https://www.dictionary.com/browse/Lua error: Internal error: The interpreter exited with status 1.. "Scoliosis Definition & Meaning". http://www.dictionary.com/browse/scoliosis..
- ↑ Aebi, Max (2005). "The Adult Scoliosis". European Spine Journal 14 (10): 925–948. doi:10.1007/s00586-005-1053-9. PMID 16328223. https://doc.rero.ch/record/321519/files/586_2005_Article_1053.pdf. Retrieved 2022-12-21.
- ↑ 17.0 17.1 Nachemson, Alf (1968). "A Long Term Follow-up Study of Non-treated Scoliosis". Acta Orthopaedica Scandinavica 39 (4): 466–476. doi:10.3109/17453676808989664. PMID 5726117. https://www.tandfonline.com/doi/pdf/10.3109/17453676808989664. Retrieved 2022-12-21.
- ↑ Yanner, Baher S. (2021-12-17). "How Scoliosis Affects the Body". Spine Institute of North America. https://spineina.com/blog/how-scoliosis-affects-the-body/#:~:text=Digestive%20systems%3A%20By%20compressing%20the,cause%20nausea%20for%20some%20patients.
- ↑ "Muscular Imbalance: Why Does Scoliosis Create One Weak Side?". Scoliosis SOS Clinic. 2017-08-28. https://www.scoliosissos.com/blog/scoliosis-weak-side#:~:text=The%20condition%20known%20as%20scoliosis,those%20on%20the%20other%20side..
- ↑ 20.0 20.1 Coillard, Christine; Leroux, Michel A.; Prince, François; Rivard, Charles H.; Zabjek, Karl Franc (2008). "Postural Characteristics of Adolescents With Idiopathic Scoliosis". Journal of Pediatric Orthopaedics 28 (2): 218–224. doi:10.1097/BPO.0b013e3181651bdc. PMID 18388718. https://www.researchgate.net/publication/5463283. Retrieved 2023-01-08.
- ↑ "Ectopic calcification: gathering hard facts about soft tissue mineralization". The American Journal of Pathology 154 (3): 671–675. March 1999. doi:10.1016/S0002-9440(10)65313-8. PMID 10079244.
- ↑ "Progression of scoliosis after skeletal maturity in institutionalized adults who have cerebral palsy". The Journal of Bone and Joint Surgery. American Volume 70 (9): 1290–1296. October 1988. doi:10.2106/00004623-198870090-00002. PMID 3182881.
- ↑ "Scoliosis and the respiratory system". Paediatric Respiratory Reviews 7 (2): 152–160. June 2006. doi:10.1016/j.prrv.2006.04.009. PMID 16765303.
- ↑ 24.0 24.1 "Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study". JAMA 289 (5): 559–567. February 2003. doi:10.1001/jama.289.5.559. PMID 12578488.
- ↑ 25.0 25.1 "Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients". The Journal of Bone and Joint Surgery. American Volume 63 (5): 702–712. June 1981. doi:10.2106/00004623-198163050-00003. PMID 6453874.
- ↑ "Idiopathic scoliosis". Deutsches Ärzteblatt International 107 (49): 875–83; quiz 884. December 2010. doi:10.3238/arztebl.2010.0875. PMID 21191550. "It was once assumed, on the basis of studies in heterogeneous patient populations, that patients with untreated adolescent scoliosis would necessarily become wheelchair-dependent in old age and were likely to die of cardiopulmonary arrest for reasons related to scoliosis. This is no longer held to be the case.".
- ↑ Step-Up to Medicine. Step-Up Series. Hagerstwon, MD: Lippincott Williams & Wilkins. 2008. p. 90. ISBN 978-0-7817-7153-5. https://archive.org/details/stepuptomedicine0000agab.
- ↑ 28.0 28.1 28.2 28.3 "The genetic epidemiology of idiopathic scoliosis". European Spine Journal 21 (10): 1905–1919. October 2012. doi:10.1007/s00586-012-2389-6. PMID 22695700.
- ↑ 29.0 29.1 "The search for idiopathic scoliosis genes". Spine 31 (6): 679–681. March 2006. doi:10.1097/01.brs.0000202527.25356.90. PMID 16540873.
- ↑ "Evidence of a linkage between matrilin-1 gene (MATN1) and idiopathic scoliosis". Scoliosis 1: 21. December 2006. doi:10.1186/1748-7161-1-21. PMID 17176459.
