Medicine:Crohn's disease
| Crohn's disease | |
|---|---|
| Other names | Crohn disease, Crohn syndrome, granulomatous enteritis, regional enteritis, Leśniowski-Crohn disease |
| Error creating thumbnail: Unable to save thumbnail to destination | |
| The three most common sites of intestinal involvement in Crohn's disease (left) compared to the areas affected by ulcerative colitis (colitis ulcerosa, right) | |
| Specialty | Gastroenterology |
| Symptoms | Abdominal pain, diarrhea (may be bloody), fever, weight loss,[1] fatigue, mouth sores, reduced appetite[2] |
| Complications | Anemia, skin rashes, arthritis, bowel cancer[1] |
| Usual onset | 20 to 30[3] |
| Duration | Long term[1] |
| Risk factors | Tobacco smoking[4] |
| Diagnostic method | Biopsy, medical imaging[1] |
| Differential diagnosis | Irritable bowel syndrome, celiac disease, Behçet's disease, nonsteroidal anti-inflammatory drug enteropathy, intestinal tuberculosis[1][5] |
| Medication | Corticosteroids, biological therapy, immunosuppressants such as azathioprine, methotrexate[1] |
| Prognosis | Slightly increased risk of death[6] |
| Frequency | 3.2 per 1,000 (developed world)[7] |
Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any segment of the gastrointestinal tract.[3] Symptoms often include abdominal pain, diarrhea, fever, abdominal distension, and weight loss.[1][3] Complications outside of the gastrointestinal tract may include anemia, skin rashes, arthritis, inflammation of the eye, and fatigue.[1] The skin rashes may be due to infections as well as pyoderma gangrenosum or erythema nodosum.[1] Bowel obstruction may occur as a complication of chronic inflammation, and those with the disease are at greater risk of colon cancer and small bowel cancer.[1]
Although the precise causes of Crohn's disease (CD) are unknown, it is believed to be caused by a combination of environmental, immune, and bacterial factors in genetically susceptible individuals.[3][8][9][10] It results in a chronic inflammatory disorder, in which the body's immune system defends the gastrointestinal tract, possibly targeting microbial antigens.[9][11] While Crohn's is an immune-related disease, it does not appear to be an autoimmune disease (the immune system is not triggered by the body itself).[12] The exact underlying immune problem is not clear; however, it may be an immunodeficiency state.[11][13][14]
About half of the overall risk is related to genetics, with more than 70 genes involved.[1][15] Tobacco smokers are three times as likely to develop Crohn's disease as non-smokers.[4] It often begins after gastroenteritis.[1] Other conditions with similar symptoms include irritable bowel syndrome and Behçet's disease.[1]
There is no known cure for Crohn's disease.[1][3] Treatment options are intended to help with symptoms, maintain remission, and prevent relapse.[1] In those newly diagnosed, a corticosteroid may be used for a brief period of time to rapidly improve symptoms, alongside another medication such as either methotrexate or a thiopurine used to prevent recurrence.[1] Cessation of smoking is recommended for people with Crohn's disease.[1] One in five people with the disease is admitted to the hospital each year, and half of those with the disease will require surgery at some point over a ten-year period.[1] While surgery should be used as little as possible, it is necessary to address some abscesses, certain bowel obstructions, and cancers.[1] Checking for bowel cancer via colonoscopy is recommended every few years, starting eight years after the disease has begun.[1]
Crohn's disease affects about 3.2 per 1,000 people in Europe and North America;[7] it is less common in Asia and Africa.[16][17] It has historically been more common in the developed world.[18] Rates have, however, been increasing, particularly in the developing world, since the 1970s.[17][18] Inflammatory bowel disease resulted in 47,400 deaths in 2015,[19] and those with Crohn's disease have a slightly reduced life expectancy.[1] It tends to start in adolescence and young adulthood, though it can occur at any age.[20][1][3][21] Males and females are equally affected.[3]
Name controversy
The disease was named after gastroenterologist Burrill Bernard Crohn, who in 1932, together with Leon Ginzburg (1898–1988) and Gordon D. Oppenheimer (1900–1974) at Mount Sinai Hospital in New York, described a series of patients with inflammation of the terminal ileum of the small intestine, the area most commonly affected by the illness.[22] Why the disease was named after Crohn has controversy around it.[23][24] While Crohn in his memoir describes his original investigation of the disease, Ginzburg provided strong evidence how he and Oppenheimer were the first to study the disease.[25]
Signs and symptoms
Gastrointestinal

Many people with Crohn's disease have symptoms for years before the diagnosis.[26] The usual onset is in the teens and twenties, but can occur at any age.[21][1] Because of the 'patchy' nature of the gastrointestinal disease and the depth of tissue involvement, initial symptoms can be more subtle than those of ulcerative colitis. People with Crohn's disease experience chronic recurring periods of flare-ups and remission.[27] The symptoms experienced can change over time as inflammation increases and spreads. Symptoms can also be different depending on which organs are involved. It is generally thought that the presentation of Crohn's disease is different for each patient due to the high variability of symptoms, organ involvement, and initial presentation.
Perianal
Perianal discomfort may also be prominent in Crohn's disease. Itchiness or pain around the anus may be suggestive of inflammation of the anus, or perianal complications such as anal fissures, fistulae, or abscesses around the anal area.[1] Perianal skin tags are also common in Crohn's disease, and may appear with or without the presence of colorectal polyps.[28] Fecal incontinence may accompany perianal Crohn's disease.
Intestines
The intestines, especially the colon and terminal ileum, are the most commonly affected areas of the body. Abdominal pain is a common initial symptom of Crohn's disease,[3] especially in the lower right abdomen.[29] Flatulence, bloating, and abdominal distension are additional symptoms and may also add to the intestinal discomfort. Pain is often accompanied by diarrhea, which may or may not be bloody. Inflammation in different areas of the intestinal tract can affect the quality of the feces. Ileitis typically results in large-volume, watery feces, while colitis may result in a smaller volume of feces of higher frequency. Fecal consistency may range from solid to watery. In severe cases, an individual may have more than 20 bowel movements per day, and may need to awaken at night to defecate.[1][30][31][32] Visible bleeding in the feces is less common in Crohn's disease than in ulcerative colitis, but is not unusual.[1] Bloody bowel movements are usually intermittent, and may be bright red, dark maroon, or even black in color. The color of bloody stool depends on the location of the bleed. In severe Crohn's colitis, bleeding may be copious.[30]
Stomach and esophagus
The stomach is rarely the sole or predominant site of CD. To date there are only a few documented case reports of adults with isolated gastric CD and no reports in the pediatric population. Isolated stomach involvement is very unusual presentation accounting for less than 0.07% of all gastrointestinal CD.[33] Rarely, the esophagus and stomach may be involved in Crohn's disease. These can cause symptoms including difficulty swallowing (dysphagia), upper abdominal pain, and vomiting.[34]
Oropharynx (mouth)
The mouth may be affected by recurrent sores (aphthous ulcers). Recurrent aphthous ulcers are common; however, it is not clear whether this is due to Crohn's disease or simply that they are common in the general population. Other findings may include diffuse or nodular swelling of the mouth, a cobblestone appearance inside the mouth, granulomatous ulcers, or pyostomatitis vegetans. Medications that are commonly prescribed to treat CD, such as anti-inflammatory and sulfa-containing drugs, may cause lichenoid drug reactions in the mouth. Fungal infection such as candidiasis is also common due to the immunosuppression required in the treatment of the disease. Signs of anemia such as pallor and angular cheilitis or glossitis are also common due to nutritional malabsorption.[35]
People with Crohn's disease are also susceptible to angular stomatitis, an inflammation of the corners of the mouth, and pyostomatitis vegetans.[36]
Systemic
Like many other chronic, inflammatory diseases, Crohn's disease can cause a variety of systemic symptoms.[1] Among children, growth failure is common. Many children are first diagnosed with Crohn's disease based on inability to maintain growth.[37] As it may manifest at the time of the growth spurt in puberty, up to 30% of children with Crohn's disease may have retardation of growth.[38] Fever may also be present, though fevers greater than 38.5 °C (101.3 °F) are uncommon unless there is a complication such as an abscess.[1] Among older individuals, Crohn's disease may manifest as weight loss, usually related to decreased food intake, since individuals with intestinal symptoms from Crohn's disease often feel better when they do not eat and might lose their appetite.[37] People with extensive small intestine disease may also have malabsorption of carbohydrates or lipids, which can further exacerbate weight loss.[39]
Extraintestinal
Crohn's disease can affect many organ systems beyond the gastrointestinal tract.[40]
Visual
Inflammation of the interior portion of the eye, known as uveitis, can cause blurred vision and eye pain, especially when exposed to light (photophobia).[41] Uveitis can lead to loss of vision if untreated.[40]
Inflammation may also involve the white part of the eye (sclera) or the overlying connective tissue (episclera), which causes conditions called scleritis and episcleritis, respectively.[41]
Other very rare ophthalmological manifestations include: conjunctivitis, glaucoma, and retinal vascular disease.[42]
Gallbladder and liver
Crohn's disease that affects the ileum may result in an increased risk of gallstones. This is due to a decrease in bile acid resorption in the ileum, and the bile gets excreted in the stool. As a result, the cholesterol/bile ratio increases in the gallbladder, resulting in an increased risk for gallstones.[41] Although the association is greater in the context of ulcerative colitis, Crohn's disease may also be associated with primary sclerosing cholangitis, a type of inflammation of the bile ducts.[43]
Liver involvement of Crohn's disease can include cirrhosis and steatosis. Nonalcoholic fatty liver disease (nonalcoholic steatohepatitis, NAFLD) are relatively common and can slowly progress to end-stage liver disease. NAFLD sensitizes the liver to injury and increases the risk of developing acute or chronic liver failure following another liver injury.[42]
Other rare hepatobiliary manifestations of Crohn's disease include: cholangiocarcinoma, granulomatous hepatitis, cholelithiasis, autoimmune hepatitis, hepatic abscess, and pericholangitis.[42]
Renal and urological
Nephrolithiasis, obstructive uropathy, and fistulization of the urinary tract directly result from the underlying disease process. Nephrolithiasis is due to calcium oxalate or uric acid stones. Calcium oxalate is due to hyperoxaluria typically associated with either distal ileal CD or ileal resection. Oxalate absorption increases in the presence of unabsorbed fatty acids in the colon. The fatty acids compete with oxalate to bind calcium, displacing the oxalate, which can then be absorbed as unbound sodium oxalate across colonocytes and excreted into the urine. Because sodium oxalate only is absorbed in the colon, calcium-oxalate stones form only in patients with an intact colon. Patients with an ileostomy are prone to formation of uric-acid stones because of frequent dehydration. The sudden onset of severe abdominal, back, or flank pain in patients with IBD, particularly if different from the usual discomfort, should lead to inclusion of a renal stone in the differential diagnosis.[42]
Urological manifestations in patients with IBD may include ureteral calculi, enterovesical fistula, perivesical infection, perinephric abscess, and obstructive uropathy with hydronephrosis. Ureteral compression is associated with retroperitoneal extension of the phlegmonous inflammatory process involving the terminal ileum and cecum, and may result in hydronephrosis severe enough to cause hypertension.[42]
Immune complex glomerulonephritis presenting with proteinuria and hematuria has been described in children and adults with CD or UC. Diagnosis is by renal biopsy, and treatment parallels the underlying IBD.[42]
Amyloidosis (see endocrinological involvement) secondary to Crohn's disease has been described and is known to affect the kidneys.[42]
Pancreatic
Pancreatitis may be associated with both UC and CD. The most common cause is iatrogenic and involves sensitivity to medications used to treat IBD (3% of patients), including sulfasalazine, mesalamine, 6-mercaptopurine, and azathioprine. Pancreatitis may present as symptomatic (in 2%) or more commonly asymptomatic (8–21%) disease in adults with IBD.[42]
Cardiovascular and circulatory
Children and adults with IBD have been rarely (<1%) reported developing pleuropericarditis either at initial presentation or during active or quiescent disease. The pathogenesis of pleuropericarditis is unknown, although certain medications (e.g., sulfasalazine and mesalamine derivatives) have been implicated in some cases. The clinical presentation may include chest pain, dyspnea, or in severe cases pericardial tamponade requiring rapid drainage. Nonsteroidal anti-inflammatory drugs have been used as therapy, although this should be weighed against the hypothetical risk of exacerbating the underlying IBD.[42]
In rare cases, cardiomyopathy, endocarditis, and myocarditis have been described.[42]
Crohn's disease also increases the risk of blood clots;[41] painful swelling of the lower legs can be a sign of deep venous thrombosis, while difficulty breathing may be a result of pulmonary embolism.
