Medicine:Open aortic surgery
| Open aortic surgery | |
|---|---|
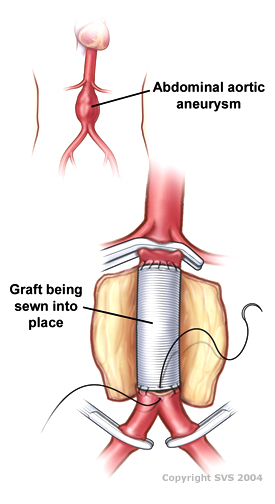 Drawing of an open infrarenal aortic aneurysm repair using a tube graft | |
| Other names | Open aortic repair |
| Specialty | Vascular Surgery |
Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.[1]
Depending on the extent of the aorta repaired, an open aortic operation may be called an Infrarenal aortic repair, a Thoracic aortic repair, or a Thoracoabdominal aortic repair. A thoracoabdominal aortic repair is a more extensive operation than either an isolated infrarenal or thoracic aortic repair.
OAS is distinct from aortic valve repair and aortic valve replacement, as OAS describes surgery of the aorta, rather than of the heart valves. When the aortic valve is diseased in addition to the ascending aorta, the Bentall procedure is used to treat the entire aortic root. An axillary-bifemoral bypass is another type of vascular bypass used to treat aortic pathology, however it is not true open aortic surgery as it reconstructs the flow of blood to the legs from the arm, rather than in the native location of the aorta.
Medical uses
Open aortic surgery (OAS) is used to treat patients with aortic aneurysms greater than 5.5 cm in diameter, to treat aortic rupture of an aneurysm any size, to treat aortic dissections, and to treat acute aortic syndrome. It is used to treat infrarenal aneurysms, as well as juxta- and pararenal aneurysm, thoracic and thoracoabdominal aneurysms, and also non-aneurysmal aortic pathology. Disease of the aorta proximal to the left subclavian artery in the chest lies within the specialty of cardiac surgery, and is treated via procedures such as the valve-sparing aortic root replacement.
Prior to the advent of endovascular aneurysm repair (EVAR), OAS was the only surgical treatment available for aortic aneurysms. It is still preferred at some institutions and by some patients as it may be more durable than EVAR,[2] and does not require post-operative surveillance CT scans.
OAS is sometimes required for patients who have previously undergone EVAR but need further treatment, such as for degeneration of the EVAR seal zones leading to continued aneurysm growth. OAS is also sometimes required in cases of EVAR graft infection where the stent graft is removed to treat the infection.[3]
Open repair versus endovascular repair
The shift away from open aortic surgery towards endovascular surgery since 2003 has been driven by worse perioperative mortality associated with OAS, particularly in patients in relatively frail health.[4] Unlike endovascular repair, there are no strict anatomic contra-indications to open repair; Rather, open repair is viewed as the fall back option for patients with unfavorable anatomy for endovascular repair.[5] The main drawback of open repair is the larger physiologic demand of the operation, which is associated with increased rates of short term mortality in most studies.[6]
Patients younger than 50 years with descending and thoracoabdominal aortic aneurysm have low surgical risks, and open repairs can be performed with excellent short-term and durable long-term results. Open surgical repairs should be considered initially in younger patients requiring descending and thoracoabdominal aortic aneurysm repairs. Heritable thoracic aortic disease (HTAD) warrants closer postoperative surveillance.[7]
Technique
Open surgery typically involves exposure of the dilated portion of the aorta and insertion of a synthetic (Dacron or Gore-Tex) graft (tube). Once the graft is sewn into the proximal (toward the patient's head) and distal (toward the patient's foot) portions of the aorta, the aneurysmal sac is closed around the graft. Alternatively, the anastomosis can be carried out with expandable devices, a simpler and quicker procedure [8][9]
The aorta and its branching arteries are cross-clamped during open surgery. This can lead to inadequate blood supply to the spinal cord, resulting in paraplegia, when repairing thoracic aneurysms. A 2004 systematic review and meta analysis found that cerebrospinal fluid drainage (CFSD), when performed in experienced centers, reduces the risk of ischemic spinal cord injury by increasing the perfusion pressure to the spinal cord.[10] A 2012 Cochrane systematic review noted that further research regarding the effectiveness of CFSD for preventing a spinal cord injury is required.[11]
Approach
The infrarenal aorta can be approached via a transabdominal midline or paramedian incision, or via a retroperitoneal approach.