- ↑ 31.0 31.1 "Adolescent idiopathic scoliosis and genetic testing". Current Opinion in Pediatrics 22 (1): 67–70. February 2010. doi:10.1097/MOP.0b013e32833419ac. PMID 19949338.
- ↑ "Adolescent idiopathic scoliosis". Nature Reviews. Disease Primers 1: 15030. September 2015. doi:10.1038/nrdp.2015.30. PMID 27188385.
- ↑ "Aetiology of idiopathic scoliosis: current concepts". Pediatric Rehabilitation 6 (3–4): 137–170. 2003. doi:10.1080/13638490310001642757. PMID 14713582.
- ↑ "Paraspinal muscle morphology and composition in adolescent idiopathic scoliosis: A histological analysis". JOR Spine 4 (3): e1169. September 2021. doi:10.1002/jsp2.1169. PMID 34611591.
- ↑ "The pathogenesis of adolescent idiopathic scoliosis: review of the literature". Spine 33 (26): 2898–2908. December 2008. doi:10.1097/BRS.0b013e3181891751. PMID 19092622.
- ↑ "Rate of complications in scoliosis surgery - a systematic review of the Pub Med literature". Scoliosis 3: 9. August 2008. doi:10.1186/1748-7161-3-9. PMID 18681956.
- ↑ "Selective fusion for adolescent idiopathic scoliosis: a review of current operative strategy". European Spine Journal 20 (7): 1048–1057. July 2011. doi:10.1007/s00586-011-1730-9. PMID 21387194.
- ↑ "A multicenter study of the outcomes of the surgical treatment of adolescent idiopathic scoliosis using the Scoliosis Research Society (SRS) outcome instrument". Spine 27 (18): 2046–2051. September 2002. doi:10.1097/00007632-200209150-00015. PMID 12634567.
- ↑ "Comparison of combined anterior-posterior approach versus posterior-only approach in treating adolescent idiopathic scoliosis: a meta-analysis". European Spine Journal 25 (2): 363–371. February 2016. doi:10.1007/s00586-015-3968-0. PMID 25900299.
- ↑ 40.0 40.1 "Analysis of Shoulder Complex Function After Posterior Spinal Fusion in Adolescents With Idiopathic Scoliosis". Journal of Pediatric Orthopedics 39 (1): e32–e38. January 2019. doi:10.1097/BPO.0000000000001267. PMID 30312252.
- ↑ "Prevalence of postoperative pain in adolescent idiopathic scoliosis and the association with preoperative pain". Spine 38 (21): 1848–1852. October 2013. doi:10.1097/brs.0b013e3182a4aa97. PMID 23883827.
- ↑ "Prevalence and predictors of pain in surgical treatment of adolescent idiopathic scoliosis". Spine 36 (10): 825–829. May 2011. doi:10.1097/brs.0b013e3181de8c2b. PMID 21192302.
- ↑ "Athletic activity after spine surgery in children and adolescents: results of a survey". Spine 27 (4): 423–427. February 2002. doi:10.1097/00007632-200202150-00019. PMID 11840110.
- ↑ "Timing and predictors of return to short-term functional activity in adolescent idiopathic scoliosis after posterior spinal fusion: a prospective study". Spine 39 (18): 1471–1478. August 2014. doi:10.1097/brs.0000000000000452. PMID 24875955.
- ↑ 45.0 45.1 45.2 "Idiopathic scoliosis". Deutsches Ärzteblatt International 107 (49): 875–83; quiz 884. December 2010. doi:10.3238/arztebl.2010.0875. PMID 21191550.
- ↑ "What is Scoliosis: What Causes Scoliosis?". MedicalBug. 17 February 2012. http://www.medicalbug.com/what-is-scoliosis-what-causes-scoliosis/.
- ↑ "Congenital Scoliosis". Scoliosis Research Society (SRS). http://www.srs.org/professionals/conditions_and_treatment/congenital_scoliosis/.
- ↑ Toga, Arthur W.; Thompson, Paul M. (2003). "Mapping brain asymmetry". Nat. Rev. Neurosci. 4 (1): 37–48. doi:10.1038/nrn1009. PMID 12511860.
