Medicine:Segmental colitis associated with diverticulosis
| Segmental colitis associated with diverticulosis | |
|---|---|
| Other names | SCAD |
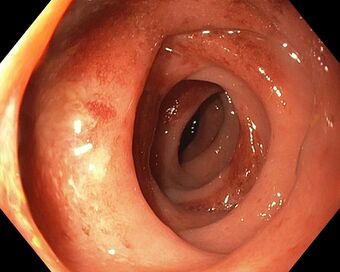 | |
| Endoscopic image of segmental colitis associated with diverticulosis, Type A | |
| Specialty | Gastroenterology |
| Symptoms | Rectal bleeding, Abdominal cramping, Asymptomatic |
| Usual onset | 64 years of age |
| Types | A-D |
| Diagnostic method | Colonoscopy |
| Differential diagnosis | Bacterial colitis, Diverticulitis, NSAID-induced colitis, Crohn's disease, Ulcerative colitis |
| Treatment | Antibiotics, Mesalamine, Prednisone, Surgery |
| Prognosis | Benign |
| Frequency | 0.3 - 1.3% |
Segmental colitis associated with diverticulosis (SCAD) is a condition characterized by localized inflammation in the colon, which spares the rectum and is associated with multiple sac-like protrusions or pouches in the wall of the colon (diverticulosis). Unlike diverticulitis, SCAD involves inflammation of the colon between diverticula (interdiverticular mucosa), while sparing the diverticular orifices. SCAD may lead to abdominal pain, especially in the left lower quadrant, intermittent rectal bleeding and chronic diarrhea.[1]
The cause of SCAD is unknown, but may be related to local colonic ischemia, fecal stasis, or mucosal prolapse. The factors that cause SCAD likely overlap with inflammatory bowel disease. There are four types of SCAD, which are categorized based on the appearance during colonoscopy. Pattern A is characterized by involvement of crescentic folds and is the most common type of SCAD (52%).[2] Pattern B has an appearance similar to mild-to moderate ulcerative colitis (30.40%), whereas pattern C appears similar to Crohn's disease (10.90%).[2] Pattern D is the least common, and appears similar to severe ulcerative colitis (6.50%).[2]
SCAD is diagnosed by colonoscopy. Additional testing may be necessary to rule out infectious causes of colitis. Evaluation should include assessment for additional causes of colitis, such as medication induced (checkpoint inhibitors, NSAIDs, etc.). Laboratory results are usually normal in SCAD, although the white blood cell count may be mildly elevated. Fecal calprotectin, a marker of colon inflammation, may be elevated. Computed tomography of the abdomen is not routinely necessary, but may show thickening or inflammation in the distal colon (sigmoid colon) with associated diverticulosis.
Treatment may consist of antibiotics, aminosalicylates (mesalamine), or prednisone. In rare cases, surgery with segmental resection may be considered. The long term prognosis is likely benign, although data is lacking. The prevalence of SCAD ranges from 0.3 - 1.3 percent.
Types
There are four types of SCAD, based on endoscopic appearance. Pattern A is characterized by involvement of crescentic folds and is the most common type of SCAD (52%).[2] Pattern B has an appearance similar to mild-to moderate ulcerative colitis (30.40%), whereas pattern C appears similar to Crohn's disease (10.90%).[2] Pattern D is the least common, and appears similar to severe ulcerative colitis (6.50%).[2]
Signs and symptoms
People with SCAD may develop left lower quadrant abdominal cramping, intermittent rectal bleeding, and chronic diarrhea.[1] Rectal bleeding (hematochezia) is the most common symptom,[3] and is the presenting complaint in more than 70% of individuals with SCAD.[4] Fever is rare.[5]
Pathophysiology
The cause of segmental colitis associated with diverticula is unknown. Several factors may influence the development of the disease, such as local colonic ischemia, fecal stasis, or mucosal prolapse. SCAD shares some features with inflammatory bowel disease, including the increase of tumor necrosis factor (TNF) alpha during active disease, and decrease in TNF during health improvement. The pathogenesis of SCAD likely overlaps with inflammatory bowel disease.[6]
Diagnosis
SCAD is diagnosed via colonoscopy, often incidentally during examination for unrelated concerns. Colonoscopy shows erythema of the colonic mucosa, which may be characterized by friability and exudate.[1] The descending and sigmoid colon are typically involved. Biopsies of the affected area and the unaffected rectum confirm the diagnosis.[1] Biopsies of SCAD show evidence of chronic inflammation. Rectal biopsies show normal mucosa.
It is important and occasional difficult to distinguish SCAD from inflammatory bowel disease (IBD).[1][7] Biopsies reveal histologic findings that are identical in both conditions.[1] However, ulcerative colitis usually affects the rectum and inflammation in IBD extends to areas of the colon without diverticulosis.[1]
Additional causes of colitis should be evaluated, including infectious and medication-induced, particularly NSAID-associated.[1]
Laboratory results are usually normal in individuals with SCAD. The white blood cell count may be mildly elevated. Fecal calprotectin, a marker of colon inflammation, may be elevated in individuals with SCAD.[8] Fecal calprotectin may assist in distinguishing SCAD from irritable bowel syndrome.[8]
Imaging tests, including CT abdomen, may show inflammation or thickening of the distal colon, with associated diverticulosis. There may be evidence of inflammation extending around the bowel (fat stranding).
Treatment
There are several options in treatment for SCAD. Data is lacking, and there are no prospective trials comparing different therapies for SCAD. As of 2017, there are no guidelines available to direct treatment.[6] Treatment may include antibiotics, aminosalicylates, and corticosteroids. Antibiotics include ciprofloxacin and metronidazole, given for 14 days. If symptoms recur after improvement with antibiotics, a second course of antibiotics may be given.