Respiratory
Laryngeal involvement in inflammatory bowel disease is extremely rare. Only 12 cases of laryngeal involvement in Crohn's disease have been reported as of 2019[update]. Moreover, only one case of laryngeal manifestations in ulcerative colitis has been reported as of that date.[44] Nine patients complained of difficulty in breathing due to edema and ulceration from the larynx to the hypopharynx.[45] Hoarseness, sore throat, and odynophagia are other symptoms of laryngeal involvement of Crohn's disease.[46]
Considering extraintestinal manifestations of CD, those involving the lung are relatively rare. However, there is a wide array of lung manifestations, ranging from subclinical alterations, airway diseases and lung parenchymal diseases to pleural diseases and drug-related diseases. The most frequent manifestation is bronchial inflammation and suppuration with or without bronchiectasis. There are a number of mechanisms by which the lungs may become involved in CD. These include the same embryological origin of the lung and gastrointestinal tract by ancestral intestine, similar immune systems in the pulmonary and intestinal mucosa, the presence of circulating immune complexes and auto-antibodies, and the adverse pulmonary effects of some drugs.[47] A complete list of known pulmonary manifestations include: fibrosing alveolitis, pulmonary vasculitis, apical fibrosis, bronchiectasis, bronchitis, bronchiolitis, tracheal stenosis, granulomatous lung disease, and abnormal pulmonary function.[42]
Musculoskeletal
Crohn's disease is associated with a type of rheumatologic disease known as seronegative spondyloarthropathy.[41] This group of diseases is characterized by inflammation of one or more joints (arthritis) or muscle insertions (enthesitis).[41] The arthritis in Crohn's disease can be divided into two types. The first type affects larger weight-bearing joints such as the knee (most common), hips, shoulders, wrists, or elbows.[41] The second type symmetrically involves five or more of the small joints of the hands and feet.[41] The arthritis may also involve the spine, leading to ankylosing spondylitis if the entire spine is involved, or simply sacroiliitis if only the sacroiliac joint is involved.[41]
Crohn's disease increases the risk of osteoporosis or thinning of the bones.[41] Individuals with osteoporosis are at increased risk of bone fractures.[48]
Dermatological

Crohn's disease may also involve the skin, blood, and endocrine system. Erythema nodosum is the most common type of skin problem, occurring in around 8% of people with Crohn's disease, producing raised, tender red nodules usually appearing on the shins.[41][49][50] Erythema nodosum is due to inflammation of the underlying subcutaneous tissue, and is characterized by septal panniculitis.[49]
Pyoderma gangrenosum is a less common skin problem, occurring in under 2%,[50] and is typically a painful ulcerating nodule.[49][40]
Clubbing, a deformity of the ends of the fingers, may also be a result of Crohn's disease.
psoriasis It is one of the most common within CD and UC.
Other very rare dermatological manifestations include: pyostomatitis vegetans, erythema multiforme, epidermolysis bullosa acquista (described in a case report), and metastatic CD (the spread of Crohn's inflammation to the skin[36]).[42] It is unknown if Sweet's syndrome is connected to Crohn's disease.[42]
Neurological
Crohn's disease can also cause neurological complications (reportedly in up to 15%).[51] The most common of these are seizures, stroke, myopathy, peripheral neuropathy, headache, and depression.[51]
Central and peripheral neurological disorders are described in patients with IBD and include peripheral neuropathies, myopathies, focal central nervous system defects, convulsions, confusional episodes, meningitis, syncope, optic neuritis, and sensorineural loss. Autoimmune mechanisms are proposed for involvement with IBD. Nutritional deficiencies associated with neurological manifestations, such as vitamin B12 deficiency, should be investigated. Spinal abscess has been reported in both a child and an adult with initial complaints of severe back pain due to extension of a psoas abscess from the epidural space to the subarachnoid space.[42]
Psychiatric and psychological
Crohn's disease is linked to many psychological disorders, including depression and anxiety, denial of one's disease, the need for dependence or dependent behaviors, feeling overwhelmed, and having a poor self-image.[52]
Many studies have found that patients with IBD report a higher frequency of depressive and anxiety disorders than the general population; most studies confirm that women with IBD are more likely than men to develop affective disorders and show that up to 65% of them may have depression and anxiety disorder.[53][54]
Endocrinological or hematological
Autoimmune hemolytic anemia, a condition in which the immune system attacks the red blood cells, is also more common in Crohn's disease and may cause fatigue, a pale appearance, and other symptoms common in anemia.
Secondary amyloidosis (AA) is another rare but serious complication of inflammatory bowel disease (IBD), generally seen in Crohn's disease. At least 1% of patients with Crohn's disease develop amyloidosis. In the literature, the time lapse between the onset of Crohn's disease and the diagnosis of amyloidosis has been reported to range from 1 to 21 years.
Leukocytosis and thrombocytopenia are usually due to immunosuppressant treatments or sulfasalazine. Plasma erythropoietin levels often are lower in patients with IBD than expected, in conjunction with severe anemia.[42]
Thrombocytosis and thromboembolic events resulting from a hypercoagulable state in patients with IBD can lead to pulmonary embolism or thrombosis elsewhere in the body. Thrombosis has been reported in 1.8% of patients with UC and 3.1% of patients with CD. Thromboembolism and thrombosis are less frequently reported among pediatric patients, with three patients with UC and one with CD described in case reports.[42]
In rare cases, hypercoagulation disorders and portal vein thrombosis have been described.[42]
Malnutrition symptoms
People with Crohn's disease may develop anemia due to vitamin B12, folate, iron deficiency, or due to anemia of chronic disease.[55][56] The most common is iron deficiency anemia[55] from chronic blood loss, reduced dietary intake, and persistent inflammation leading to increased hepcidin levels, restricting iron absorption in the duodenum.[56] As Crohn's disease most commonly affects the terminal ileum where the vitamin B12/intrinsic factor complex is absorbed, B12 deficiency may be seen.[56] This is particularly common after surgery to remove the ileum.[55] Involvement of the duodenum and jejunum can impair the absorption of many other nutrients including folate. People with Crohn's often also have issues with small bowel bacterial overgrowth syndrome, which can produce micronutrient deficiencies.[57][58]
Complications
Intestinal damage

Crohn's disease can lead to several mechanical complications within the intestines, including obstruction,[59] fistulae,[60] and abscesses.[61] Obstruction typically occurs from strictures or adhesions that narrow the lumen, blocking the passage of the intestinal contents. A fistula can develop between two loops of bowel, between the bowel and bladder, between the bowel and vagina, and between the bowel and skin. Abscesses are walled-off concentrations of infection, which can occur in the abdomen or in the perianal area. Crohn's is responsible for 10% of vesicoenteric fistulae, and is the most common cause of ileovesical fistulae.[62]
Symptoms caused by intestinal stenosis, or the tightening and narrowing of the bowel, are also common in Crohn's disease. Abdominal pain is often most severe in areas of the bowel with stenosis. Persistent vomiting and nausea may indicate stenosis from small bowel obstruction or disease involving the stomach, pylorus, or duodenum.[30]
Intestinal granulomas are a walled-off portions of the intestine by macrophages in order to isolate infections. Granuloma formation is more often seen in younger patients, and mainly in the severe, active penetrating disease.[63] Granuloma is considered the hallmark of microscopic diagnosis in Crohn's disease (CD), but granulomas can be detected in only 21–60% of CD patients.[63]
Cancer
Crohn's disease also increases the risk of cancer in the area of inflammation. For example, individuals with Crohn's disease involving the small bowel are at higher risk for small intestinal cancer.[64] Similarly, people with Crohn's colitis have a relative risk of 5.6 for developing colon cancer.[65] Screening for colon cancer with colonoscopy is recommended for anyone who has had Crohn's colitis for at least eight years.[66]
Some studies suggest there is a role for chemoprotection in the prevention of colorectal cancer in Crohn's involving the colon; two agents have been suggested, folate and mesalamine preparations.[67] Also, immunomodulators and biologic agents used to treat this disease may promote developing extra-intestinal cancers.[68]
Some cancers, such as acute myelocytic leukaemia have been described in cases of Crohn's disease.[42] Hepatosplenic T-cell lymphoma (HSTCL) is a rare, lethal disease generally seen in young male patients with inflammatory bowel disease. TNF-α Inhibitor treatments (infliximab, adalimumab, certolizumab, natalizumab, and etanercept) are thought to be the cause of this rare disease.[69]

Major complications
Major complications of Crohn's disease include bowel obstruction, abscesses, free perforation, and hemorrhage, which in rare cases may be fatal.[70][71]
Other complications
Individuals with Crohn's disease are at risk of malnutrition for many reasons, including decreased food intake and malabsorption. The risk increases following resection of the small bowel. Such individuals may require oral supplements to increase their caloric intake, or in severe cases, total parenteral nutrition (TPN). Most people with moderate or severe Crohn's disease are referred to a dietitian for assistance in nutrition.[72]
Small intestinal bacterial overgrowth (SIBO) is characterized by excessive proliferation of colonic bacterial species in the small bowel. Potential causes of SIBO include fistulae, strictures, or motility disturbances. Hence, patients with Crohn's disease are especially predisposed to develop SIBO. As result, CD patients may experience malabsorption and report symptoms such as weight loss, watery diarrhea, meteorism, flatulence, and abdominal pain, mimicking acute flare in these patients.[58]
Pregnancy
Crohn's disease can be problematic during pregnancy, and some medications can cause adverse outcomes for the fetus or mother. Consultation with an obstetrician and gastroenterologist about Crohn's disease and all medications facilitates preventive measures. In some cases, remission occurs during pregnancy. Certain medications can also lower sperm count or otherwise adversely affect a man's fertility.[73]
Ostomy-related complications
Common complications of an ostomy (a common surgery in Crohn's disease) are: mucosal edema, peristomal dermatitis, retraction, ostomy prolapse, mucosal/skin detachment, hematoma, necrosis, parastomal hernia, and stenosis.[74]
Etiology
The etiology of Crohn's disease is unknown. Many theories have been disputed, with four main theories hypothesized to be the primary mechanism of Crohn's disease. In autoimmune diseases, antibodies and T lymphocytes are the primary mode of inflammation. These cells and bodies are part of the adaptive immune system, or the part of the immune system that learns to fight foreign bodies when first identified.[75] Autoinflammatory diseases are diseases where the innate immune system, or the immune system we are genetically coded with, is designed to attack our own cells.[76] Crohn's disease likely has involvement of both the adaptive and innate immune systems.[77]
Autoinflammatory theory
Crohn's disease can be described as a multifactorial autoinflammatory disease. The etiopathogenesis of Crohn's disease is still unknown. In any event, a loss of the regulatory capacity of the immune apparatus would be implicated in the onset of the disease. In this respect interestingly enough, as for Blau's disease (a monogenic autoinflammatory disease), the NOD2 gene mutations have been linked to Crohn's disease. However, in Crohn's disease, NOD2 mutations act as a risk factor, being more common among Crohn's disease patients than the background population, while in Blau's disease NOD2 mutations are linked directly to this syndrome, as it is an autosomal-dominant disease. All this new knowledge in the pathogenesis of Crohn's disease allows us to put this multifactorial disease in the group of autoinflammatory syndromes.[76]
Some examples of how the innate immune system affects bowel inflammation have been described.[77] A meta-analysis of CD genome-wide association studies revealed 71 distinct CD-susceptibility loci. Interestingly, three very important CD-susceptibility genes (the intracellular pathogen-recognition receptor, NOD2; the autophagy-related 16-like 1, ATG16L1 and the immunity-related GTPase M, IRGM) are involved in innate immune responses against gut microbiota, while one (the X-box binding protein 1) is involved in regulation of the [adaptive] immune pathway via MHC class II,[78] resulting in autoinflammatory inflammation. Studies have also found that increased ILC3 can overexpress major histocompatibility complex (MHC) II. MHC class II can induce CD4+ T cell apoptosis, thus avoiding the T cell response to normal bowel micro bacteria. Further studies of IBD patients compared with non-IBD patients found that the expression of MHC II by ILC3 was significantly reduced in IBD patients, thus causing an immune reaction against intestinal cells or normal bowel bacteria and damaging the intestines. This can also make the intestines more susceptible to environmental factors, such as food or bacteria.[77]
The thinking is that because Crohn's disease has strong innate immune system involvement and has NOD2 mutations as a predisposition, Crohn's disease is more likely an autoinflammatory disease than an autoimmune disease.[77]
Immunodeficiency theory
A substantial body of data has emerged in recent years to suggest that the primary defect in Crohn's disease is actually one of relative immunodeficiency.[79] This view has been bolstered recently by novel immunological and clinical studies that have confirmed gross aberrations in this early response, consistent with subsequent genetic studies that highlighted molecules important for innate immune function. The suggestion therefore is that Crohn's pathogenesis actually results from partial immunodeficiency, a theory that coincides with the frequent recognition of a virtually identical, non-infectious inflammatory bowel disease arising in patients with congenital monogenic disorders impairing phagocyte function.[79]
Risk factors
While the exact cause or causes are unknown, Crohn's disease seems to be due to a combination of environmental factors and genetic predisposition.[80] Crohn's is the first genetically complex disease in which the relationship between genetic risk factors and the immune system is understood in considerable detail.[81] Each individual risk mutation makes a small contribution to the overall risk of Crohn's (approximately 1:200). The genetic data, and direct assessment of immunity, indicates a malfunction in the innate immune system.[82] In this view, the chronic inflammation of Crohn's is caused when the adaptive immune system tries to compensate for a deficient innate immune system.[83]