- ↑ 49.0 49.1 de Lussanet, M.H.E. (2019). "Opposite asymmetries of face and trunk and of kissing and hugging, as predicted by the axial twist hypothesis". PeerJ 7: e7096. doi:10.7717/peerj.7096. PMID 31211022.
- ↑ "Segmental neurophysiological mechanisms in scoliosis". The Journal of Bone and Joint Surgery. British Volume 61-B (3): 310–313. August 1979. doi:10.1302/0301-620x.61b3.479254. PMID 479254.
- ↑ POSNA. (2014). Neuromuscular Scoliosis. The Pediatric Orthopaedic Society of North America. "Neuromuscular Scoliosis - POSNA". http://www.posna.org/education/StudyGuide/neuromuscularScoliosis.asp.
- ↑ "Syndromic Scoliosis: National Trends in Surgical Management and Inpatient Hospital Outcomes: A 12-Year Analysis". Spine 44 (22): 1564–1570. November 2019. doi:10.1097/BRS.0000000000003134. PMID 31689252.
- ↑ Komazec, Jovan; Matic, Aleksandra (2009). "Amniotic Band Syndrome". Acta Medica Medianae 48 (2): 44–48. https://publisher.medfak.ni.ac.rs/AMM_1/amm-stari/2009-html/2-broj/AMNIOTIC%20BAND%20SYNDROME.pdf. Retrieved 2023-01-29.
- ↑ "Chiari malformation". Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/chiari-malformation/symptoms-causes/syc-20354010.
- ↑ Marchesi, Chiara; Pareyson, Davide (2009). "Diagnosis, natural history, and management of Charcot-Marie-Tooth disease". The Lancet Neurology 8 (7): 654–667. doi:10.1016/S1474-4422(09)70110-3. PMID 19539237. http://new.c-m-t.cz/wp-content/uploads/2016/01/Diagnosis-natural-history-and-management-of-Charcot%E2%80%93Marie%E2%80%93Tooth-disease.pdf. Retrieved 2023-01-29.
- ↑ Krigger, Karen W. (2006). "Celebral Palsy: An Overview". American Family Physician 73 (1): 91–100. PMID 16417071. https://www.aafp.org/pubs/afp/issues/2006/0101/p91.html. Retrieved 2023-01-29.
- ↑ Chandraekharan, Praveen Kumar; Lakshminrusimha, Satyan; Madappa, Rajeshwari; Rawat, Munmun; Rothstein, David H. (2017). "Congenital Diaphragmatic hernia - a review". Maternal Health, Neonatology and Perinatology 3: 6. doi:10.1186/s40748-017-0045-1. PMID 28331629.
- ↑ 58.0 58.1 58.2 Hresko, M. Timothy (2013). "Idiopathic Scoliosis in Adolescents". The New England Journal of Medicine 368 (9): 834–841. doi:10.1056/NEJMcp1209063. PMID 23445094. https://pedclerk.uchicago.edu/sites/pedclerk.uchicago.edu/files/uploads/scoliosis_0.pdf. Retrieved 2023-01-29.
- ↑ Aartsma-Ra, Annemieke; Duan, Dongsheng; Goemans, Nathalie; Mercuri, Eugenio; Takeda, Shin'ichi (2021). "Duchenne muscular dystrophy". Nature Reviews Disease Primers 7. https://www.nature.com/articles/s41572-021-00248-3.
- ↑ Fuente-Mora, Cristina; Kauffman, Horacio; Mendoza-Santiesteban, Carlos; Norcliffe-Kauffman, Lucy; Palma, Jose-Alberto; Percival, Leila (2014). "Current treatments in familial dysautonomia". Expert Opinion on Pharmacotherapy 15 (18): 2653–2671. doi:10.1517/14656566.2014.970530. PMID 25323828. PMC 4236240. https://www.researchgate.net/publication/267043910. Retrieved 2023-01-29.
- ↑ Blake, Kim D; Prasad, Chitra (2006). "CHARGE syndrome". Orphanet Journal of Rare Diseases 1: 34. doi:10.1186/1750-1172-1-34. PMID 16959034.
- ↑ "Fragile X syndrome". Department for Work and Pensions, UK. http://www.dwp.gov.uk/publications/specialist-guides/medical-conditions/a-z-of-medical-conditions/learning-disability/fragile-x-syndrome-ld.shtml.
- ↑ "Orthopaedic aspects of fragile-X syndrome". The Journal of Bone and Joint Surgery. American Volume 72 (6): 889–896. July 1990. doi:10.2106/00004623-199072060-00015. PMID 2195034.