The paravisceral and thoracic aorta are approached via a left-sided posteriolateral thoracotomy incision in approximately the 9th intercostal space.[12] For a thoracoabdominal aortic aneurysm, this approach can be extended to a median or paramedian abdominal incision to allow access to the iliac arteries.
Sequential aortic clamping
At medical centers with a high volume of open aortic surgery, the fastest option for open aortic surgery was sequential aortic clamping or "clamp-and-sew", whereby the aorta was clamped proximally and distally to the diseased segment, and a graft sewn into the intervening segment.[13] This technique leaves the branches of the aorta un-perfused during the time it takes to sew in the graft, potentially increasing the risk of ischemia to the organs which derive their arterial supply from the clamped segment. Critics of this technique advocate intra-operative aortic perfusion.[14] In infrarenal aneurysms, the relative tolerance of the lower extremities to ischemia allows surgeons to clamp distally with low risk of ill effect.
Techniques to limit ischemia
A number of techniques exist for maintaining perfusion to the viscera and spinal cord during open thoracoabdominal aortic aneurysm repair, including left heart bypass, balloon perfusion catheter placement in the visceral arteries, selective spinal drainage and cold crystalloid renal perfusion.[15] There is limited evidence supporting these techniques.[16]
Graft configuration
The abdominal aorta is anastomosed preferentially to the main limb of a tube or bifurcated graft in an end-to-end fashion to minimize turbulent flow at the proximal anastomosis. If normal aorta exists superior to the iliac bifurcation, a tube graft can be sewn distally to that normal aorta. If the distal aorta is diseased, a bifurcated graft can be used in an aorto-billiac or aorto-bifemoral configuration. If visceral vessels are involved in the diseased aortic segment, a branched graft can be used with branches sewn directly to visceral vessels, or the visceral vessels can be separately revascularized.[citation needed]
Reimplantation of the inferior mesenteric artery
Because of collateral blood flow from the superior mesenteric artery (SMA) via the marginal artery, the inferior mesenteric artery usually does not have to be reimplanted into the aortic graft when performing an open abdominal aortic aneurysm repair.
Risks and complications
OAS is widely recognized as having higher rates of perioperative morbidity and mortality than endovascular procedures for comparable segments of the aorta. For example, in infrarenal aneurysms, perioperative mortality with endovascular surgery is approximately 0.5%, against 3% with open repair.[17]
Besides the risk of death, other risks and complications with OAS depend on the segment of aorta involved, and may include renal failure, spinal cord ischemia leading to paralysis, buttock claudication, ischemic colitis, embolization leading to acute limb ischemia, infection, and bleeding.[18] Development of spinal cord injury is associated with increased perioperative mortality after the complex aortic repair.[19]
Aortic graft infections occur in 1-5% of aortic prosthetic placements. It can result in limb amputation, pseudo-aneurysm formation, septic emboli, aorto-enteric fistulae, septic shock and death. The most frequently involved pathogens are Staphylococcus aureus, and coagulase-negative staphylococci, followed by Enterobacterales and uncommon bacteria. In case of gut involvement also fungi may play a role. For patients unable to undergo major surgery, the outcome of conservative approach remains uncertain but usually provides for life-long suppressive antibiotic therapy. In selected cases an attempt of stopping antibiotic treatment after 3-6 months can be done.[20]
Recovery after OAS
Recovery time after OAS is substantial. Immediately following surgery, patients can expect to spend 1–3 days in the intensive care unit, followed by 4–10 days on the hospital ward. After discharge, patients will take 3–6 months to fully recover their energy and return to their pre-operative daily activities.[citation needed] However, enhanced recovery after surgery (ERAS) protocols can improve recovery following surgery.[21]
TAAA repair requires a very large incision that cuts through muscles and bones making recovery very difficult and painful for the patient. Intraoperative intercostal nerve cryoanalgesia has been used during procedure to help reduce pain after TAAA.[22]
History
The history of aortic surgery dates back to Greek surgeon Antyllus, who first performed surgeries for various aneurysms in the second century AD. Many advancements of OAS have been developed in the past century.