Genetics
Crohn's has a genetic component.[85] Because of this, siblings of known people with Crohn's are 30 times more likely to develop Crohn's than the general population.[86]
The first mutation found to be associated with Crohn's was a frameshift in the NOD2 gene (also known as the CARD15 gene),[87] followed by the discovery of point mutations.[88] Over 30 genes have been associated with Crohn's; a biological function is known for most of them. For example, one association is with mutations in the XBP1 gene, which is involved in the unfolded protein response pathway of the endoplasmic reticulum.[89][90] The gene variants of NOD2/CARD15 seem to be related with small-bowel involvement.[91] Other well documented genes which increase the risk of developing Crohn's disease are ATG16L1,[92] IL23R,[93] IRGM,[94] and SLC11A1.[95] There is considerable overlap between susceptibility loci for IBD and mycobacterial infections.[96] Genome-wide association studies have shown that Crohn's disease is genetically linked to coeliac disease.[97]
Crohn's has been linked to the gene LRRK2 with one variant potentially increasing the risk of developing the disease by 70%, while another lowers it by 25%. The gene is responsible for making a protein, which collects and eliminates waste product in cells, and is also associated with Parkinson's disease.[98]
Immune system
There was a prevailing view that Crohn's disease is a primary T cell autoimmune disorder; however, a newer theory hypothesizes that Crohn's results from an impaired innate immunity.[99] The later hypothesis describes impaired cytokine secretion by macrophages, which contributes to impaired innate immunity and leads to a sustained microbial-induced inflammatory response in the colon, where the bacterial load is high.[9][82] Another theory is that the inflammation of Crohn's was caused by an overactive Th1 and Th17 cytokine response.[100][101]
In 2007, the ATG16L1 gene was implicated in Crohn's disease, which may induce autophagy and hinder the body's ability to attack invasive bacteria.[92] Another study theorized that the human immune system traditionally evolved with the presence of parasites inside the body and that the lack thereof due to modern hygiene standards has weakened the immune system. Test subjects were reintroduced to harmless parasites, with positive responses.[102]
Microbes
It is hypothesized that maintenance of commensal microorganism growth in the GI tract is dysregulated, either as a result or cause of immune dysregulation.[103][104]
There is an apparent connection between Crohn's disease, Mycobacterium, other pathogenic bacteria, and genetic markers.[105][106] A number of studies have suggested a causal role for Mycobacterium avium subspecies paratuberculosis (MAP), which causes a similar disease, Johne's disease, in cattle.[107][108] In many individuals, genetic factors predispose individuals to Mycobacterium avium subsp. paratuberculosis infection. This bacterium may produce certain compounds containing mannose, which may protect both itself and various other bacteria from phagocytosis, thereby possibly causing a variety of secondary infections.[109]
NOD2 is a gene involved in Crohn's genetic susceptibility. It is associated with macrophages' diminished ability to phagocytize MAP. This same gene may reduce innate and adaptive immunity in gastrointestinal tissue and impair the ability to resist infection by the MAP bacterium.[110] Macrophages that ingest the MAP bacterium are associated with high production of TNF-α.[111][112]
Other studies have linked specific strains of enteroadherent E. coli to the disease.[113] Adherent-invasive Escherichia coli (AIEC), more common in people with CD,[114][115][113] have the ability to make strong biofilms compared to non-AIEC strains correlating with high adhesion and invasion indices[116][117] of neutrophils and the ability to block autophagy at the autolysosomal step, which allows for intracellular survival of the bacteria and induction of inflammation.[118] Inflammation drives the proliferation of AIEC and dysbiosis in the ileum, irrespective of genotype.[119] AIEC strains replicate extensively inside macrophages inducing the secretion of very large amounts of TNF-α.[120]
Mouse studies have suggested some symptoms of Crohn's disease, ulcerative colitis, and irritable bowel syndrome have the same underlying cause. Biopsy samples taken from the colons of all three patient groups were found to produce elevated levels of a serine protease.[121] Experimental introduction of the serine protease into mice has been found to produce widespread pain associated with irritable bowel syndrome, as well as colitis, which is associated with all three diseases.[122] Regional and temporal variations in those illnesses follow those associated with infection with the protozoan Blastocystis.[123]
The "cold-chain" hypothesis is that psychrotrophic bacteria such as Yersinia and Listeria species contribute to the disease. A statistical correlation was found between the advent of the use of refrigeration in the United States and various parts of Europe and the rise of the disease.[124][125][126]
There is also a tentative association between Candida colonization and Crohn's disease.[127]
Still, these relationships between specific pathogens and Crohn's disease remain unclear.[128][129]
Environmental factors
The increased incidence of Crohn's in the industrialized world indicates an environmental component. Crohn's is associated with an increased intake of animal protein, milk protein, and an increased ratio of omega-6 to omega-3 polyunsaturated fatty acids.[130] Those who consume vegetable proteins appear to have a lower incidence of Crohn's disease. Consumption of fish protein has no association.[130] Smoking increases the risk of the return of active disease (flares).[4] The introduction of hormonal contraception in the United States in the 1960s is associated with a dramatic increase in incidence, and one hypothesis is that these drugs work on the digestive system in ways similar to smoking.[131] Isotretinoin is associated with Crohn's.[132][133][134]
Although stress is sometimes claimed to exacerbate Crohn's disease, there is no concrete evidence to support such claim.[3] Still, it is well known that immune function is related to stress.[135] Dietary microparticles, such as those found in toothpaste, have been studied as they produce effects on immunity, but they were not consumed in greater amounts in patients with Crohn's.[136][137] The use of doxycycline has also been associated with increased risk of developing inflammatory bowel diseases.[138][139][140] In one large retrospective study, patients who were prescribed doxycycline for their acne had a 2.25-fold greater risk of developing Crohn's disease.[139]
Pathophysiology
During a colonoscopy, biopsies of the colon are often taken to confirm the diagnosis. Certain characteristic features of the pathology seen point toward Crohn's disease; it shows a transmural pattern of inflammation, meaning the inflammation may span the entire depth of the intestinal wall.[1]
Granulomas, aggregates of macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. The granulomas of Crohn's disease do not show "caseation", a cheese-like appearance on microscopic examination characteristic of granulomas associated with infections, such as tuberculosis. Biopsies may also show chronic mucosal damage, as evidenced by blunting of the intestinal villi, atypical branching of the crypts, and a change in the tissue type (metaplasia). One example of such metaplasia, Paneth cell metaplasia, involves the development of Paneth cells (typically found in the small intestine and a key regulator of intestinal microbiota) in other parts of the gastrointestinal system.[141][142]
Diagnosis
The diagnosis of Crohn's disease can sometimes be challenging,[26] and many tests are often required to assist the physician in making the diagnosis.[30] Even with a full battery of tests, it may not be possible to diagnose Crohn's with complete certainty; a colonoscopy is approximately 70% effective in diagnosing the disease, with further tests being less effective. Disease in the small bowel is particularly difficult to diagnose, as a traditional colonoscopy allows access to only the colon and lower portions of the small intestines; introduction of the capsule endoscopy[143] aids in endoscopic diagnosis. Giant (multinucleate) cells, a common finding in the lesions of Crohn's disease, are less common in the lesions of lichen nitidus.[144]
-
Endoscopic image of Crohn's colitis showing deep ulceration
-
CT scan showing Crohn's disease in the fundus of the stomach
-
Section of colectomy showing transmural inflammation
-
Resected ileum from a person with Crohn's disease
Classification
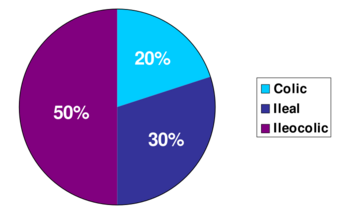
Crohn's disease is one type of inflammatory bowel disease (IBD). It typically manifests in the gastrointestinal tract and can be categorized by the specific tract region affected.
Gastroduodenal Crohn's disease causes inflammation in the stomach and the first part of the small intestine called the duodenum. Jejunoileitis causes spotty patches of inflammation in the top half of the small intestine, called the jejunum.[145] The disease can attack any part of the digestive tract, from mouth to anus. However, individuals affected by the disease rarely fall outside these three classifications, with presentations in other areas.[1]
Crohn's disease may also be categorized by the behavior of disease as it progresses. These categorizations formalized in the Vienna classification of the disease.[146] There are three categories of disease presentation in Crohn's disease: stricturing, penetrating, and inflammatory. Stricturing disease causes narrowing of the bowel that may lead to bowel obstruction or changes in the caliber of the feces. Penetrating disease creates abnormal passageways (fistulae) between the bowel and other structures, such as the skin. Inflammatory disease (or nonstricturing, nonpenetrating disease) causes inflammation without causing strictures or fistulae.[146][147]
Endoscopy
A colonoscopy is the best test for making the diagnosis of Crohn's disease, as it allows direct visualization of the colon and the terminal ileum, identifying the pattern of disease involvement. On occasion, the colonoscope can travel past the terminal ileum, but it varies from person to person. During the procedure, the gastroenterologist can also perform a biopsy, taking small samples of tissue for laboratory analysis, which may help confirm a diagnosis. As 30% of Crohn's disease involves only the ileum,[1] cannulation of the terminal ileum is required in making the diagnosis. Finding a patchy distribution of disease, with involvement of the colon or ileum, but not the rectum, is suggestive of Crohn's disease, as are other endoscopic stigmata.[148] The utility of capsule endoscopy for this, however, is still uncertain.[149]
Radiologic tests
A small bowel follow-through may suggest the diagnosis of Crohn's disease and is useful when the disease involves only the small intestine. Because colonoscopy and gastroscopy allow direct visualization of only the terminal ileum and beginning of the duodenum, they cannot be used to evaluate the remainder of the small intestine. As a result, a barium follow-through X-ray, wherein barium sulfate suspension is ingested and fluoroscopic images of the bowel are taken over time, is useful for looking for inflammation and narrowing of the small bowel.[148][150] Barium enemas, in which barium is inserted into the rectum and fluoroscopy is used to image the bowel, are rarely used in the work-up of Crohn's disease due to the advent of colonoscopy. They remain useful for identifying anatomical abnormalities when strictures of the colon are too small for a colonoscope to pass through, or in the detection of colonic fistulae (in this case contrast should be performed with iodate substances).[151]
CT and MRI scans are useful for evaluating the small bowel with enteroclysis protocols.[152] They are also useful for looking for intra-abdominal complications of Crohn's disease, such as abscesses, small bowel obstructions, or fistulae.[153] Magnetic resonance imaging (MRI) is another option for imaging the small bowel as well as looking for complications, though it is more expensive and less readily available.[154] MRI techniques such as diffusion-weighted imaging and high-resolution imaging are more sensitive in detecting ulceration and inflammation compared to CT.[155][156]
Blood tests
A complete blood count may reveal anemia, which commonly is caused by blood loss leading to iron deficiency or by vitamin B12 deficiency, usually caused by ileal disease impairing vitamin B12 absorption. Rarely autoimmune hemolysis may occur.[157] Ferritin levels help assess if iron deficiency is contributing to the anemia. Erythrocyte sedimentation rate (ESR) and C-reactive protein help assess the degree of inflammation, which is important as ferritin can also be raised in inflammation.[158]
Other causes of anemia include medication used in treatment of inflammatory bowel disease, like azathioprine, which can lead to cytopenia, and sulfasalazine, which can also result in folate deficiency. Testing for Saccharomyces cerevisiae antibodies (ASCA) and antineutrophil cytoplasmic antibodies (ANCA) has been evaluated to identify inflammatory diseases of the intestine[159] and to differentiate Crohn's disease from ulcerative colitis.[160] Furthermore, increasing amounts and levels of serological antibodies such as ASCA, antilaminaribioside [Glc(β1,3)Glb(β); ALCA], antichitobioside [GlcNAc(β1,4)GlcNAc(β); ACCA], antimannobioside [Man(α1,3)Man(α)AMCA], antiLaminarin [(Glc(β1,3))3n(Glc(β1,6))n; anti-L] and antichitin [GlcNAc(β1,4)n; anti-C] associate with disease behavior and surgery, and may aid in the prognosis of Crohn's disease.[161][162][163][164]
Low serum levels of vitamin D are associated with Crohn's disease.[165] Further studies are required to determine the significance of this association.[165]
Comparison with ulcerative colitis
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.[1][30][31]
Differential diagnosis
Other conditions with similar symptoms as Crohn's disease includes intestinal tuberculosis, Behçet's disease, ulcerative colitis, nonsteroidal anti-inflammatory drug enteropathy, irritable bowel syndrome and celiac disease.[5] Irritable bowel syndrome is excluded when there are inflammatory changes.[5] Celiac disease cannot be excluded if specific antibodies (anti-transglutaminase antibodies) are negative,[166][167] nor in absence of intestinal villi atrophy.[168][169]
Management
There is no cure for Crohn's disease and remission may not be possible or prolonged if achieved. In cases where remission is possible, relapse can be prevented and symptoms controlled with medication, lifestyle and dietary changes, changes to eating habits (eating smaller amounts more often), reduction of stress, moderate activity, and exercise. Surgery is generally contraindicated and has not been shown to prevent relapse. Adequately controlled, Crohn's disease may not significantly restrict daily living.[170] Treatment for Crohn's disease involves first treating the acute problem and its symptoms, then maintaining remission of the disease.