- ↑ Delatycki, Martin B; Forrest, Susan M; Williamson, Robert (2000). "Freidreich ataxia: an overview". Journal of Medical Genetics 37 (1): 1–8. doi:10.1136/jmg.37.1.1. PMID 10633128. PMC 1734457. https://jmg.bmj.com/content/jmedgenet/37/1/1.full.pdf. Retrieved 2023-01-30.
- ↑ Sheth, Ujash (2021). "Hemihypertrophy". OrthoBullets. https://www.orthobullets.com/pediatrics/4044/hemihypertrophy.
- ↑ Black, James H.; Bowdin, Sarah; Dietz, Harry C.; El-Hamamsy, Ismail; Frischmeyer-Guerrerio, Pamela A.; Guerrerio, Anthony L.; Loeys, Bart; MacCarrick, Gretchen et al. (2014). "Loeys-Dietz syndrome: a primer for diagnosis and management". Genetics in Medicine 16 (8): 576–587. doi:10.1038/gim.2014.11. PMID 24577266.
- ↑ Fryer, G; Green, A; McIntosh, I; Mountford, R; Sweeney, E (2003). "Nail patella syndrome: a review of the phenotype aided by developmental biology". Journal of Medical Genetics 40 (3): 153–162. doi:10.1136/jmg.40.3.153. PMID 12624132. PMC 1735400. https://jmg.bmj.com/content/jmedgenet/40/3/153.full.pdf. Retrieved 2023-01-30.
- ↑ Boyd, Kevin P.; Korf, Bruce R.; Theos, Amy (2009). "Neurofibromatosis type 1". Journal of the American Academy of Dermatology 61 (1): 1–16. doi:10.1016/j.jaad.2008.12.051. PMID 19539839.
- ↑ Glorieux, Francis H; Rauch, Frank (2004). "Osteogenesis imperfecta". The Lancet 363 (9418): 1377–1385. doi:10.1016/S0140-6736(04)16051-0. PMID 15110498. http://publicationslist.org.s3.amazonaws.com/data/frauch/ref-67/Rauch%20OI%20review%20Lancet%202004.pdf. Retrieved 2023-01-30.
- ↑ Cassidy, Suzanne B.; Driscoll, Daniel J.; Miller, Jennifer L.; Schwartz, Stuart (2012). "Prader-Willi syndrome". Genetics in Medicine 14 (1): 10–26. doi:10.1038/gim.0b013e31822bead0. PMID 22237428.
- ↑ Biesecker, Leslie G.; Choyke, Peter L.; Jamis-Dow, Carlos A.; Turner, Joyce (2004). "Radiologic Manifestations of Proteus Syndrome". RadioGraphics 24 (4): 1051–1068. doi:10.1148/rg.244035726. PMID 15256628. https://www.proteus-syndrome.org/uploads/1/1/4/6/114696341/compressed_jamis-dow_et_al.pdf. Retrieved 2023-01-31.
- ↑ Adzick, N Scott; Melchionne, Jeanne; Mitchell, Laura E; Pasquariello, Patrick S; Sutton, Leslie N; Whitehead, Alexander S (2004). "Spina bifida". The Lancet 364 (9448): 1885–1895. doi:10.1016/S0140-6736(04)17445-X. PMID 15555669. https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=186b07a3d4651e28f9ffd0b9bc7ec1c2af33e56b. Retrieved 2023-01-31.
- ↑ Lunn, Mitchell R; Wang, Ching H (2008). "Spinal muscular atrophy". The Lancet 371 (9630): 2120–2133. doi:10.1016/S0140-6736(08)60921-6. PMID 18572081. https://www.academia.edu/18213331. Retrieved 2023-01-31.
- ↑ Vandertop, W. Peter (2014). "Syringomyelia". Neuropediatrics 45 (1): 003–009. doi:10.1055/s-0033-1361921. PMID 24272770.
- ↑ Desmarais, Thomas J.; Keller, Martin S. (2013). "Pectus carinatum". Current Opinion in Pediatrics 25 (3): 375–381. doi:10.1097/MOP.0b013e3283604088. PMID 23657247. https://www.braceworks.ca/wp-content/uploads/2016/08/Desmarais-Keller-2013-Pectus-carinatum.pdf. Retrieved 2023-01-31.