In 1955, cardiovascular surgeons, Drs. Michael DeBakey and Denton Cooley performed the first replacement of a thoracic aneurysm with a homograft. In 1958, they began using the Dacron graft, resulting in a revolution for surgeons in the surgical repair of aortic aneurysms.[23] DeBakey was first to perform cardiopulmonary bypass to repair the ascending aorta, using antegrade perfusion of the brachiocephalic artery.
By the mid-1960s, at Baylor College of Medicine, DeBakey’s group began performing surgery on thoracoabdominal aortic aneurysms (TAAA), which presented formidable surgical challenges, often fraught with serious complications, such as paraplegia, paraparesis and renal failure. DeBakey protégé and vascular Surgeon, E. Stanley Crawford, in particular, began dedicating most of his time to TAAAs. In 1986, he classified TAAA open surgery cases into four types:[24] Extent I, extending from the left subclavian artery to just below the renal artery; Extent II, from the left subclavian to below the renal artery; Extent III, from the sixth intercostal space to below the renal artery; and Extent IV, from the twelfth intercostal space to the iliac bifurcation (i.e. total abdominal).
In 1992, another classification, Extent V, characterized by Hazim J. Safi, MD, identified aneurysmal disease extending from the sixth intercostal space to above the renal arteries. Safi's group used experimental animal models for a prospective study on the use distal aortic perfusion, cerebrospinal fluid drainage, moderate hypothermia and sequential clamping to decrease in the incidence of neurological deficit. In 1994, they presented their experiences, showing that the incidence for Extent I and II dropped from 25% to 5%.[25] This marked a new era for protecting the spinal cord, brain, kidneys, heart and lungs during OAS on TAAA.
Progress and future challenges
Postoperative paraplegia and paraparesis have been the scourge of thoracoabdominal aortic repair since the inception of the procedure.[26] However, with evolving surgical strategies, identification of predictors, and use of various adjuncts over the years, the incidence of spinal cord injury after thoracic/thoracoabdominal aortic repair has declined. Embracing a multimodality approach offers a good insight into combating this grave complication[27]
See also
References
- ↑ "Impact of hospital market competition on endovascular aneurysm repair adoption and outcomes.". J. Vasc. Surg. 58 (3): 596–606. September 2013. doi:10.1016/j.jvs.2013.02.014. PMID 23684424.
- ↑ "Long-term durability of open abdominal aortic aneurysm repair.". J. Vasc. Surg. 46 (4): 669–75. October 2007. doi:10.1016/j.jvs.2007.05.046. PMID 17903647.
- ↑ Chaufour, Xavier; Gaudric, Julien; Goueffic, Yann; Khodja, Réda Hassen; Feugier, Patrick; Malikov, Sergei; Beraud, Guillaume; Ricco, Jean-Baptiste (February 2017). For the AURC (French University Surgeons Association) collaborators. "A multicenter experience with infected abdominal aortic endograft explantation.". Journal of Vascular Surgery 65 (2): 372–380. doi:10.1016/j.jvs.2016.07.126. PMID 27720319.
- ↑ "Long-term comparison of endovascular and open repair of abdominal aortic aneurysm.". N. Engl. J. Med. 367 (21): 1988–97. November 2012. doi:10.1056/NEJMoa1207481. PMID 23171095.
- ↑ "Endovascular repair of abdominal aortic aneurysm.". Cochrane Database Syst Rev 1 (1): CD004178. 2014. doi:10.1002/14651858.CD004178.pub2. PMID 24453068. PMC 10749584. https://semanticscholar.org/paper/40160cfe152e8e35ce6d54c4799a8d677caa5d3e.