Lifestyle changes
Certain lifestyle changes can reduce symptoms, including dietary adjustments, elemental diet, proper hydration, and smoking cessation. Patients with Crohn's disease are very interested in diet. Recent reviews underlined the importance to adopt diets that are best supported by evidence, even if little is known about the impact of diets on these patients.[171][172] Diets that include higher levels of fiber and fruit are associated with reduced risk, while diets rich in total fats, polyunsaturated fatty acids, meat, and omega-6 fatty acids may increase the risk of Crohn's.[173] Maintaining a balanced diet with proper portion control can help manage symptoms of the disease. Eating small meals frequently instead of big meals may also help with a low appetite. A food diary may help with identifying foods that trigger symptoms. Despite the recognized importance of dietary fiber for intestinal health, some people should follow a low residue diet to control acute symptoms especially if foods high in insoluble fiber cause symptoms, e.g., due to obstruction or irritation of the bowel.[170] Some find relief in eliminating casein (a protein found in cow's milk) and gluten (a protein found in wheat, rye and barley) from their diets. They may have specific dietary intolerances (not allergies), for example, lactose.[174] Fatigue can be helped with regular exercise, a healthy diet, and enough sleep, and for those with malabsorption of vitamin B12 due to disease or surgical resection of the terminal ileum, cobalamin injections. Smoking may worsen symptoms and the course of the disease, and stopping is recommended. Alcohol consumption can also worsen symptoms, and moderation or cessation is advised.[170]
Medication
Acute treatment uses medications to treat any infection (normally antibiotics) and to reduce inflammation (normally aminosalicylate anti-inflammatory drugs and corticosteroids). When symptoms are in remission, treatment enters maintenance, with a goal of avoiding the recurrence of symptoms. Prolonged use of corticosteroids has significant side-effects; as a result, they are, in general, not used for long-term treatment. Alternatives include aminosalicylates alone, though only a minority are able to maintain the treatment, and many require immunosuppressive drugs.[175] It has been also suggested that antibiotics change the enteric flora, and their continuous use may pose the risk of overgrowth with pathogens such as Clostridium difficile.[176]
Medications used to treat the symptoms of Crohn's disease include 5-aminosalicylic acid (5-ASA) formulations, prednisone, immunomodulators such as azathioprine (given as the prodrug for 6-mercaptopurine), methotrexate,[177] and anti-TNF therapies and monoclonal antibodies, such as infliximab, adalimumab,[31] certolizumab,[178] vedolizumab, ustekinumab,[179] natalizumab,[180][181]risankizumab-rzaa, and upadacitinib[182] Hydrocortisone should be used in severe attacks of Crohn's disease.[183] Biological therapies are medications used to avoid long-term steroid use, decrease inflammation, and treat people who have fistulas with abscesses.[29] The monoclonal antibody ustekinumab appears to be a safe treatment option, and may help people with moderate to severe active Crohn's disease.[184] The long term safety and effectiveness of monoclonal antibody treatment is not known.[184] The monoclonal antibody briakinumab is not effective for people with active Crohn's disease and it is no longer being manufactured.[184]
The gradual loss of blood from the gastrointestinal tract, as well as chronic inflammation, often leads to anemia, and professional guidelines suggest routinely monitoring for this.[185][186][187]
Immunosuppressant therapies, infection risks and vaccinations
Many patients affected by Crohn's disease need immunosuppressant therapies, which are known to be associated with a higher risk of contracting opportunistic infectious diseases and of pre-neoplastic or neoplastic lesions such as cervical high-grade dysplasia and cancer.[188][189] Many of these potentially harmful diseases, such as Hepatitis B, Influenza, chickenpox, herpes zoster virus, pneumococcal pneumonia, or human papilloma virus, can be prevented by vaccines. Each drug used in the treatment of IBD should be classified according to the degree of immunosuppression induced in the patient. Several guidelines suggest investigating patients’ vaccination status before starting any treatment and performing vaccinations against Vaccine-preventable disease when required.[190][191] Compared to the rest of the population, patients affected by IBD are known to be at higher risk of contracting some vaccine-preventable diseases such as flu and pneumonia.[192] Nevertheless, despite the increased risk of infections, vaccination rates in IBD patients are known to be suboptimal and may also be lower than vaccination rates in the general population.[193][194]
Surgery
Crohn's cannot be cured by surgery, as the disease eventually recurs, though it is used in the case of partial or full blockage of the intestine.[195] Surgery may also be required for complications such as obstructions, fistulas, or abscesses, or if the disease does not respond to drugs. After the first surgery, Crohn's usually comes back at the site where the diseased intestine was removed and the healthy ends were rejoined; it can also come back in other locations. After a resection, scar tissue builds up, which can cause strictures, which form when the intestines become too small to allow excrement to pass through easily, which can lead to a blockage. After the first resection, another resection may be necessary within five years.[196] For patients with an obstruction due to a stricture, two options for treatment are strictureplasty and resection of that portion of bowel. There is no statistical significance between strictureplasty alone versus strictureplasty and resection in cases of duodenal involvement. In these cases, re-operation rates were 31% and 27%, respectively, indicating that strictureplasty is a safe and effective treatment for selected people with duodenal involvement.[197]
Postsurgical recurrence of Crohn's disease is relatively common. Crohn's lesions are nearly always found at the site of the resected bowel. The join (or anastomosis) after surgery may be inspected, usually during a colonoscopy, and disease activity graded. The "Rutgeert's score" is an endoscopic scoring system for postoperative disease recurrence in Crohn's disease. Mild postsurgical recurrences of Crohn's disease are graded i1 and i2, moderate to severe recurrences are graded i3 and i4.[198] Fewer lesions result in a lower grade. Based on the score, treatment plans can be designed to give the patient the best chance of managing the recurrence of the disease.[199]
Short bowel syndrome (SBS, also short gut syndrome or simply short gut) is caused by the surgical removal of part of the small intestine. It usually develops in those patients who have had half or more of their small intestines removed.[200] Diarrhea is the main symptom, but others may include weight loss, cramping, bloating, and heartburn. Short bowel syndrome is treated with changes in diet, intravenous feeding, vitamin and mineral supplements, and treatment with medications. In some cases of SBS, intestinal transplant surgery may be considered; though the number of transplant centres offering this procedure is quite small and it comes with a high risk due to the chance of infection and rejection of the transplanted intestine.[201]
Bile acid diarrhea is another complication following surgery for Crohn's disease in which the terminal ileum has been removed. This leads to the development of excessive watery diarrhea. It is usually thought to be due to an inability of the ileum to reabsorb bile acids after resection of the terminal ileum and was the first type of bile acid malabsorption recognized.[202]
Microbiome modification
The use of oral probiotic supplements to modify the composition and behaviour of the gastrointestinal microbiome has been researched to understand whether it may help to improve remission rate in people with Crohn's disease. However, only two controlled trials were available in 2020, with no clear overall evidence of higher remission nor lower adverse effects, in people with Crohn's disease receiving probiotic supplementation.[203]
Mental health
Crohn's may result in anxiety or mood disorders, especially in young people who may have stunted growth or embarrassment from fecal incontinence.[204] Counselling as well as antidepressant or anxiolytic medication may help some people manage.[204]
As of 2017[update] there is a small amount of research looking at mindfulness-based therapies, hypnotherapy, and cognitive behavioural therapy.[205]
Alternative medicine
It is common for people with Crohn's disease to try complementary or alternative therapy.[206] These include diets, probiotics, fish oil, and other herbal and nutritional supplements.
- Acupuncture is used to treat inflammatory bowel disease in China , and is being used more frequently in Western society.[207] At this time, evidence is insufficient to recommend the use of acupuncture.[206]
- A 2006 survey in Germany found that about half of people with IBD used some form of alternative medicine, with the most common being homeopathy, and a study in France found that about 30% used alternative medicine.[208] Homeopathic preparations are not proven with this or any other condition,[209][210][211] with large-scale studies finding them to be no more effective than a placebo.[212][213][214]
- There are contradicting studies regarding the effect of medical cannabis on inflammatory bowel disease,[215] and its effects on management are uncertain.[216]
Prognosis
Crohn's disease is a chronic condition for which there is no known cure. It is characterised by periods of improvement followed by episodes when symptoms flare up. With treatment, most people achieve a healthy weight, and the mortality rate for the disease is relatively low. It can vary from being benign to very severe, and people with CD could experience just one episode or have continuous symptoms. It usually reoccurs, although some people can remain disease-free for years or decades. Up to 80% of people with Crohn's disease are hospitalized at some point during the course of their disease, with the highest rate occurring in the first year after diagnosis.[6] Most people with Crohn's live a normal lifespan.[217] However, Crohn's disease is associated with a small increase in risk of small bowel and colorectal carcinoma (bowel cancer).[218]
Epidemiology
The percentage of people with Crohn's disease has been determined in Norway and the United States and is similar at 6 to 7.1:100,000. The Crohn's & Colitis Foundation of America cites this number as approx 149:100,000; NIH cites 28 to 199 per 100,000.[219][220] Crohn's disease is more common in northern countries, and with higher rates still in the northern areas of these countries.[221] The incidence of Crohn's disease is thought to be similar in Europe but lower in Asia and Africa.[219] It also has a higher incidence in Ashkenazi Jews[1][222] and smokers.[223]
Crohn's disease begins most commonly in people in their teens and 20s, and people in their 50s through to their 70s.[1][30][21] It is rarely diagnosed in early childhood. It usually affects female children more severely than males.[224] However, only slightly more women than men have Crohn's disease.[225] Parents, siblings or children of people with Crohn's disease are 3 to 20 times more likely to develop the disease.[226] Twin studies find that if one has the disease there is a 55% chance the other will too.[227]
The incidence of Crohn's disease is increasing in Europe[228] and in newly industrialised countries.[229] For example, in Brazil, there has been an annual increase of 11% in the incidence of Crohn's disease since 1990.[229]
History
Inflammatory bowel diseases were described by Giovanni Battista Morgagni (1682–1771) and by Scottish physician Thomas Kennedy Dalziel in 1913.[230]
Ileitis terminalis was first described by Polish surgeon Antoni Leśniowski in 1904, although it was not conclusively distinguished from intestinal tuberculosis.[231] In Poland, it is still called Leśniowski-Crohn's disease (Polish: choroba Leśniowskiego-Crohna). Burrill Bernard Crohn, an American gastroenterologist at New York City 's Mount Sinai Hospital, described fourteen cases in 1932, and submitted them to the American Medical Association under the rubric of "Terminal ileitis: A new clinical entity". Later that year, he, along with colleagues Leon Ginzburg and Gordon Oppenheimer, published the case series "Regional ileitis: a pathologic and clinical entity". However, due to the precedence of Crohn's name in the alphabet, it later became known in the worldwide literature as Crohn's disease.[22]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 "Crohn's disease". Lancet 380 (9853): 1590–605. August 2012. doi:10.1016/S0140-6736(12)60026-9. PMID 22914295.
- ↑ "Crohn's disease". https://www.autoimmuneregistry.org/crohns-disease.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 "Crohn's Disease". https://www.niddk.nih.gov/health-information/digestive-diseases/crohns-disease/all-content.
- ↑ 4.0 4.1 4.2 "Tobacco and IBD: relevance in the understanding of disease mechanisms and clinical practice". Best Practice & Research. Clinical Gastroenterology 18 (3): 481–96. June 2004. doi:10.1016/j.bpg.2003.12.003. PMID 15157822.
- ↑ 5.0 5.1 5.2 "Inflammatory Bowel Disease". World Gastroenterology Organization. August 2015. http://www.worldgastroenterology.org/UserFiles/file/guidelines/inflammatory-bowel-disease-english-2015.pdf.
- ↑ 6.0 6.1 "ACG Clinical Guideline: Management of Crohn's Disease in Adults". The American Journal of Gastroenterology 113 (4): 481–517. April 2018. doi:10.1038/ajg.2018.27. PMID 29610508.
- ↑ 7.0 7.1 "Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review". Gastroenterology 142 (1): 46–54.e42; quiz e30. January 2012. doi:10.1053/j.gastro.2011.10.001. PMID 22001864. http://www.gastrojournal.org/article/S0016508511013783/pdf. Retrieved October 7, 2022.
- ↑ "Recent insights into the genetics of inflammatory bowel disease". Gastroenterology 140 (6): 1704–12. May 2011. doi:10.1053/j.gastro.2011.02.046. PMID 21530736.
- ↑ 9.0 9.1 9.2 "Innate immunity in Crohn's disease: the reverse side of the medal". Journal of Clinical Gastroenterology 42 (Suppl 3 Pt 1): S144–7. September 2008. doi:10.1097/MCG.0b013e3181662c90. PMID 18806708.
- ↑ "New insights into inflammatory bowel disease pathophysiology: paving the way for novel therapeutic targets". Current Drug Targets 9 (5): 413–8. May 2008. doi:10.2174/138945008784221170. PMID 18473770.
- ↑ 11.0 11.1 "Crohn's disease: an immune deficiency state". Clinical Reviews in Allergy & Immunology 38 (1): 20–31. February 2010. doi:10.1007/s12016-009-8133-2. PMID 19437144.
- ↑ "Revisiting Crohn's disease as a primary immunodeficiency of macrophages". The Journal of Experimental Medicine 206 (9): 1839–43. August 2009. doi:10.1084/jem.20091683. PMID 19687225.
- ↑ "Mycobacteria in Crohn's disease: how innate immune deficiency may result in chronic inflammation". Expert Review of Clinical Immunology 6 (4): 633–41. July 2010. doi:10.1586/eci.10.29. PMID 20594136.
- ↑ "Crohn's disease: innate immunodeficiency?". World Journal of Gastroenterology 12 (42): 6751–5. November 2006. doi:10.3748/wjg.v12.i42.6751. PMID 17106921.
- ↑ "Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease". Nature Genetics 40 (8): 955–62. August 2008. doi:10.1038/ng.175. PMID 18587394.
- ↑ "Inflammatory bowel disease in Asia: a systematic review". Journal of Gastroenterology and Hepatology 27 (8): 1266–80. August 2012. doi:10.1111/j.1440-1746.2012.07150.x. PMID 22497584.
- ↑ 17.0 17.1 "Epidemiology and clinical course of Crohn's disease: results from observational studies". World Journal of Gastroenterology 18 (15): 1723–31. April 2012. doi:10.3748/wjg.v18.i15.1723. PMID 22553396.
- ↑ 18.0 18.1 "Inflammatory bowel disease epidemiology". Current Opinion in Gastroenterology 29 (4): 357–62. July 2013. doi:10.1097/MOG.0b013e32836229fb. PMID 23695429.
- ↑ (( GBD 2015 Mortality Causes of Death Collaborators)) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". The Lancet 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMID 27733281.
- ↑ Shih, I-Lun; Lee, Tsung-Chun; Tu, Chia-Hung; Chang, Chin-Chen; Wang, Yu-Fen; Tseng, Yao-Hui; Chiu, Han-Mo; Wu, Ming-Shiang et al. (2016-12-01). "Intraobserver and interobserver agreement for identifying extraluminal manifestations of Crohn's disease with magnetic resonance enterography" (in en). Advances in Digestive Medicine 3 (4): 174–180. doi:10.1016/j.aidm.2015.05.004.
- ↑ 21.0 21.1 21.2 "Crohn's Disease: Get Facts on Symptoms and Diet". http://www.emedicinehealth.com/crohn_disease/article_em.htm.