- ↑ Giradi, Federico; Hughes, Alex; Kotwal, Suhel; Pumberger, Matthias (2011). "Degenerative Scoliosis: A Review". HSS Journal 7 (3): 257–264. doi:10.1007/s11420-011-9204-5. PMID 23024623.
- ↑ "Scoliosis symptoms – pain, flat back, screening, self-assessment". iscoliosis.com. http://www.iscoliosis.com/symptoms-screening.html.
- ↑ "Scoliometer (Inclinometer)". National Scoliosis Foundation. http://www.scoliosis.org/store/scoliometer.php.
- ↑ "Scoliosis imaging: what radiologists should know". Radiographics 30 (7): 1823–1842. November 2010. doi:10.1148/rg.307105061. PMID 21057122. "The main purpose of performing CT or MR imaging in a patient with scoliosis is to identify an underlying cause. MR imaging is used with increasing frequency to evaluate patients with an unusual curve pattern or alarming clinical manifestations. Nevertheless, two reasons for performing such screening are plausible: First, the treatment of an underlying neurologic lesion could help alleviate progressive neurologic deterioration and lead to improvement or stabilization of scoliosis; second, surgery performed to correct scoliosis in the presence of an underlying neurologic disorder that has not been identified and treated could result in new or additional neurologic deficits.".
- ↑ "The Scoliosis Quandary: Are Radiation Exposures From Repeated X-Rays Harmful?". Dose-Response 17 (2): 1559325819852810. 2019-04-01. doi:10.1177/1559325819852810. PMID 31217755.
- ↑ "Early Onset Scoliosis | Scoliosis Research Society". http://www.srs.org/patients-and-families/conditions-and-treatments/parents/scoliosis/early-onset-scoliosis.
- ↑ Sponseller PD, Yazici M, Demetracopoulos C, et al. Evidence basisfor management of spine and chest wall deformities in children.Spine(Phila Pa 1976). 2007;32(suppl):S81–S90
- ↑ Celebioglu E., Yataganbaba A., Bekmez S., et al Growing-rod Graduates with Idiopathic Early-onset Scoliosis Have Comparable Exercise Tolerance to Patients with Surgically Treated Adolescent Idiopathic Scoliosis. J. Pediatr. Orthop.. 2020;40(8):e734-e739. doi:10.1097/BPO.0000000000001567
- ↑ "Screening for Adolescent Idiopathic Scoliosis: US Preventive Services Task Force Recommendation Statement". JAMA 319 (2): 165–172. January 2018. doi:10.1001/jama.2017.19342. PMID 29318284.
- ↑ The Complete Scoliosis Surgery Handbook for Patients: An In-Depth and Unbiased Look Into What to Expect Before and During Scoliosis Surgery. Health In Your Hands. p. 89. ISBN 978-9810785925. https://books.google.com/books?id=fLIkBQAAQBAJ&pg=PA89.
- ↑ "Treatment Options | Scoliosis Research Society". https://www.srs.org/patients-and-families/common-questions-and-glossary/frequently-asked-questions/treatment-and-coping.
- ↑ "Treating scoliosis in children". NHS Choices. 19 February 2013. http://www.nhs.uk/Conditions/Scoliosis/Pages/Treatment.aspx.
- ↑ 88.0 88.1 "Effects of corrective, therapeutic exercise techniques on adolescent idiopathic scoliosis. A systematic review". Archivos Argentinos de Pediatria 116 (4): e582–e589. August 2018. doi:10.5546/aap.2018.eng.e582. PMID 30016036.
- ↑ "Scoliosis – Treatment in adults". NHS Choices. 19 February 2013. http://www.nhs.uk/Conditions/Scoliosis/Pages/treatment-adults.aspx.
- ↑ "Idiopathic Scoliosis – Adult Nonoperative Management". Scoliosis Research Society. http://www.srs.org/patient_and_family/scoliosis/idiopathic/adults/nonoperative_management.htm.
- ↑ "Idiopathic Scoliosis – Adult Surgical Treatment". Scoliosis Research Society. http://www.srs.org/patient_and_family/scoliosis/idiopathic/adults/surgical_treatment.htm.
- ↑ "Exercises reduce the progression rate of adolescent idiopathic scoliosis: results of a comprehensive systematic review of the literature". Disability and Rehabilitation 30 (10): 772–785. 2008. doi:10.1080/09638280801889568. PMID 18432435.