- ↑ Antoniou, GA; Antoniou, SA; Torella, F (March 2020). "Editor's Choice - Endovascular vs. Open Repair for Abdominal Aortic Aneurysm: Systematic Review and Meta-analysis of Updated Peri-operative and Long Term Data of Randomised Controlled Trials.". European Journal of Vascular and Endovascular Surgery 59 (3): 385–397. doi:10.1016/j.ejvs.2019.11.030. PMID 31899100.
- ↑ Tanaka, Akiko; Leonard, Samuel D.; Sandhu, Harleen K.; Afifi, Rana O.; Miller, Charles C.; Charlton-Ouw, Kristofer M.; Ray, Amberly; Hassan, Madiha et al. (September 2019). "Open Descending and Thoracoabdominal Aortic Repairs in Patients Younger Than 50 Years Old". The Annals of Thoracic Surgery 108 (3): 693–699. doi:10.1016/j.athoracsur.2019.03.058. ISSN 1552-6259. PMID 31009630.
- ↑ "Improved Device for Sutureless Aortic Anastomosis: Applied in a Case of Cancer". Tex. Heart Inst. J. 29 (1): 56–9. 2002. PMID 11995854.
- ↑ "Descending aorta substitution with expandable ends prosthesis. Case report". J Cardiovasc Surg (Torino) 40 (3): 417–20. June 1999. PMID 10412932.
- ↑ Cinà, C.; Abouzahr, L.; Arena, G.; Laganà, A.; Devereaux, P.; Farrokhyar, F. (2004). "Cerebrospinal fluid drainage to prevent paraplegia during thoracic and thoracoabdominal aortic aneurysm surgery: a systematic review and meta-analysis". Journal of Vascular Surgery 40 (1): 36–44. doi:10.1016/j.jvs.2004.03.017. PMID 15218460.
- ↑ Khan, Shaukat Nawaz; Stansby, Gerard (2012-10-17). "Cerebrospinal fluid drainage for thoracic and thoracoabdominal aortic aneurysm surgery". The Cochrane Database of Systematic Reviews 10 (10): CD003635. doi:10.1002/14651858.CD003635.pub3. ISSN 1469-493X. PMID 23076900.
- ↑ Coselli, Joseph (2008). "Tips for successful outcomes for descending thoracic and thoracoabdominal aortic aneurysm procedures.". Semin Vasc Surg 21 (1): 13–20. doi:10.1053/j.semvascsurg.2007.11.009. PMID 18342730.
- ↑ "Descending thoracic aortic aneurysm repair: 12-year experience using distal aortic perfusion and cerebrospinal fluid drainage.". Ann. Thorac. Surg. 80 (4): 1290–6; discussion 1296. October 2005. doi:10.1016/j.athoracsur.2005.02.021. PMID 16181856.
- ↑ "Descending thoracic aortic aneurysm repair: 12-year experience using distal aortic perfusion and cerebrospinal fluid drainage.". Ann. Thorac. Surg. 80 (4): 1290–6; discussion 1296. October 2005. doi:10.1016/j.athoracsur.2005.02.021. PMID 16181856.
- ↑ Coselli, Joseph (2008). "Tips for successful outcomes for descending thoracic and thoracoabdominal aortic aneurysm procedures.". Semin Vasc Surg 21 (1): 13–20. doi:10.1053/j.semvascsurg.2007.11.009. PMID 18342730.
- ↑ Hsu, CC; Kwan, GN; van Driel, ML; Rophael, JA (14 March 2012). "Distal aortic perfusion during thoracoabdominal aneurysm repair for prevention of paraplegia.". The Cochrane Database of Systematic Reviews 3 (3): CD008197. doi:10.1002/14651858.CD008197.pub2. PMID 22419329. https://espace.library.uq.edu.au/view/UQ:273694/UQ273694_OA.pdf.
- ↑ Schermerhorn, Marc (2008). "Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population.". N Engl J Med 358 (5): 464–74. doi:10.1056/NEJMoa0707348. PMID 18234751.
