Medicine:MDMA-assisted psychotherapy
| Part of a series on |
| Psychology |
|---|
 |
|
|
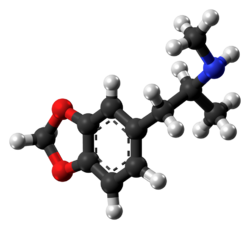
MDMA-assisted psychotherapy is the use of prescribed doses of MDMA as an adjunct to psychotherapy sessions. Research suggests that MDMA-assisted psychotherapy for post-traumatic stress disorder (PTSD), including Complex PTSD, might improve treatment effectiveness.[1][2][3] In 2017, a Phase II clinical trial led to "breakthrough therapy" designation by the US Food and Drug Administration (FDA) for potential use as a treatment for PTSD.[4][5]
MDMA-assisted psychotherapy is currently under investigation as a treatment for various other mental health disorders, inclusing Major Depressive Disorder, social anxiety in autistic individuals, alcohol use disorder, and mood disturbances in individuals facing life-threatening illnesses.[6][7][8] The research is controversial[9][10] in part because recreational MDMA use has been associated with harmful effects among some users.[11][9][12]
Therapeutic effects
Post-traumatic stress disorder (PTSD) is most commonly treated by cognitive behavioral therapy (particularly prolonged exposure and cognitive processing therapy), eye movement desensitization and reprocessing, and psychodynamic psychotherapy. However, over half of these patients continue to have PTSD after completing therapy, with results from military PTSD being especially poor.[13]
PTSD is best treated when a patient is in the 'optimal arousal zone'. This is the zone in which emotions are engaged yet not overwhelming. In this zone, four symptom clusters of PTSD are sedated:[10] These are:
- re-experiencing
- avoidance
- negative alterations in cognition/mood
- alterations in arousal and reactivity
Subjects with PTSD exhibit extreme emotional numbing or anxiety and struggle to remain in the optimal arousal zone during conservative therapies. Threatening interpretations of memories are reinforced when patients are in low emotional states.[14] If traumatic memories are revisited in therapy when a patient is not within the optimal arousal state, therapy for PTSD can actually increase the patient's trauma.[14]
When used in therapy, MDMA has been reported to increase empathy, closeness between patient and therapist, relaxation, motivation to engage with therapy and introspective thought, and reduce depression and anxiety. MDMA makes it easier for a patient to stay in the optimal arousal zone by decreasing feelings of anxiety and defensiveness when revisiting traumatic memories.[10] By increasing feelings of closeness and empathy, it can improve the patient's trust in the therapist and encourage introspective thought to reassess memories and actions. Furthermore, research suggests that treatment may improve the quality of sleep of individuals affected by PTSD-related sleep disturbances.[15] It is believed that these factors may increase the success rate of psychotherapy.
Adverse effects, which can last from a few hours to several days, include diminished appetite, anxiety, headache, jaw tightness, tinnitus, nausea, asthenia, fatigue, acute sinusitis, nasopharyngitis, upper respiratory tract infection, disturbance in attention, tremor, tics, dysuria, erythema, and depression.[16]
Research
With FDA approval granted in 2017, MDMA has been authorized for use in research related to psychotherapy.[4] MDMA-assisted psychotherapy is currently under investigation as a potential treatment for various mental health disorders, encompassing PTSD, Major Depressive Disorder, social anxiety in autistic individuals,[6] alcohol use disorder,[7] and mood disturbances in individuals facing life-threatening illnesses.[8] A large proportion of this research has been focused on PTSD and Major Depressive Disorder.