- ↑ 22.0 22.1 "Regional ileitis: a pathologic and clinical entity. 1932". The Mount Sinai Journal of Medicine, New York 67 (3): 263–8. May 2000. PMID 10828911.
- ↑ Van Hootegem, Philippe; Travis, Simon (2020-07-09). "Is Crohn's Disease a Rightly Used Eponym?" (in en). Journal of Crohn's and Colitis 14 (6): 867–871. doi:10.1093/ecco-jcc/jjz183. ISSN 1873-9946. PMID 31701137. https://academic.oup.com/ecco-jcc/article/14/6/867/5614546.
- ↑ Mulder, Daniel J.; Noble, Angela J.; Justinich, Christopher J.; Duffin, Jacalyn M. (May 2014). "A tale of two diseases: The history of inflammatory bowel disease" (in en). Journal of Crohn's and Colitis 8 (5): 341–348. doi:10.1016/j.crohns.2013.09.009. PMID 24094598.
- ↑ Ginzburg, Leon (May 1986). "Regional enteritis: Historical perspective" (in en). Gastroenterology 90 (5): 1310–1311. doi:10.1016/0016-5085(86)90419-1. PMID 3514360.
- ↑ 26.0 26.1 "Identification of a prodromal period in Crohn's disease but not ulcerative colitis". The American Journal of Gastroenterology 95 (12): 3458–62. December 2000. doi:10.1111/j.1572-0241.2000.03361.x. PMID 11151877.
- ↑ "Johne's Disease and Crohn's Disease". Diagnosis and Control of Johne's Disease. Washington, DC: National Academies Press. 2003. doi:10.17226/10625. Bookshelf ID: NBK207651. ISBN 978-0-309-08611-0. https://www.ncbi.nlm.nih.gov/books/NBK207651/. Retrieved August 30, 2017.
- ↑ "The histology of anal skin tags in Crohn's disease: an aid to confirmation of the diagnosis". International Journal of Colorectal Disease 4 (3): 197–9. August 1989. doi:10.1007/BF01649703. PMID 2769004.
- ↑ 29.0 29.1 "What I need to know about Crohn's Disease". http://www.niddk.nih.gov/health-information/health-topics/digestive-diseases/crohns-disease/Pages/ez.aspx#symptoms.
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 Crohn Disease at eMedicine
- ↑ 31.0 31.1 31.2 "Inflammatory bowel disease". The New England Journal of Medicine 347 (6): 417–29. August 2002. doi:10.1056/NEJMra020831. PMID 12167685. http://gut.bmj.com/cgi/content/short/39/Suppl_1/A15. Retrieved September 4, 2018.
- ↑ "Anorectal functional disorders in the absence of anorectal inflammation in patients with Crohn's disease". The British Journal of Surgery 89 (8): 1027–31. August 2002. doi:10.1046/j.1365-2168.2002.02173.x. PMID 12153630.
- ↑ Ingle, Sachin B; Hinge, Chitra R; Dakhure, Sarita; Bhosale, Smita S (May 16, 2013). "Isolated gastric Crohn's disease". World Journal of Clinical Cases 1 (2): 71–73. doi:10.12998/wjcc.v1.i2.71. ISSN 2307-8960. PMID 24303469.
- ↑ "Gastroduodenal Crohn's disease". Gastrointestinal Endoscopy 60 (6): 985. December 2004. doi:10.1016/S0016-5107(04)02200-X. PMID 15605018.
- ↑ "Dermatological Manifestations in Inflammatory Bowel Diseases". J Clin Med 10 (2): 364. January 2021. doi:10.3390/jcm10020364. PMID 33477990.
- ↑ 36.0 36.1 Aberumand, Babak; Howard, Jessica; Howard, John (January 3, 2017). "Metastatic Crohn's Disease: An Approach to an Uncommon but Important Cutaneous Disorder". BioMed Research International 2017: e8192150. doi:10.1155/2017/8192150. ISSN 2314-6133. PMID 28127561.
- ↑ 37.0 37.1 "Inflammatory bowel disease". Archives of Disease in Childhood 91 (5): 426–32. May 2006. doi:10.1136/adc.2005.080481. PMID 16632672.
- ↑ "Problems in diagnosis of IBD in children". The Netherlands Journal of Medicine 50 (2): S8–11. February 1997. doi:10.1016/S0300-2977(96)00064-2. PMID 9050326. http://dare.uva.nl/personal/pure/en/publications/problems-in-diagnosis-of-ibd-in-children(59612226-ecf5-49df-8848-d79d03f0c5c8).html. Retrieved September 4, 2018.
- ↑ "Nutrition and gastrointestinal disease". Scandinavian Journal of Gastroenterology. Supplement 220: 52–9. 1996. doi:10.3109/00365529609094750. PMID 8898436.
- ↑ 40.0 40.1 40.2 "The First European Evidence-based Consensus on Extra-intestinal Manifestations in Inflammatory Bowel Disease". Journal of Crohn's & Colitis 10 (3): 239–54. March 2016. doi:10.1093/ecco-jcc/jjv213. PMID 26614685.
- ↑ 41.00 41.01 41.02 41.03 41.04 41.05 41.06 41.07 41.08 41.09 41.10 "Diagnosis and therapeutic management of extra-intestinal manifestations of inflammatory bowel disease". Drugs 72 (18): 2333–49. December 2012. doi:10.2165/11638120-000000000-00000. PMID 23181971.
- ↑ 42.00 42.01 42.02 42.03 42.04 42.05 42.06 42.07 42.08 42.09 42.10 42.11 42.12 42.13 42.14 42.15 42.16 42.17 Jose, Folashade A.; Heyman, Melvin B. (February 2008). "Extraintestinal Manifestations of Inflammatory Bowel Disease". Journal of Pediatric Gastroenterology and Nutrition 46 (2): 124–133. doi:10.1097/MPG.0b013e318093f4b0. ISSN 0277-2116. PMID 18223370.
- ↑ "The Gastrointestinal Tract". Robbins and Cotran: Pathologic Basis of Disease (7th ed.). Philadelphia, Pennsylvania: Elsevier Saunders. July 30, 2004. p. 847. ISBN 978-0-7216-0187-8.
- ↑ Loos, Elke; Lemkens, Peter; Poorten, Vincent Vander; Humblet, Evelien; Laureyns, Griet (January 2019). "Laryngeal Manifestations of Inflammatory Bowel Disease". Journal of Voice 33 (1): 1–6. doi:10.1016/j.jvoice.2017.09.021. ISSN 1873-4588. PMID 29605161. https://pubmed.ncbi.nlm.nih.gov/29605161/. Retrieved September 6, 2021.
- ↑ Hasegawa, Naoko; Ishimoto, Shin-Ichi; Takazoe, Masakazu; Tsunoda, Koichi; Fujimaki, Youko; Shiraishi, Aiko; Kinoshita, Makoto; Okada, Kazunari (July 2009). "Recurrent hoarseness due to inflammatory vocal fold lesions in a patient with Crohn's disease". The Annals of Otology, Rhinology, and Laryngology 118 (7): 532–535. doi:10.1177/000348940911800713. ISSN 0003-4894. PMID 19708494. https://pubmed.ncbi.nlm.nih.gov/19708494/. Retrieved September 6, 2021.
- ↑ Li, Cong J.; Aronowitz, Paul (March 2013). "Sore throat, odynophagia, hoarseness, and a muffled, high-pitched voice". Cleveland Clinic Journal of Medicine 80 (3): 144–145. doi:10.3949/ccjm.80a.12056. ISSN 0891-1150. PMID 23456463.
- ↑ Lu, De-Gan; Ji, Xiao-Qing; Liu, Xun; Li, Hong-Jia; Zhang, Cai-Qing (January 7, 2014). "Pulmonary manifestations of Crohn's disease". World Journal of Gastroenterology 20 (1): 133–141. doi:10.3748/wjg.v20.i1.133. ISSN 1007-9327. PMID 24415866.
- ↑ "Maintenance infliximab treatment is associated with improved bone mineral density in Crohn's disease". The American Journal of Gastroenterology 100 (9): 2031–5. September 2005. doi:10.1111/j.1572-0241.2005.50219.x. PMID 16128948.
- ↑ 49.0 49.1 49.2 "Cutaneous manifestations of gastrointestinal disease: part II". Journal of the American Academy of Dermatology 68 (2): 211.e1-33; quiz 244–6. February 2013. doi:10.1016/j.jaad.2012.10.036. PMID 23317981.
- ↑ 50.0 50.1 "Occurrence of skin manifestations in patients of the Swiss Inflammatory Bowel Disease Cohort Study". PLOS ONE 14 (1): e0210436. 2019. doi:10.1371/journal.pone.0210436. PMID 30682031. Bibcode: 2019PLoSO..1410436R.
- ↑ 51.0 51.1 Crohn's disease . professionals.epilepsy.com. Retrieved July 13, 2007.
- ↑ "Mental and Emotional Well-Being". https://www.crohnscolitisfoundation.org/mental-health.
- ↑ Fracas E, Costantino A, Vecchi M, Buoli M. Depressive and Anxiety Disorders in Patients with Inflammatory Bowel Diseases: Are There Any Gender Differences? International Journal of Environmental Research and Public Health. 2023; 20(13):6255. https://doi.org/10.3390/ijerph20136255
- ↑ Barberio B, Zamani M, Black CJ, Savarino EV, Ford AC. Prevalence of symptoms of anxiety and depression in patients with inflammatory bowel disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2021 May;6(5):359-370. doi: 10.1016/S2468-1253(21)00014-5
- ↑ 55.0 55.1 55.2 "Dietary and nutritional considerations for inflammatory bowel disease". The Proceedings of the Nutrition Society 70 (3): 329–35. August 2011. doi:10.1017/S0029665111000097. PMID 21450124.
- ↑ 56.0 56.1 56.2 "The aetiology and impact of malnutrition in paediatric inflammatory bowel disease". Journal of Human Nutrition and Dietetics 24 (4): 313–26. August 2011. doi:10.1111/j.1365-277X.2011.01171.x. PMID 21564345.
- ↑ MedlinePlus Encyclopedia Small bowel bacterial overgrowth
- ↑ 58.0 58.1 Klaus, Jochen; Spaniol, Ulrike; Adler, Guido; Mason, Richard A.; Reinshagen, Max; von Tirpitz C, Christian (July 30, 2009). "Small intestinal bacterial overgrowth mimicking acute flare as a pitfall in patients with Crohn's Disease". BMC Gastroenterology 9 (1): 61. doi:10.1186/1471-230X-9-61. ISSN 1471-230X. PMID 19643023.
 Text was copied from this source, which is available under a Creative Commons Attribution 2.0 Generic (CC BY 2.0) license.
Text was copied from this source, which is available under a Creative Commons Attribution 2.0 Generic (CC BY 2.0) license.
- ↑ "Intestinal Obstruction". http://www.merckmanuals.com/home/digestive-disorders/gastrointestinal-emergencies/intestinal-obstruction.
- ↑ "Anorectal Fistula". http://www.merckmanuals.com/home/digestive-disorders/anal-and-rectal-disorders/anorectal-fistula.
- ↑ "Anorectal Abscess". http://www.merckmanuals.com/home/digestive-disorders/anal-and-rectal-disorders/anorectal-abscess.
- ↑ Enterovesical Fistula at eMedicine
- ↑ 63.0 63.1 Molnár, Tamás; Tiszlavicz, László; Gyulai, Csaba; Nagy, Ferenc; Lonovics, János (May 28, 2005). "Clinical significance of granuloma in Crohn's disease". World Journal of Gastroenterology 11 (20): 3118–3121. doi:10.3748/wjg.v11.i20.3118. ISSN 1007-9327. PMID 15918200.
- ↑ "Strategies for detecting colon cancer in patients with inflammatory bowel disease". The Cochrane Database of Systematic Reviews 2017 (9): CD000279. September 2017. doi:10.1002/14651858.CD000279.pub4. PMID 28922695.
- ↑ "Increased risk of large-bowel cancer in Crohn's disease with colonic involvement". Lancet 336 (8711): 357–9. August 1990. doi:10.1016/0140-6736(90)91889-I. PMID 1975343. https://zenodo.org/record/1258309. Retrieved September 4, 2018.
- ↑ "Consensus conference: Colorectal cancer screening and surveillance in inflammatory bowel disease". Inflammatory Bowel Diseases 11 (3): 314–21. March 2005. doi:10.1097/01.mib.0000160811.76729.d5. PMID 15735438.
- ↑ "Colorectal cancer and dysplasia in inflammatory bowel disease". World Journal of Gastroenterology 14 (17): 2662–9. May 2008. doi:10.3748/wjg.14.2662. PMID 18461651.
- ↑ "Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment". World Journal of Gastroenterology 22 (20): 4794–801. May 2016. doi:10.3748/wjg.v22.i20.4794. PMID 27239106.
- ↑ Parakkal, Deepak; Sifuentes, Humberto; Semer, Rumi; Ehrenpreis, Eli Daniel (November 2011). "Hepatosplenic T-cell lymphoma in patients receiving TNF-α inhibitor therapy: expanding the groups at risk". European Journal of Gastroenterology & Hepatology 23 (12): 1150–1156. doi:10.1097/MEG.0b013e32834bb90a. ISSN 1473-5687. PMID 21941193. https://pubmed.ncbi.nlm.nih.gov/21941193/. Retrieved October 3, 2021.
- ↑ "Man of Many Problems Comes to City for Help". Richmond Times-Dispatch (Richmond, Virginia, USA): p. B1. September 1, 1985. http://infoweb.newsbank.com/iw-search/we/InfoWeb?p_product=AWNB&p_theme=aggregated5&p_action=doc&p_docid=0EB4F60CC90DCE22&p_docnum=2&p_queryname=4.