- ↑ "Exercises for adolescent idiopathic scoliosis". The Cochrane Database of Systematic Reviews 2012 (8): CD007837. August 2012. doi:10.1002/14651858.cd007837.pub2. PMID 22895967.
- ↑ "Review of scoliosis-specific exercise methods used to correct adolescent idiopathic scoliosis". Archives of Physiotherapy 9: 8. 2019. doi:10.1186/s40945-019-0060-9. PMID 31463082.
- ↑ The influence of elastic orthotic belt on sagittal profile in adolescent idiopathic thoracic scoliosis: A comparative radiographic study with Milwaukee brace., Research Gate, September 2010, https://www.researchgate.net/figure/The-same-patient-wearing-Milwaukee-brace-The-neck-ring-cause-a-stimulant-effect-on-the_fig2_46412715
- ↑ "Compliance with night-time overcorrection bracing in adolescent idiopathic scoliosis: Result from a cohort follow-up". Medical Engineering & Physics 77: 137–141. March 2020. doi:10.1016/j.medengphy.2020.01.003. PMID 31992499.
- ↑ "BASIS study". https://basisstudy.org.
- ↑ "To Brace or Not to Brace: The Three-Dimensional Nature and Growth Considerations for Adolescent Idiopathic Scoliosis". Academy Today (The Edge). American Academy of Orthosits and Prosthetist.. 2013. pp. 5–8.
- ↑ 99.0 99.1 Tachdjian's Pediatric Orthopaedics. Philadelphia, PA: W.B. Saunders. 2002. ISBN 978-0-7216-5684-7. https://archive.org/details/tachdjianspediat0002unse.Lua error: Internal error: The interpreter exited with status 1.
- ↑ "Braces for idiopathic scoliosis in adolescents". The Cochrane Database of Systematic Reviews 2015 (6): CD006850. June 2015. doi:10.1002/14651858.CD006850.pub3. PMID 26086959.
- ↑ "Scoliosis Treatment". 19 December 2020. https://www.webmd.com/back-pain/treatment-for-scoliosis#1.
- ↑ 102.0 102.1 102.2 102.3 102.4 Guay, Joanne; Suresh, Santhanam; Kopp, Sandra; Johnson, Rebecca L. (2019-01-16). "Postoperative epidural analgesia versus systemic analgesia for thoraco-lumbar spine surgery in children". The Cochrane Database of Systematic Reviews 1 (1): CD012819. doi:10.1002/14651858.CD012819.pub2. ISSN 1469-493X. PMID 30650189.
- ↑ 103.0 103.1 "Adolescent Idiopathic Scoliosis". Scoliosis Research Society (SRS). http://www.srs.org/patient_and_family/scoliosis/idiopathic/. adolescents/surgical_treatment.htm. Accessed 27 January 2013
- ↑ "Development of a human spine simulation system." (in en). Advances in Therapeutic Engineering. CRC Press. January 2012. p. 27. ISBN 978-1-4398-7174-4. https://books.google.com/books?id=ylLNBQAAQBAJ&pg=PA27.
- ↑ Lin, Yang; Chen, Wenjian; Chen, Anmin; Li, Feng; Xiong, Wei (March 2018). "Anterior versus Posterior Selective Fusion in Treating Adolescent Idiopathic Scoliosis: A Systematic Review and Meta-Analysis of Radiologic Parameters". World Neurosurgery 111: e830–e844. doi:10.1016/j.wneu.2017.12.161. ISSN 1878-8769. PMID 29309975. https://pubmed.ncbi.nlm.nih.gov/29309975/#:~:text=Anterior%20is%20more%20effective%20than,in%20restoring%20the%20sagittal%20curvature..
- ↑ Andreacchio, Antonio; Caretti, Valentina; Colombo, Luca (2022). "Anterior vertebral body tethering as a treatment for scoliosis in skeletally immature patients". La Pediatria Medica e Chirurgica 44 (1): 291. doi:10.4081/pmc.2022.291. PMID 37184319.
- ↑ "Health and Function of Patients With Untreated Idiopathic Scoliosis—Reply.". JAMA 289 (20): 2644; author reply 2644–5. May 2003. doi:10.1001/jama.289.20.2644-a. PMID 12771105.