If an initial course of antibiotics is ineffective, then mesalamine may be tried. If mesalamine is ineffective, then a course of prednisone may be helpful. In severe cases of SCAD, where corticosteroids are unable to be discontinued, then surgery may be considered (segmental resection).
Prognosis
The natural history of SCAD lacks rigorous study, with little data regarding long term outcomes. However, the course appears to largely benign. In cases that require surgery, recurrence of disease is rare.[9] Long term medication therapy is rarely necessary.[6] Over a course of 7 years, about half of people with SCAD experience a recurrence of symptoms.[10] About a third of people have a mild recurrence.[10]
Epidemiology
Among individuals with diverticulosis, the prevalence of SCAD ranges from 0.3 - 1.3%.[11] SCAD is more common in men.[5][11][12] SCAD often occurs in elderly individuals, with an average of 64 years upon diagnosis.[11][12]
History
SCAD was first described in a case series in 1984.[13] SCAD was initially believed to represent a complication of diverticular disease.[14] As evidence suggested increasing overlap with inflammatory bowel disease, SCAD became recognized as a distinct condition.[14]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Lamps, Laura W.; Knapple, Whitfield L. (January 2007). "Diverticular Disease–Associated Segmental Colitis". Clinical Gastroenterology and Hepatology 5 (1): 27–31. doi:10.1016/j.cgh.2006.10.024. PMID 17234553.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Tursi, A; Elisei, W; Brandimarte, G; Giorgetti, GM; Lecca, PG; Di Cesare, L; Inchingolo, CD; Aiello, F (May 2010). "The endoscopic spectrum of segmental colitis associated with diverticulosis.". Colorectal Disease 12 (5): 464–70. doi:10.1111/j.1463-1318.2009.01969.x. PMID 19558591.
- ↑ Imperiali, G; Meucci, G; Alvisi, C; Fasoli, R; Ferrara, A; Girelli, CM; Rocca, F; Saibeni, S et al. (April 2000). "Segmental colitis associated with diverticula: a prospective study. Gruppo di Studio per le Malattie Infiammatorie Intestinali (GSMII).". The American Journal of Gastroenterology 95 (4): 1014–6. doi:10.1111/j.1572-0241.2000.01943.x. PMID 10763952.
- ↑ Freeman, HJ (28 September 2016). "Segmental colitis associated diverticulosis syndrome.". World Journal of Gastroenterology 22 (36): 8067–9. doi:10.3748/wjg.v22.i36.8067. PMID 27688648.
- ↑ 5.0 5.1 Freeman, HJ (June 2023). "Segmental Colitis Associated with Diverticulosis (SCAD).". Current Gastroenterology Reports 25 (6): 130–133. doi:10.1007/s11894-023-00871-y. PMID 37129830.
- ↑ 6.0 6.1 6.2 Schembri, J; Bonello, J; Christodoulou, DK; Katsanos, KH; Ellul, P (2017). "Segmental colitis associated with diverticulosis: is it the coexistence of colonic diverticulosis and inflammatory bowel disease?". Annals of Gastroenterology 30 (3): 257–261. doi:10.20524/aog.2017.0126. PMID 28469355.
- ↑ Cassieri, C; Brandimarte, G; Elisei, W; Lecca, GP; Goni, E; Penna, A; Picchio, M; Tursi, A (October 2016). "How to Differentiate Segmental Colitis Associated With Diverticulosis and Inflammatory Bowel Diseases.". Journal of Clinical Gastroenterology 50 (Suppl 1): S36-8. doi:10.1097/MCG.0000000000000630. PMID 27622359.
- ↑ 8.0 8.1 Tursi, A; Elisei, W; Giorgetti, G; Aiello, F; Brandimarte, G (September 2011). "Role of fecal calprotectin in the diagnosis and treatment of segmental colitis associated with diverticulosis.". Minerva Gastroenterologica e Dietologica 57 (3): 247–55. PMID 21769075.
- ↑ Guslandi, M (January 2003). "Segmental colitis: so what?". European Journal of Gastroenterology & Hepatology 15 (1): 1–2. doi:10.1097/00042737-200301000-00001. PMID 12544686.
- ↑ 10.0 10.1 Imperiali, G; Terpin, MM; Meucci, G; Ferrara, A; Minoli, G (June 2006). "Segmental colitis associated with diverticula: a 7-year follow-up study.". Endoscopy 38 (6): 610–2. doi:10.1055/s-2006-924985. PMID 16612745.
- ↑ 11.0 11.1 11.2 Mann, NS; Hoda, KK (October 2012). "Segmental colitis associated with diverticulosis: systematic evaluation of 486 cases with meta-analysis.". Hepato-gastroenterology 59 (119): 2119–21. doi:10.5754/hge11043. PMID 23435130.
- ↑ 12.0 12.1 Mulhall, AM; Mahid, SS; Petras, RE; Galandiuk, S (June 2009). "Diverticular disease associated with inflammatory bowel disease-like colitis: a systematic review.". Diseases of the Colon and Rectum 52 (6): 1072–9. doi:10.1007/DCR.0b013e31819ef79a. PMID 19581849.
- ↑ Sladen, GE; Filipe, MI (August 1984). "Is segmental colitis a complication of diverticular disease?". Diseases of the Colon and Rectum 27 (8): 513–4. doi:10.1007/BF02555508. PMID 6147239.
- ↑ 14.0 14.1 Tursi, A (January 2011). "Segmental colitis associated with diverticulosis: complication of diverticular disease or autonomous entity?". Digestive Diseases and Sciences 56 (1): 27–34. doi:10.1007/s10620-010-1230-5. PMID 20411418.