- ↑ "Kay, Laura Lynn". Richmond Times-Dispatch (Richmond, Virginia, USA). April 3, 2014. http://infoweb.newsbank.com/iw-search/we/InfoWeb?p_product=AWNB&p_theme=aggregated5&p_action=doc&p_docid=14CF552B8BBF3B90&p_docnum=5&p_queryname=1.
"Doris L. Johnson, 82, of Westminster". Carroll County Times (Westminster, Maryland, USA). March 2, 2014. http://infoweb.newsbank.com/iw-search/we/InfoWeb?p_product=AWNB&p_theme=aggregated5&p_action=doc&p_docid=14C4D200CC6C63B0&p_docnum=13&p_queryname=1.
"In memoriam: Dan Hodges Jr.". The Roanoke Times (Roanoke, Virginia, USA). December 31, 2013. http://infoweb.newsbank.com/iw-search/we/InfoWeb?p_product=AWNB&p_theme=aggregated5&p_action=doc&p_docid=14B0CCC8A20C3B78&p_docnum=29&p_queryname=1.
"Cynthia Meredith Routt". Daily Press (Newport News, Virginia, USA): p. A11. May 4, 2014. http://infoweb.newsbank.com/iw-search/we/InfoWeb?p_product=AWNB&p_theme=aggregated5&p_action=doc&p_docid=14D99C943586A6E8&p_docnum=1&p_queryname=1. - ↑ "Home total parenteral nutrition: an alternative to early surgery for complicated inflammatory bowel disease". Journal of Gastrointestinal Surgery 7 (4): 562–566. 2003. doi:10.1016/S1091-255X(02)00132-4. PMID 12763417.
- ↑ "IBD and Pregnancy: What You Need to Know". Crohn's and Colitis Foundation of America. October 21, 2005. http://www.ccfa.org/about/news/pregnancy.
- ↑ Rodrigues, Francielle Profeta; Novaes, Jane Andrea Vieira; Pinheiro, Marcela Monteiro; Martins, Paula; Cunha-Melo, José Renan (October 23, 2019). Intestinal Ostomy Complications and Care. IntechOpen. ISBN 978-1-78984-186-2. https://www.intechopen.com/chapters/67036. Retrieved September 6, 2021.
- ↑ "Definition of Autoimmunity & Autoimmune Disease - Autoimmune Disease | Johns Hopkins Pathology". https://pathology.jhu.edu/autoimmune/definitions.
- ↑ 76.0 76.1 Ciccarelli, F.; Martinis, M. De; Ginaldi, L. (January 2013). "An Update on Autoinflammatory Diseases". Current Medicinal Chemistry 21 (3): 261–269. doi:10.2174/09298673113206660303. ISSN 0929-8673. PMID 24164192.
- ↑ 77.0 77.1 77.2 77.3 Li, Na; Shi, Rui-Hua (January 7, 2018). "Updated review on immune factors in pathogenesis of Crohn's disease". World Journal of Gastroenterology 24 (1): 15–22. doi:10.3748/wjg.v24.i1.15. ISSN 1007-9327. PMID 29358878.
- ↑ Roggenbuck, D.; Reinhold, D.; Baumgart, D. C.; Schierack, P.; Conrad, K.; Laass, M. W. (January 1, 2016), Makowski, Gregory S., ed., "Chapter Two - Autoimmunity in Crohn's Disease—A Putative Stratification Factor of the Clinical Phenotype", Advances in Clinical Chemistry (Elsevier) 77: 77–101, doi:10.1016/bs.acc.2016.06.002, PMID 27717419, https://www.sciencedirect.com/science/article/pii/S0065242316300361, retrieved November 4, 2021
- ↑ 79.0 79.1 Marks, Daniel J. B.; Rahman, Farooq Z.; Sewell, Gavin W.; Segal, Anthony W. (February 2010). "Crohn's Disease: an Immune Deficiency State". Clinical Reviews in Allergy & Immunology 38 (1): 20–31. doi:10.1007/s12016-009-8133-2. ISSN 1080-0549. PMID 19437144.
- ↑ "Immunology of Crohn's disease". Annals of the New York Academy of Sciences 1072 (1): 135–54. August 2006. doi:10.1196/annals.1326.039. PMID 17057196. Bibcode: 2006NYASA1072..135B.
- ↑ "The role of genetics in inflammatory bowel disease". Current Drug Targets 9 (5): 361–8. May 2008. doi:10.2174/138945008784221161. PMID 18473763.
- ↑ 82.0 82.1 "Defective acute inflammation in Crohn's disease: a clinical investigation". Lancet 367 (9511): 668–78. February 2006. doi:10.1016/S0140-6736(06)68265-2. PMID 16503465.
- ↑ "Impaired innate immunity in Crohn's disease". Trends in Molecular Medicine 12 (9): 397–9. September 2006. doi:10.1016/j.molmed.2006.07.005. PMID 16890491.
- ↑ "Crohn's disease risk alleles on the NOD2 locus have been maintained by natural selection on standing variation". Molecular Biology and Evolution 29 (6): 1569–85. June 2012. doi:10.1093/molbev/mss006. PMID 22319155.
- ↑ "Crohn's disease has strong genetic link: study". Crohn's and Colitis Foundation of America. April 16, 2007. http://www.ccfa.org/reuters/geneticlink.
- ↑ "Genetic studies of Crohn's disease: past, present and future". Best Practice & Research. Clinical Gastroenterology 28 (3): 373–86. June 2014. doi:10.1016/j.bpg.2014.04.009. PMID 24913378.
- ↑ "A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease". Nature 411 (6837): 603–6. May 2001. doi:10.1038/35079114. PMID 11385577. Bibcode: 2001Natur.411..603O.
- ↑ "The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease". Gastroenterology 122 (4): 867–74. April 2002. doi:10.1053/gast.2002.32415. PMID 11910337.
- ↑ "XBP1 links ER stress to intestinal inflammation and confers genetic risk for human inflammatory bowel disease". Cell 134 (5): 743–56. September 2008. doi:10.1016/j.cell.2008.07.021. PMID 18775308.
- ↑ "Inflammatory bowel disease, stress, and the endoplasmic reticulum". The New England Journal of Medicine 360 (7): 726–7. February 2009. doi:10.1056/NEJMcibr0809591. PMID 19213688.
- ↑ "NOD2/CARD15: relevance in clinical practice". Best Practice & Research. Clinical Gastroenterology 18 (3): 569–75. June 2004. doi:10.1016/j.bpg.2003.12.008. PMID 15157828.
- ↑ 92.0 92.1 "A nonsynonymous SNP in ATG16L1 predisposes to ileal Crohn's disease and is independent of CARD15 and IBD5". Gastroenterology 132 (5): 1665–71. May 2007. doi:10.1053/j.gastro.2007.03.034. PMID 17484864.
- ↑ "Intestinal DMBT1 expression is modulated by Crohn's disease-associated IL23R variants and by a DMBT1 variant which influences binding of the transcription factors CREB1 and ATF-2". PLOS ONE 8 (11): e77773. 2013. doi:10.1371/journal.pone.0077773. PMID 24223725. Bibcode: 2013PLoSO...877773D.
- ↑ "Independent and population-specific association of risk variants at the IRGM locus with Crohn's disease". Human Molecular Genetics 19 (9): 1828–39. May 2010. doi:10.1093/hmg/ddq041. PMID 20106866.
- ↑ "Crohn's disease and SLC11A1 promoter polymorphism". Digestive Diseases and Sciences 52 (7): 1632–5. July 2007. doi:10.1007/s10620-006-9682-3. PMID 17385031.
- ↑ "Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease". Nature 491 (7422): 119–24. November 2012. doi:10.1038/nature11582. PMID 23128233. Bibcode: 2012Natur.491..119..
- ↑ "An update in the diagnosis of coeliac disease". Histopathology 59 (2): 166–79. August 2011. doi:10.1111/j.1365-2559.2010.03680.x. PMID 21054494. "Recent genome-wide association studies have shown that chronic inflammatory and autoimmune diseases are linked genetically to coeliac disease; for example, type 1 diabetes mellitus, Grave's disease and Crohn's disease.".
- ↑ "A single gene can either raise or lower Crohn's disease risk". New Scientist. January 10, 2018. https://www.newscientist.com/article/single-gene-can-either-raise-lower-crohns-disease-risk/.
- ↑ "Innate immunity in inflammatory bowel disease: a disease hypothesis". The Journal of Pathology 214 (2): 260–6. January 2008. doi:10.1002/path.2291. PMID 18161747.
- ↑ "Defects in mucosal immunity leading to Crohn's disease". Immunological Reviews 206 (1): 277–95. August 2005. doi:10.1111/j.0105-2896.2005.00293.x. PMID 16048555.
- ↑ "Monoclonal anti-interleukin 23 reverses active colitis in a T cell-mediated model in mice". Gastroenterology 132 (7): 2359–70. June 2007. doi:10.1053/j.gastro.2007.03.104. PMID 17570211.
- ↑ "The Worm Turns". The New York Times. June 29, 2008. https://www.nytimes.com/2008/06/29/magazine/29wwln-essay-t.html.
- ↑ "Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis". Nature Clinical Practice. Gastroenterology & Hepatology 3 (7): 390–407. July 2006. doi:10.1038/ncpgasthep0528. PMID 16819502.
- ↑ "Multidrug resistance is common in Escherichia coli associated with ileal Crohn's disease". Inflammatory Bowel Diseases 19 (1): 141–50. January 2013. doi:10.1002/ibd.22971. PMID 22508665.
- ↑ "Replication of Colonic Crohn's Disease Mucosal Escherichia coli Isolates within Macrophages and Their Susceptibility to Antibiotics". Antimicrobial Agents and Chemotherapy 52 (2): 427–34. February 2008. doi:10.1128/AAC.00375-07. PMID 18070962.
- ↑ "Microbial mannan inhibits bacterial killing by macrophages: a possible pathogenic mechanism for Crohn's disease". Gastroenterology 133 (5): 1487–98. November 2007. doi:10.1053/j.gastro.2007.08.004. PMID 17919633. http://download.journals.elsevierhealth.com/pdfs/journals/0016-5085/PIIS0016508507014503.pdf.
- ↑ "Debate on the lack of evidence of Mycobacterium avium subsp. paratuberculosis in Crohn's disease". Inflammatory Bowel Diseases 11 (12): 1123. December 2005. doi:10.1097/01.MIB.0000191609.20713.ea. PMID 16306778.
- ↑ "Mycobacterium avium subspecies paratuberculosis causes Crohn's disease in some inflammatory bowel disease patients". World Journal of Gastroenterology 20 (23): 7403–15. June 2014. doi:10.3748/wjg.v20.i23.7403. PMID 24966610.
- ↑ "New insights into Crohn's Disease". http://www.liv.ac.uk/researchintelligence/issue33/crohns.htm.
- ↑ "NOD2 and ATG16L1 polymorphisms affect monocyte responses in Crohn's disease". World Journal of Gastroenterology 17 (23): 2829–37. June 2011. doi:10.3748/wjg.v17.i23.2829. PMID 21734790.
- ↑ "Molecular evidence for Mycobacterium avium subspecies paratuberculosis (MAP) in Crohn's disease correlates with enhanced TNF-alpha secretion". Digestive and Liver Disease 39 (5): 445–51. May 2007. doi:10.1016/j.dld.2006.12.006. PMID 17317344.
- ↑ "Involvement of mycobacterium avium subspecies paratuberculosis in TNF-α production from macrophage: possible link between MAP and immune response in Crohn's disease". Inflammatory Bowel Diseases 17 (11): E140–2. November 2011. doi:10.1002/ibd.21750. PMID 21990211.
- ↑ 113.0 113.1 "Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn's disease involving the ileum". The ISME Journal 1 (5): 403–18. September 2007. doi:10.1038/ismej.2007.52. PMID 18043660. Bibcode: 2007ISMEJ...1..403B.
- ↑ "Invasive Escherichia coli are a feature of Crohn's disease". Laboratory Investigation; A Journal of Technical Methods and Pathology 87 (10): 1042–54. October 2007. doi:10.1038/labinvest.3700661. PMID 17660846.
- ↑ "High prevalence of adherent-invasive Escherichia coli associated with ileal mucosa in Crohn's disease". Gastroenterology 127 (2): 412–21. August 2004. doi:10.1053/j.gastro.2004.04.061. PMID 15300573.
- ↑ "Crohn's disease-associated adherent-invasive Escherichia coli adhesion is enhanced by exposure to the ubiquitous dietary polysaccharide maltodextrin". PLOS ONE 7 (12): e52132. 2012. doi:10.1371/journal.pone.0052132. PMID 23251695. Bibcode: 2012PLoSO...752132N.
- ↑ "Biofilm formation as a novel phenotypic feature of adherent-invasive Escherichia coli (AIEC)". BMC Microbiology 9 (1): 202. September 2009. doi:10.1186/1471-2180-9-202. PMID 19772580.
- ↑ "Subversion of autophagy in adherent invasive Escherichia coli-infected neutrophils induces inflammation and cell death". PLOS ONE 7 (12): e51727. 2012. doi:10.1371/journal.pone.0051727. PMID 23272151. Bibcode: 2012PLoSO...751727C.
- ↑ "Inflammation drives dysbiosis and bacterial invasion in murine models of ileal Crohn's disease". PLOS ONE 7 (7): e41594. 2012. doi:10.1371/journal.pone.0041594. PMID 22848538. Bibcode: 2012PLoSO...741594C.
- ↑ "Adherent-invasive Escherichia coli and Crohn's disease". Current Opinion in Gastroenterology 23 (1): 16–20. January 2007. doi:10.1097/MOG.0b013e3280105a38. PMID 17133079.