- ↑ "Many With Scoliosis Can Skip Treatments". stopgettingsick.com. http://www.stopgettingsick.com/templates/news_template.cfm/6427.
- ↑ "Adolescent idiopathic scoliosis: natural history and long term treatment effects". Scoliosis 1 (1): 2. March 2006. doi:10.1186/1748-7161-1-2. PMID 16759428.
- ↑ "Adolescent Idiopathic Scoliosis | Scoliosis Research Society". http://www.srs.org/patients-and-families/conditions-and-treatments/parents/scoliosis/adolescent-idiopathic-scoliosis.
- ↑ "New disease gene location and high genetic heterogeneity in idiopathic scoliosis". European Journal of Human Genetics 19 (8): 865–869. August 2011. doi:10.1038/ejhg.2011.31. PMID 21407261.
- ↑ "Aetiology of idiopathic scoliosis: current concepts". Pediatric Rehabilitation 6 (3–4): 137–70. 2003. doi:10.1080/13638490310001642757. PMID 14713582.
- ↑ Scoliosis: Causes, Symptoms and Treatment. Nova Science Publishers. October 2012. ISBN 978-1-62081-007-1. https://public.ebookcentral.proquest.com/choice/publicfullrecord.aspx?p=3020988.
- ↑ "The scoliosis of Richard III, last Plantagenet King of England: diagnosis and clinical significance". Lancet 383 (9932): 1944. 2014. doi:10.1016/S0140-6736(14)60762-5. PMID 24881996. http://www.richardiii.ca/wp-content/uploads/2017/10/The-Lancet-Richard-III-Scoliosis-053114.pdf.
- ↑ "A dangerous curve: the role of history in America's scoliosis screening programs". American Journal of Public Health 102 (4): 606–616. April 2012. doi:10.2105/AJPH.2011.300531. PMID 22397340.
- ↑ "Scoliosis Surgery". News-medical.net. 22 November 2009. http://www.news-medical.net/health/Scoliosis-Surgery.aspx.
- ↑ 117.0 117.1 117.2 "Idiopathic Scoliosis: Options of Fixation and Fusion of Thoracic Curves". SpineUniverse. 8 February 2013. http://www.spineuniverse.com/conditions/scoliosis/idiopathic-scoliosis-options-fixation-fusion-thoracic-curves.
- ↑ 118.0 118.1 118.2 118.3 118.4 118.5 118.6 "The natural history of human gait and posture. Part 1. Spine and pelvis". Gait & Posture 21 (1): 95–112. January 2005. doi:10.1016/s0966-6362(04)00014-1. PMID 15536039.
- ↑ "Chapter 5". Handbook of Paleoanthropology. Springer Berlin Heidelberg. 2007. pp. 1483–1518.
- ↑ "The evolution of human bipedality: ecology and functional morphology". Journal of Human Evolution 26 (3): 182–202. March 1994. doi:10.1006/jhev.1994.1011.
- ↑ "Early onset scoliosis: what the primary care provider needs to know and implications for practice". Journal of the American Academy of Nurse Practitioners 23 (8): 392–403. August 2011. doi:10.1111/j.1745-7599.2011.00634.x. PMID 21790832.
- ↑ "Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases". The Journal of Bone and Joint Surgery. American Volume 92 (5): 1097–1104. May 2010. doi:10.2106/JBJS.I.00879. PMID 20439654.
- ↑ "Scoliosis Awareness Month | Scoliosis Research Society". https://www.srs.org/patients-and-families/additional-scoliosis-resources/scoliosis-awareness-month.
- ↑ "Recent advances in the treatment of scoliosis in children". British Editorial Society of Bone and Joint Surgery. 2011. http://www.boneandjoint.org.uk/content/recent-advances-treatment-scoliosis-children.
Lua error: Internal error: The interpreter exited with status 1.
External links
- Scoliosis at Curlie
- Early Onset Scoliosis is the abnormal, side-to-side curve of the spine in children under five years old, often including children with congenital scoliosis (present at birth, with spine abnormalities) and infantile scoliosis (birth to three years).
- Questions and Answers about Scoliosis in Children and Adolescents – US National Institute of Arthritis and Musculoskeletal and Skin Diseases
Lua error: Internal error: The interpreter exited with status 1. Lua error: Internal error: The interpreter exited with status 1.
Lua error: Internal error: The interpreter exited with status 1.