PTSD
A phase 3 study indicated that MDMA-assisted therapy represents a potential breakthrough treatment for severe PTSD that merits expedited clinical evaluation.[17] Based on this study, MDMA-assisted psychotherapy was granted breakthrough therapy designation by the FDA, a designation that indicates that there is preliminary evidence that an intervention might offer a substantial improvement over other options for a serious health condition.[5]However, given the lack of blinding, several researchers have postulated that the results of the phase 3 trial might be heavily influenced by expectancy effects.[18][19] There are no trials comparing MDMA-assisted psychotherapy to already existing first-line psychological treatments for PTSD which seems to attain similar or elevated symptom reduction compared with that due to MDMA-assisted psychotherapy based on indirect evidence.[20]
Major Depressive Disorder
There have been several studies that investigated MDMA-assisted psychotherapy as a potential treatment for Major Depressive Disorder (MDD). A analysis of six phase 2 trials showed a trend toward significance, while a phase 3 trial reported that MDMA-assisted psychotherapy had antidepressant effects. Given that unprocessed trauma is considered a causative factor in some individuals with depression, it has been proposed that the benefit observed in PTSD trials might be applicable to MDD as well. [21]
Neuroscience & mechanism of action
PTSD inhibits a subject's ability to respond appropriately to trauma-related stimuli.[10] The current model of PTSD proposes that it results from amplified and uncontrolled responses from the amygdala to trauma-specific cues.[14] Oxytocin, which is increased by MDMA, has been found to increase trust and emotional awareness and reduce amygdala responses as well as reduce coupling of the amygdala to brainstem regions associated with autonomic and behavioral characteristics of fear.[22][23][24] It has been proposed that these effects foster memory reconsolidation by allowing the patient to access the traumatic memory while feeling detached from the sense of imminent threat.[14]
History
MDMA was first synthesized by the German pharmaceutical company Merck KGaA in 1912 as an intermediate in the synthesis of a potential blood clotting medication. Its psychoactive effects were not noted until the early 1960s. In the 1960s and 1970s, the drug was used in psychotherapy, although it was not an approved drug, and no clinical trials had been performed. Alexander Shuglin, an American chemist, synthesized MDMA in order to investigate its properties and was responsible for introducing the compound to a small number of American psychiatrists in the early 1970s. Shuglin and another chemist, David E. Nichols, are credited with publishing the first report regarding the effects and pharmacology of MDMA in humans.[25]
Psychotherapists using MDMA for therapeutic purposes initially desired to keep its use within the clinical research community; however, the medication gained popularity in the club scene in the early 1980s. This eventually lead to the drug being classified as a Schedule One substance by the US Drug Enforcement Administration (DEA) in 1986. The scheduling of MDMA made it illegal to manufacture, possess, or distribute, essentially ending the practice of MDMA-assisted psychotherapy in the US. Despite this, MDMA continued to be used recreationally in the club and rave scene.[25]
Switzerland continued to study the drug for use in individual, couple, and group therapies until 1993, when the Swiss Ministry of Health withdrew permission to use MDMA and LSD by psychiatrists due to concerns about a lack of research methodology. Over 100 patients in Switzerland with a variety of mental illnesses were treated with MDMA-assisted psychotherapy during this time frame.[26]
Legality
In 1986, MDMA was classed as a Schedule One drug by the United Nations according to its Convention on Psychotropic Substances of 1971 due to increasing rates of non-clinical use and police seizures, along with its high potential for abuse.[10][25] MDMA has remained a Schedule One substance since 1986, and most research was stopped at that time. In response to this, researchers interested in MDMA for use in psychotherapy founded and funded the US-based non-profit research organization, Multidisciplinary Association for Psychedelic Studies (MAPS).[25] MAPS is now one of the leading organizations funding research on psychedelic and controlled substances.
Current legal status
The US Food and Drug Administration (FDA) and Drug Enforcement Administration (DEA) granted approval for researching MDMA's efficacy as an adjunct to psychotherapy in 2004, and the first trial was carried out in 2011.[10][27] In 2023, MAPS announced that it is compiling data from 18 different phase 2 and phase 3 studies with plans to file a New Drug Application with the FDA. MAPS hopes to receive FDA approval by the end of 2024.[27]
In July 2023, Australia became the first country to approve the legal use of MDMA-assisted psychotherapy for the treatment of depression and PTSD.[28]
Controversy & safety
MDMA's effects vary across people and settings and include adverse outcomes.[9][12] The drug causes neurotransmitter activation across the main neural pathways (including serotonin and dopamine, noradrenaline) that can result in large mood swings. The memories that emerge under the influence of MDMA can evoke unwanted emotions.[9] Side effects of MDMA use by recreational users include appetite fluctuations, food cravings, and disordered eating.[9]
Once the effects of MDMA wear off, there is a "period of neurochemical depletion" that invokes anhedonia, lethargy, anger, depression, irritability, brooding, greater everyday stress, altered pain thresholds, changes in sleep, and bad dreams, especially in female participants.[9] The symptoms are thought to be due to the depletion of serotonin, as a result of the large release of serotonin triggered by MDMA and have been called "neurotoxic in terms of causing serotonergic dysfunction."[9]
There are also concerns surrounding "drug-dependent learning" — the theory that patients will return to the drug to access the state they were in when on the drug in therapy.[9]
There were 92 MDMA-related deaths in England and Wales in 2018, up from 56 the year before,[29] and 10,000 hospitalizations for MDMA-related illness/injury in 2011 in the US.[11] However, as of 2021, there have been no such cases reported for clinical settings.