- ↑ "Role for protease activity in visceral pain in irritable bowel syndrome". The Journal of Clinical Investigation 117 (3): 636–47. March 2007. doi:10.1172/JCI29255. PMID 17304351.
- ↑ "Induction of intestinal inflammation in mouse by activation of proteinase-activated receptor-2". The American Journal of Pathology 161 (5): 1903–15. November 2002. doi:10.1016/S0002-9440(10)64466-5. PMID 12414536.
- ↑ "Oh my aching gut: irritable bowel syndrome, Blastocystis, and asymptomatic infection". Parasites & Vectors 1 (1): 40. October 2008. doi:10.1186/1756-3305-1-40. PMID 18937874.
- ↑ "Crohn's disease: the cold chain hypothesis". Lancet 362 (9400): 2012–5. December 2003. doi:10.1016/S0140-6736(03)15024-6. PMID 14683664.
- ↑ "Fridges blamed for Crohn's disease rise". Medical News Today. December 12, 2003. http://www.medicalnewstoday.com/articles/4849.php.
- ↑ "Crohn's disease: the cold chain hypothesis". International Journal of Colorectal Disease 21 (5): 399–401. July 2006. doi:10.1007/s00384-005-0003-7. PMID 16059694.
- ↑ "Inflammation and gastrointestinal Candida colonization". Current Opinion in Microbiology 14 (4): 386–91. August 2011. doi:10.1016/j.mib.2011.07.015. PMID 21802979.
- ↑ "Possible links between Crohn's disease and Paratuberculosis". European Commission Directorate-General Health & Consumer Protection. http://ec.europa.eu/food/fs/sc/scah/out38_en.pdf.
- ↑ "Two-year-outcomes analysis of Crohn's disease treated with rifabutin and macrolide antibiotics". The Journal of Antimicrobial Chemotherapy 39 (3): 393–400. March 1997. doi:10.1093/jac/39.3.393. PMID 9096189.
- ↑ 130.0 130.1 "Epidemiologic analysis of Crohn disease in Japan: increased dietary intake of n-6 polyunsaturated fatty acids and animal protein relates to the increased incidence of Crohn disease in Japan". The American Journal of Clinical Nutrition 63 (5): 741–5. May 1996. doi:10.1093/ajcn/63.5.741. PMID 8615358.
- ↑ "Evidence for an increased risk of Crohn's disease in oral contraceptive users". Gastroenterology 89 (5): 1046–9. November 1985. doi:10.1016/0016-5085(85)90207-0. PMID 4043662.
- ↑ "Possible association between isotretinoin and inflammatory bowel disease". The American Journal of Gastroenterology 101 (7): 1569–73. July 2006. doi:10.1111/j.1572-0241.2006.00632.x. PMID 16863562.
- ↑ "[Isotretinoin and ulcerous colitis]" (in es). Anales del Sistema Sanitario de Navarra 27 (2): 241–3. 2004. doi:10.4321/S1137-66272004000300009. PMID 15381956.
- ↑ "Isotretinoin-induced inflammatory bowel disease in an adolescent". The Annals of Pharmacotherapy 35 (10): 1214–6. October 2001. doi:10.1345/aph.10368. PMID 11675849. http://www.theannals.com/cgi/pmidlookup?view=long&pmid=11675849. Retrieved November 1, 2010.
- ↑ Segerstrom, Suzanne C.; Miller, Gregory E. (July 2004). "Psychological Stress and the Human Immune System: A Meta-Analytic Study of 30 Years of Inquiry". Psychological Bulletin 130 (4): 601–630. doi:10.1037/0033-2909.130.4.601. ISSN 0033-2909. PMID 15250815.
- ↑ "Dietary sources of inorganic microparticles and their intake in healthy subjects and patients with Crohn's disease". The British Journal of Nutrition 92 (6): 947–55. December 2004. doi:10.1079/bjn20041276. PMID 15613257.
- ↑ "Dietary microparticles and their impact on tolerance and immune responsiveness of the gastrointestinal tract". The British Journal of Nutrition 98 (Suppl 1): S59–63. October 2007. doi:10.1017/S0007114507832922. PMID 17922962.
- ↑ "Association of doxycycline use with the development of gastroenteritis, irritable bowel syndrome and inflammatory bowel disease in Australians deployed abroad". Internal Medicine Journal 43 (8): 919–26. August 2013. doi:10.1111/imj.12179. PMID 23656210.
- ↑ 139.0 139.1 "Potential association between the oral tetracycline class of antimicrobials used to treat acne and inflammatory bowel disease". The American Journal of Gastroenterology 105 (12): 2610–6. December 2010. doi:10.1038/ajg.2010.303. PMID 20700115.
- ↑ "Impact of Long-Term Antibiotic Use for Acne on Bacterial Ecology and Health Outcomes: A Review of Observational Studies". Current Dermatology Reports 1 (1): 23–28. March 2012. doi:10.1007/s13671-011-0001-7.
- ↑ Crawford JM. "The Gastrointestinal tract, Chapter 17". In Cotran RS, Kumar V, Robbins SL. Robbins Pathologic Basis of Disease: 5th Edition. W.B. Saunders and Company, Philadelphia, 1994.
- ↑ "Host genes related to paneth cells and xenobiotic metabolism are associated with shifts in human ileum-associated microbial composition". PLOS ONE 7 (6): e30044. June 13, 2012. doi:10.1371/journal.pone.0030044. PMID 22719822. Bibcode: 2012PLoSO...730044Z.
- ↑ HCP: Pill Cam, Capsule Endoscopy, Esophageal Endoscopy
- ↑ "Crohn's disease and lichen nitidus: a case report and comparison of common histopathologic features". Inflammatory Bowel Diseases 7 (4): 314–8. November 2001. doi:10.1097/00054725-200111000-00006. PMID 11720321.
- ↑ "Diffuse jejunoileitis of Crohn's disease". Gut 34 (10): 1374–8. October 1993. doi:10.1136/gut.34.10.1374. PMID 8244104.
- ↑ 146.0 146.1 "A simple classification of Crohn's disease: report of the Working Party for the World Congresses of Gastroenterology, Vienna 1998". Inflammatory Bowel Diseases 6 (1): 8–15. February 2000. doi:10.1002/ibd.3780060103. PMID 10701144.
- ↑ "Treatment of Crohn's Disease of Inflammatory, Stenotic, and Fistulizing Phenotypes". Current Treatment Options in Gastroenterology 6 (3): 183–200. June 2003. doi:10.1007/s11938-003-0001-1. PMID 12744819.
- ↑ 148.0 148.1 "Crohn disease of the small bowel: preliminary comparison among CT enterography, capsule endoscopy, small-bowel follow-through, and ileoscopy". Radiology 238 (1): 128–34. January 2006. doi:10.1148/radiol.2381050296. PMID 16373764.
- ↑ "A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn's disease". The American Journal of Gastroenterology 101 (5): 954–64. May 2006. doi:10.1111/j.1572-0241.2006.00506.x. PMID 16696781.
- ↑ "The small bowel enema: a ten year review". Clinical Radiology 47 (1): 46–8. January 1993. doi:10.1016/S0009-9260(05)81213-9. PMID 8428417.
- ↑ "Radiographic imaging of inflammatory bowel disease". Gastroenterology Clinics of North America 31 (1): 93–117, ix. March 2002. doi:10.1016/S0889-8553(01)00007-3. PMID 12122746.
- ↑ "Multislice CT enteroclysis: technique and clinical applications". Clinical Radiology 61 (1): 31–9. January 2006. doi:10.1016/j.crad.2005.08.006. PMID 16356814.
- ↑ "Computed tomographic findings of abdominal complications of Crohn's disease--pictorial essay". Canadian Association of Radiologists Journal 56 (1): 25–35. February 2005. PMID 15835588. https://www.proquest.com/openview/d36a211b9091938911c873b3ed55d0dc/1. Retrieved May 18, 2022.
- ↑ "New diagnostic imaging tools for inflammatory bowel disease". Gut 55 (5): 733–41. May 2006. doi:10.1136/gut.2005.076612. PMID 16609136.
- ↑ "Utility of high-resolution MR imaging in demonstrating transmural pathologic changes in Crohn disease". Radiographics 29 (6): 1847–67. October 2009. doi:10.1148/rg.296095503. PMID 19959525.
- ↑ "Diffusion-weighted MR imaging of the gastrointestinal tract: technique, indications, and imaging findings". Radiographics 33 (3): 655–76; discussion 676–80. May 2013. doi:10.1148/rg.333125042. PMID 23674768.
- ↑ "Review article: nutrition and adult inflammatory bowel disease". Alimentary Pharmacology & Therapeutics 17 (3): 307–20. February 2003. doi:10.1046/j.1365-2036.2003.01482.x. PMID 12562443.
- ↑ "Diagnostic value of C-reactive protein for predicting activity level of Crohn's disease". Clinical Gastroenterology and Hepatology 4 (7): 882–7. July 2006. doi:10.1016/j.cgh.2006.02.003. PMID 16630759.
- ↑ "The anti-Saccharomyces cerevisiae antibody assay in a province-wide practice: accurate in identifying cases of Crohn's disease and predicting inflammatory disease". Canadian Journal of Gastroenterology 19 (12): 717–21. December 2005. doi:10.1155/2005/147681. PMID 16341311.
- ↑ "Anti-Saccharomyces cerevisiae and antineutrophil cytoplasmic antibodies as predictors of inflammatory bowel disease". Gut 54 (9): 1232–6. September 2005. doi:10.1136/gut.2004.060228. PMID 16099791.
- ↑ "New serological markers in inflammatory bowel disease are associated with complicated disease behaviour". Gut 56 (10): 1394–403. October 2007. doi:10.1136/gut.2006.108043. PMID 17456509.
- ↑ "New serological markers for inflammatory bowel disease are associated with earlier age at onset, complicated disease behavior, risk for surgery, and NOD2/CARD15 genotype in a Hungarian IBD cohort". The American Journal of Gastroenterology 103 (3): 665–81. March 2008. doi:10.1111/j.1572-0241.2007.01652.x. PMID 18047543.
- ↑ "Novel anti-glycan antibodies related to inflammatory bowel disease diagnosis and phenotype". The American Journal of Gastroenterology 104 (6): 1426–34. June 2009. doi:10.1038/ajg.2009.79. PMID 19491856.
- ↑ "Serologic markers in inflammatory bowel disease: tools for better diagnosis and disease stratification". Expert Review of Gastroenterology & Hepatology 1 (2): 265–74. December 2007. doi:10.1586/17474124.1.2.265. PMID 19072419.
- ↑ 165.0 165.1 "Association Between Inflammatory Bowel Disease and Vitamin D Deficiency: A Systematic Review and Meta-analysis". Inflammatory Bowel Diseases 21 (11): 2708–17. November 2015. doi:10.1097/MIB.0000000000000546. PMID 26348447.
- ↑ "Systematic review: the use of serology to exclude or diagnose coeliac disease (a comparison of the endomysial and tissue transglutaminase antibody tests)". Alimentary Pharmacology & Therapeutics 24 (1): 47–54. July 2006. doi:10.1111/j.1365-2036.2006.02967.x. PMID 16803602. "Both the endomysial antibody and tissue transglutaminase antibody have very high sensitivities (93% for both) and specificities (>99% and >98% respectively) for the diagnosis of typical coeliac disease with villous atrophy. (...) As the detection of at least partial villous atrophy was used to make a diagnosis of coeliac disease in the vast majority of studies, we can't assume that the same LRs apply to coeliac patients with lesser abnormality such as an increase in intraepithelial lymphocytes or electron-microscopic changes only. In fact, if such lesser abnormalities were used as criteria for diagnosing (and excluding) coeliac disease, the sensitivity of the tests could be lower (i.e. more false negatives), especially since a number of studies suggest that the EMA and tTG antibody tests are less sensitive with lesser degrees of mucosal abnormality".
- ↑ "[Celiac disease"] (in es). Medicina Clinica 131 (7): 264–70. September 2008. doi:10.1016/S0025-7753(08)72247-4. PMID 18775218. http://www.elsevier.es/es-revista-medicina-clinica-2-articulo-enfermedad-celiaca-13125306. Retrieved March 13, 2016. "Estos marcadores presentan en general una elevada sensibilidad y especificidad (cercanas al 90%) en presencia de atrofia marcada de las vellosidades intestinales. Sin embargo, muestran una notable disminución de la sensibilidad (del orden del 40-50%) en casos con atrofia vellositaria leve o cambios mínimos. These markers generally have high sensitivity and specificity (around 90%) in the presence of marked atrophy of the villi. However, they show a marked decrease in sensitivity (of the order of 40-50%) in cases with mild villous atrophy or minimal changes.".
- ↑ "Subclinical celiac disease and gluten sensitivity". Gastroenterology and Hepatology from Bed to Bench 4 (3): 102–8. 2011. PMID 24834166.
- ↑ "Gluten tolerance; potential challenges in treatment strategies". Gastroenterology and Hepatology from Bed to Bench 4 (2): 53–7. 2011. PMID 24834157.
- ↑ 170.0 170.1 170.2 "Crohn's Disease: 54 Tips to Help You Manage". May 16, 2007. http://www.webmd.com/digestive-disorders/features/crohns-disease-54-tips-to-help-you-manage.
- ↑ Roncoroni L, Gori R, Elli L, Tontini GE, Doneda L, Norsa L, Cuomo M, Lombardo V, Scricciolo A, Caprioli F, Costantino A, Scaramella L, Vecchi M. Nutrition in Patients with Inflammatory Bowel Diseases: A Narrative Review. Nutrients. 2022 Feb 10;14(4):751
- ↑ Ananthakrishnan AN, Kaplan GG, Bernstein CN, Burke KE, Lochhead PJ, Sasson AN, Agrawal M, Tiong JHT, Steinberg J, Kruis W, Steinwurz F, Ahuja V, Ng SC, Rubin DT, Colombel JF, Gearry R; International Organization for Study of Inflammatory Bowel Diseases. Lifestyle, behaviour, and environmental modification for the management of patients with inflammatory bowel diseases: an International Organization for Study of Inflammatory Bowel Diseases consensus. Lancet Gastroenterol Hepatol. 2022 Apr 26:S2468-1253(22)00021-8.