- ↑ Crawford, E. S.; Crawford, J. L.; Safi, H. J.; Coselli, J. S.; Hess, K. R.; Brooks, B.; Norton, H. J.; Glaeser, D. H. (March 1986). "Thoracoabdominal aortic aneurysms: preoperative and intraoperative factors determining immediate and long-term results of operations in 605 patients". Journal of Vascular Surgery 3 (3): 389–404. doi:10.1016/0741-5214(86)90101-1. ISSN 0741-5214. PMID 3951025.
- ↑ Sef, D; Thet, MS; Miskolczi, S; Velissaris, T; De Silva, R; Luthra, S; Turina, MI (1 June 2023). "Perioperative neuromonitoring during thoracoabdominal aortic aneurysm open repair: a systematic review.". European Journal of Cardio-Thoracic Surgery 63 (6). doi:10.1093/ejcts/ezad221. PMID 37233116.
- ↑ Antonello, Roberta Maria; D'Oria, Mario; Cavallaro, Marco; Dore, Franca; Cova, Maria Assunta; Ricciardi, Maria Chiara; Comar, Manola; Campisciano, Giuseppina et al. (2019). "Management of abdominal aortic prosthetic graft and endograft infections. A multidisciplinary update" (in en). Journal of Infection and Chemotherapy 25 (9): 669–680. doi:10.1016/j.jiac.2019.05.013. https://linkinghub.elsevier.com/retrieve/pii/S1341321X1930145X.
- ↑ Melnyk, M; Casey, RG; Black, P; Koupparis, AJ (October 2011). "Enhanced recovery after surgery (ERAS) protocols: Time to change practice?". Canadian Urological Association 5 (5): 342–8. doi:10.5489/cuaj.11002. PMID 22031616.
- ↑ Tanaka, Akiko; Al-Rstum, Zain; Leonard, Samuel D.; Gardiner, Bri’Ana D.; Yazij, Ibrahim; Sandhu, Harleen K.; Miller, Charles C.; Safi, Hazim J. et al. (January 2020). "Intraoperative Intercostal Nerve Cryoanalgesia Improves Pain Control After Descending and Thoracoabdominal Aortic Aneurysm Repairs" (in en). The Annals of Thoracic Surgery 109 (1): 249–254. doi:10.1016/j.athoracsur.2019.07.083. PMID 31521592.
- ↑ De Bakey, M. E.; Cooley, D. A. (1953-06-20). "Successful resection of aneurysm of thoracic aorta and replacement by graft". Journal of the American Medical Association 152 (8): 673–676. doi:10.1001/jama.1953.03690080017005. ISSN 0002-9955. PMID 13044606. https://www.ncbi.nlm.nih.gov/pubmed/13044606.
- ↑ Crawford, E. S. (May 1974). "Thoraco-abdominal and abdominal aortic aneurysms involving renal, superior mesenteric, celiac arteries". Annals of Surgery 179 (5): 763–772. doi:10.1097/00000658-197405000-00032. ISSN 0003-4932. PMID 4274686.
- ↑ Safi, H. J.; Miller, C. C. (June 1999). "Spinal cord protection in descending thoracic and thoracoabdominal aortic repair". The Annals of Thoracic Surgery 67 (6): 1937–1939; discussion 1953–1958. doi:10.1016/s0003-4975(99)00397-5. ISSN 0003-4975. PMID 10391343.
- ↑ Safi, Hazim J.; Estrera, Anthony L.; Azizzadeh, Ali; Coogan, Sheila; Miller, Charles C. (March 2008). "Progress and future challenges in thoracoabdominal aortic aneurysm management". World Journal of Surgery 32 (3): 355–360. doi:10.1007/s00268-007-9256-3. ISSN 0364-2313. PMID 17952499. https://pubmed.ncbi.nlm.nih.gov/17952499/.
- ↑ Panthee, Nirmal; Ono, Minoru (February 2015). "Spinal cord injury following thoracic and thoracoabdominal aortic repairs". Asian Cardiovascular & Thoracic Annals 23 (2): 235–246. doi:10.1177/0218492314548901. ISSN 1816-5370. PMID 25178467. https://pubmed.ncbi.nlm.nih.gov/25178467/.
 |





