Medicine:P wave (electrocardiography)
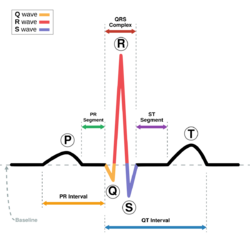
The P wave on the ECG represents atrial depolarization, which results in atrial contraction, or atrial systole.
Physiology
The P wave is a summation wave generated by the depolarization front as it transits the atria. Normally the right atrium depolarizes slightly earlier than left atrium since the depolarization wave originates in the sinoatrial node, in the high right atrium and then travels to and through the left atrium. The depolarization front is carried through the atria along semi-specialized conduction pathways including Bachmann's bundle resulting in uniform shaped waves. Depolarization originating elsewhere in the atria (atrial ectopics) result in P waves with a different morphology from normal.
Pathology
Peaked P waves (> 0.25 mV) suggest right atrial enlargement, cor pulmonale, (P pulmonale rhythm),[1] but have a low predictive value (~20%).[2]
A P wave with increased amplitude can indicate hypokalemia.[3] It can also indicate right atrial enlargement.[4]
A P wave with decreased amplitude can indicate hyperkalemia.[5]
Bifid P waves (known as P mitrale) indicate left-atrial abnormality - e.g. dilatation [6] or hypertrophy.[1]
If at least three different shaped P waves can be seen in a given ECG lead tracing, this implies that even if one of them arises from the SA node, at least two others are arising elsewhere. This is taken as evidence of multiple (i.e. at least two) ectopic foci, and is called multifocal (or more correctly, multiform) atrial rhythm if the rate is ≤100) or multifocal atrial tachycardia if the rate is over 100.[7] This appears particularly commonly in exacerbations of chronic obstructive lung disease.[8]
If the baseline has a totally irregular form, this suggests fibrillatory waves of atrial fibrillation or possibly artefact; a saw tooth shaped baseline suggests the flutter waves of atrial flutter. With either of these rhythms, if the ventricular rate is fast, the fibrillatory or flutter waves can easily be misinterpreted as P waves.
Absence of the P wave with a flat baseline may indicate:
- Fine atrial fibrillation[1]
- Sinoatrial arrest (with a secondary escape rhythm)
If P waves are not clearly delineated in the surface ECG, a Lewis lead may be used to better visualize P waves.
Atrial repolarization
This occurs a mean of 320 ms after the end of the P wave, with a duration of 2-3 times that of the P wave and a polarity always opposite to that of the P wave. It is represented on the surface ECG by a so-called Ta wave. The clinical relevance of this is that, although a normal phenomenon, the nadir of the Ta wave can occur just after the QRS complex and cause ST depression similar to (and easily mistaken with) that occurring with disease states such as cardiac ischaemia.[9]
Related pages
References
- ↑ 1.0 1.1 1.2 Longmore, Murray (2004). Oxford Handbook of Clinical Medicine 8th edition page 90. Oxford University Press. ISBN 978-0-19-852558-5.
- ↑ "Two-dimensional echocardiographic assessment of electrocardiographic criteria for right atrial enlargement.". Circulation 64 (2): 387–391. 1981. doi:10.1161/01.CIR.64.2.387. PMID 6454512.
- ↑ "Hypokalaemia". http://lifeinthefastlane.com/ecg-library/basics/hypokalaemia/.
- ↑ Yanowitz, Frank G.. "VII. Atrial Enlargement". http://library.med.utah.edu/kw/ecg/ecg_outline/Lesson7/index.html.
- ↑ Levis, Joel T (2013). "ECG Diagnosis: Hyperkalemia". The Permanente Journal 17 (1): 69. doi:10.7812/TPP/12-088. ISSN 1552-5767. PMID 23596374.
- ↑ "Sensitivity and specificity of commonly used electrocardiographic criteria for left atrial enlargement determined by m-mode echocardiography". Am J Cardiol 53 (6): 829–832. 1983. doi:10.1016/0002-9149(84)90413-2. PMID 6230922.
- ↑ Kastor JA (1990). "Multifocal Atrial Tachycardia". N Engl J Med 322 (24): 1713–1717. doi:10.1056/NEJM199006143222405. PMID 2188131.
- ↑ "Evidence supporting a new rate threshold for multifocal atrial tachycardia". Clin Cardiol 28 (12): 3561–3563. 2006. doi:10.1002/clc.4960281205. PMID 16405199.
- ↑ Smith, SW. "Atrial Repolarization Wave Mimicking ST Depression". http://hqmeded-ecg.blogspot.co.uk/2011/11/atrial-repolarization-wave-mimicking-st.html.
 |