- ↑ "Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature". The American Journal of Gastroenterology 106 (4): 563–73. April 2011. doi:10.1038/ajg.2011.44. PMID 21468064.
- ↑ Nutrition and Diagnosis-Related Care, 7th edition. Baltimore, MD: Lippincott Williams & Wilkins. 2008. pp. 1020 (pp 431). ISBN 978-1-60831-017-3.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedHanauerCrohns - ↑ "Crohn's disease". Lancet 359 (9300): 62–9. January 2002. doi:10.1016/S0140-6736(02)07284-7. PMID 11809204.
- ↑ "Therapeutic role of methotrexate in pediatric Crohn's disease". Bosnian Journal of Basic Medical Sciences 18 (3): 211–216. August 2018. doi:10.17305/bjbms.2018.2792. PMID 29338679.
- ↑ "FDA Approves Cimzia to Treat Crohn's Disease" (Press release). Food and Drug Administration (FDA). April 22, 2008. Archived from the original on October 20, 2009. Retrieved November 5, 2009.
- ↑ "Prescribing information ustekinumab". https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125261s147lbl.pdf.
- ↑ "Natalizumab induction and maintenance therapy for Crohn's disease". The New England Journal of Medicine 353 (18): 1912–25. November 2005. doi:10.1056/NEJMoa043335. PMID 16267322.
- ↑ "Natalizumab for induction of remission in Crohn's disease". The Cochrane Database of Systematic Reviews 2018 (8): CD006097. August 2018. doi:10.1002/14651858.CD006097.pub3. PMID 30068022.
- ↑ "Discover RINVOQ® (upadacitinib)" (in en). https://www.rinvoq.com/.
- ↑ Oxford Handbook of Clinical Medicine (7th ed.). Oxford University Press. 2007. pp. 266–7. ISBN 978-0-19-856837-7.
- ↑ 184.0 184.1 184.2 "Anti-IL-12/23p40 antibodies for induction of remission in Crohn's disease". The Cochrane Database of Systematic Reviews 2016 (11): CD007572. November 2016. doi:10.1002/14651858.CD007572.pub3. PMID 27885650.
- ↑ "Guidelines for the management of inflammatory bowel disease in adults". Gut 60 (5): 571–607. May 2011. doi:10.1136/gut.2010.224154. PMID 21464096.
- ↑ "Guidelines for the management of iron deficiency anaemia". Gut 60 (10): 1309–16. October 2011. doi:10.1136/gut.2010.228874. PMID 21561874.
- ↑ "Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases". Inflammatory Bowel Diseases 13 (12): 1545–53. December 2007. doi:10.1002/ibd.20285. PMID 17985376.
- ↑ Beaugerie, L.; Itzkowitz, S.H. Cancers complicating inflammatory bowel disease. N. Engl. J. Med. 2015, 372, 1441–1452
- ↑ Toruner, M.; Loftus, E.V.; Harmsen, W.S.; Zinsmeister, A.R.; Orenstein, R.; Sandborn, W.J.; Colombel, J.; Egan, L.J. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology 2008, 134, 929–936
- ↑ Farraye, F.A.; Melmed, G.Y.; Lichtenstein, G.R.; Kane, S.V. ACG Clinical Guideline: Preventive Care in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2017, 112, 241–258.
- ↑ Kucharzik, T.; Ellul, P.; Greuter, T.; Rahier, J.F.; Verstockt, B.; Abreu, C.; Albuquerque, A.; Allocca, M.; Esteve, M.; Farraye, F.A.; et al. ECCO Guidelines on the Prevention, Diagnosis, and Management of Infections in Inflammatory Bowel Disease. J. Crohn’s Colitis 2021, 15, 879–913.
- ↑ Ananthakrishnan, A.N.; McGinley, E.L. Infection-related hospitalizations are associated with increased mortality in patients with inflammatory bowel diseases. J. Crohn’s Colitis 2013, 7, 107–112.
- ↑ Malhi, G.; Rumman, A.; Thanabalan, R.; Croitoru, K.; Silverberg, M.S.; Steinhart, A.H.; Nguyen, G.C. Vaccination in inflammatory bowel disease patients: Attitudes, knowledge, and uptake. J. Crohn’s Colitis 2015, 9, 439–444.
- ↑ Costantino, A.; Michelon, M.; Noviello, D.; Macaluso, F.S.; Leone, S.; Bonaccorso, N.; Costantino, C.; Vecchi, M.; Caprioli, F., on behalf of AMICI Scientific Board. Attitudes towards Vaccinations in a National Italian Cohort of Patients with Inflammatory Bowel Disease. Vaccines 2023, 11, 1591.
- ↑ "Surgical recurrence in Crohn's disease: Are we getting better?". World Journal of Gastroenterology 21 (20): 6097–100. May 2015. doi:10.3748/wjg.v21.i20.6097. PMID 26034346.
- ↑ "Resection Surgery for Crohn's Disease". About.com. January 12, 2007. http://ibdcrohns.about.com/od/surgeryprocedures/a/resectioncrohns.htm.
- ↑ "Reoperative rates for Crohn's disease following strictureplasty. Long-term analysis". Diseases of the Colon and Rectum 39 (11): 1199–203. November 1996. doi:10.1007/BF02055108. PMID 8918424.
- ↑ "Predictability of the postoperative course of Crohn's disease". Gastroenterology 99 (4): 956–63. October 1990. doi:10.1016/0016-5085(90)90613-6. PMID 2394349.
- ↑ "The impact of early endoscopic lesions on the clinical course of patients following ileocolonic resection for Crohn's disease: A 5-year prospective cohort study". United European Gastroenterology Journal 1 (4): 294–8. August 2013. doi:10.1177/2050640613495197. PMID 24917974.
- ↑ "Short Bowel Syndrome". July 2015. https://www.niddk.nih.gov/health-information/digestive-diseases/short-bowel-syndrome.
- ↑ "Intestinal transplant for Crohn's disease". Everyday Health. October 24, 2006. http://www.revolutionhealth.com/conditions/digestive/crohns-disease/surgery/intestinal-transplant.
- ↑ "The syndrome of ileal disease and the broken enterohepatic circulation: cholerheic enteropathy". Gastroenterology 52 (4): 752–7. April 1967. doi:10.1016/S0016-5085(67)80140-9. PMID 5337211.
- ↑ Limketkai, Berkeley N; Akobeng, Anthony K; Gordon, Morris; Adepoju, Akinlolu Adedayo (2020-07-17). Cochrane Gut Group. ed. "Probiotics for induction of remission in Crohn's disease" (in en). Cochrane Database of Systematic Reviews 2020 (7): CD006634. doi:10.1002/14651858.CD006634.pub3. PMID 32678465.
- ↑ 204.0 204.1 "Inflammatory bowel disease". Child and Adolescent Psychiatric Clinics of North America 19 (2): 301–18, ix. April 2010. doi:10.1016/j.chc.2010.01.007. PMID 20478501. http://gut.bmj.com/cgi/content/short/39/Suppl_1/A15. Retrieved September 4, 2018.
- ↑ "Psychological Interventions for Irritable Bowel Syndrome and Inflammatory Bowel Diseases". Clinical and Translational Gastroenterology 8 (1): e214. January 2017. doi:10.1038/ctg.2016.69. PMID 28102860.
- ↑ 206.0 206.1 "European evidence based consensus on the diagnosis and management of Crohn's disease: special situations". Gut 55 (Suppl 1): i36–58. March 2006. doi:10.1136/gut.2005.081950c. PMID 16481630. "the colitis activity index fell significantly in the treatment group compared to the sham acupuncture group. However, recruitment did not reach its target and the number of patients was small.".
- ↑ "Acupuncture and moxibustion in the treatment of active Crohn's disease: a randomized controlled study". Digestion 69 (3): 131–9. 2004. doi:10.1159/000078151. PMID 15114043.
- ↑ "Review on efficacy and health services research studies of complementary and alternative medicine in inflammatory bowel disease". Chinese Journal of Integrative Medicine 17 (6): 403–9. June 2011. doi:10.1007/s11655-011-0758-3. PMID 21660673.
- ↑ "Homeopathy is Unscientific and Unethical". Bioethics 26 (9): 508–512. 2012. doi:10.1111/j.1467-8519.2011.01956.x. https://zenodo.org/record/1035885. Retrieved October 28, 2017.
- ↑ "Towards a Demarcation of Science from Pseudoscience". Philosophy of Pseudoscience: Reconsidering the Demarcation Problem. University of Chicago Press. 2013. pp. 45–59. ISBN 978-0-226-05182-6. https://books.google.com/books?id=Pc4OAAAAQBAJ&pg=PA45. "Yet homeopathy is a paradigmatic example of pseudoscience. It is neither simply bad science nor science fraud, but rather profoundly departs from scientific method and theories while being described as scientific by some of its adherents (often sincerely)."
- ↑ "Science, Pseudoscience, and Not Science: How do They Differ?". Healthcare and Biomedical Technology in the 21st Century. 2014. pp. 19–57. doi:10.1007/978-1-4614-8541-4_2. ISBN 978-1-4614-8540-7. https://books.google.com/books?id=7RIJAgAAQBAJ&pg=PA19. "within the traditional medical community it is considered to be quackery"
- ↑ "A systematic review of systematic reviews of homeopathy". British Journal of Clinical Pharmacology 54 (6): 577–82. December 2002. doi:10.1046/j.1365-2125.2002.01699.x. PMID 12492603.
- ↑ "Are the clinical effects of homoeopathy placebo effects? Comparative study of placebo-controlled trials of homoeopathy and allopathy". Lancet 366 (9487): 726–32. 2005. doi:10.1016/S0140-6736(05)67177-2. PMID 16125589.
- ↑ "Evidence Check 2: Homeopathy - Science and Technology Committee". British House of Commons Science and Technology Committee. February 22, 2010. https://publications.parliament.uk/pa/cm200910/cmselect/cmsctech/45/4504.htm.
- ↑ "Cannabis for inflammatory bowel disease". Digestive Diseases 32 (4): 468–74. 2014. doi:10.1159/000358155. PMID 24969296.
- ↑ "Cannabis for the treatment of Crohn's disease". The Cochrane Database of Systematic Reviews 11 (11): CD012853. November 2018. doi:10.1002/14651858.CD012853.pub2. PMID 30407616.
- ↑ "Crohn's disease - Prognosis". University of Maryland Medical Centre. http://www.umm.edu/patiented/articles/who_gets_crohns_disease_000103_5.htm.
- ↑ 219.0 219.1 "Epidemiology of inflammatory bowel disease in a defined northern California population". The Western Journal of Medicine 149 (5): 541–6. November 1988. PMID 3250100.
- ↑ "Incidence of Crohn's disease in four counties in southeastern Norway, 1990-93. A prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists". Scandinavian Journal of Gastroenterology 31 (4): 355–61. April 1996. doi:10.3109/00365529609006410. PMID 8726303.
- ↑ "Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD)". Gut 39 (5): 690–7. November 1996. doi:10.1136/gut.39.5.690. PMID 9014768.
- ↑ "Familial empirical risks for inflammatory bowel disease: differences between Jews and non-Jews". Gut 34 (4): 517–24. April 1993. doi:10.1136/gut.34.4.517. PMID 8491401.
- ↑ "Effects of light smoking consumption on the clinical course of Crohn's disease". Inflammatory Bowel Diseases 15 (5): 734–41. May 2009. doi:10.1002/ibd.20828. PMID 19067428.
- ↑ "Crohn's disease manifests differently in boys and girls". Crohn's and Colitis Foundation of America. http://www.ccfa.org/reuters/ibdboysgirls.
- ↑ "Who is affected by Crohn's disease". Healthwise. http://www.webmd.com/hw-popup/who-is-affected-by-crohns-disease.
- ↑ "The genetics of inflammatory bowel disease". Gut 40 (5): 572–4. May 1997. doi:10.1136/gut.40.5.572. PMID 9203931.
- ↑ "Ulcerative colitis and Crohn's disease in an unselected population of monozygotic and dizygotic twins. A study of heritability and the influence of smoking". Gut 29 (7): 990–6. July 1988. doi:10.1136/gut.29.7.990. PMID 3396969.
- ↑ "The burden of inflammatory bowel disease in Europe". Journal of Crohn's & Colitis 7 (4): 322–37. May 2013. doi:10.1016/j.crohns.2013.01.010. PMID 23395397.
- ↑ 229.0 229.1 "Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies". Lancet 390 (10114): 2769–2778. December 2018. doi:10.1016/S0140-6736(17)32448-0. PMID 29050646.
- ↑ "Historical aspects of inflammatory bowel disease". Journal of Clinical Gastroenterology 10 (3): 286–97. June 1988. doi:10.1097/00004836-198806000-00012. PMID 2980764.
- ↑ "Antoni Lésniowski and his contribution to regional enteritis (Crohn's disease)". Journal of the Royal Society of Medicine 81 (8): 468–70. August 1988. doi:10.1177/014107688808100817. PMID 3047387.
Further reading
- "ACG Clinical Guideline: Management of Crohn's Disease in Adults". Am. J. Gastroenterol. 113 (4): 481–517. April 2018. doi:10.1038/ajg.2018.27. PMID 29610508.
External links
- "Crohn's disease". MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/crohnsdisease.html.
| Classification | |
|---|---|
| External resources |
 |