Media reports and statements of academic authors have often transmitted the view of MDMA as a possible medicine or treatment rather than as an adjunct to psychotherapy.[10] This has been considered dangerous because it could lead people to believe that MDMA is an effective treatment alone, without concomitant psychotherapy.[10]
See also
- Alexander Shulgin
- Breakthrough therapy
- Convention on Psychotropic Substances
- Improving Access to Psychological Therapies
- List of Psychotherapies
- MDMA
- Post-traumatic stress disorder
- Psychedelic therapy
References
- ↑ "Efficacy of 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy for posttraumatic stress disorder: A systematic review and meta-analysis". Progress in Neuro-Psychopharmacology & Biological Psychiatry 96: 109735. January 2020. doi:10.1016/j.pnpbp.2019.109735. PMID 31437480.
- ↑ "MDMA-Assisted Psychotherapy for Treatment of Posttraumatic Stress Disorder: A Systematic Review With Meta-Analysis". Journal of Clinical Pharmacology 62 (4): 463–471. October 2021. doi:10.1002/jcph.1995. PMID 34708874.
- ↑ "A comparison of MDMA-assisted psychotherapy to non-assisted psychotherapy in treatment-resistant PTSD: A systematic review and meta-analysis". Journal of Psychopharmacology 35 (5): 501–511. May 2021. doi:10.1177/0269881120965915. PMID 33345689.
- ↑ 4.0 4.1 "(±)-MDMA and its enantiomers: potential therapeutic advantages of R(-)-MDMA". Psychopharmacology 235 (2): 377–392. February 2018. doi:10.1007/s00213-017-4812-5. PMID 29248945.
- ↑ 5.0 5.1 "FDA Designates MDMA As 'Breakthrough Therapy' For Post-Traumatic Stress" (in en). https://www.forbes.com/sites/janetwburns/2017/08/28/fda-designates-mdma-as-breakthrough-therapy-for-post-traumatic-stress/.
- ↑ 6.0 6.1 Danforth, Alicia L.; Grob, Charles S.; Struble, Christopher; Feduccia, Allison A.; Walker, Nick; Jerome, Lisa; Yazar-Klosinski, Berra; Emerson, Amy (2018-09-08). "Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: a randomized, double-blind, placebo-controlled pilot study". Psychopharmacology 235 (11): 3137–3148. doi:10.1007/s00213-018-5010-9. ISSN 0033-3158. PMID 30196397.
- ↑ 7.0 7.1 Sessa, Ben; Higbed, Laurie; O’Brien, Steve; Durant, Claire; Sakal, Chloe; Titheradge, Daniel; Williams, Tim M; Rose-Morris, Anna et al. (April 2021). "First study of safety and tolerability of 3,4-methylenedioxymethamphetamine-assisted psychotherapy in patients with alcohol use disorder" (in en). Journal of Psychopharmacology 35 (4): 375–383. doi:10.1177/0269881121991792. ISSN 0269-8811. PMID 33601929. http://journals.sagepub.com/doi/10.1177/0269881121991792.
- ↑ 8.0 8.1 Wolfson, Philip E.; Andries, Julane; Feduccia, Allison A.; Jerome, Lisa; Wang, Julie B.; Williams, Emily; Carlin, Shannon C.; Sola, Evan et al. (2020-11-24). "MDMA-assisted psychotherapy for treatment of anxiety and other psychological distress related to life-threatening illnesses: a randomized pilot study" (in en). Scientific Reports 10 (1): 20442. doi:10.1038/s41598-020-75706-1. ISSN 2045-2322. PMID 33235285. Bibcode: 2020NatSR..1020442W.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 "The potential dangers of using MDMA for psychotherapy". Journal of Psychoactive Drugs 46 (1): 37–43. 2014. doi:10.1080/02791072.2014.873690. PMID 24830184.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 "MDMA-assisted psychotherapy for people diagnosed with treatment-resistant PTSD: what it is and what it isn't". Annals of General Psychiatry 19: 33. 2020. doi:10.1186/s12991-020-00283-6. PMID 32435270.
- ↑ 11.0 11.1 "'My therapist gave me a pill': can MDMA help cure trauma?" (in en-GB). The Guardian. 2016-09-16. ISSN 0261-3077. https://www.theguardian.com/society/2016/sep/16/mdma-ptsd-therapy-trauma-maps-medical-study.
- ↑ 12.0 12.1 "The dark side of ecstasy: neuropsychiatric symptoms after exposure to 3,4-methylenedioxymethamphetamine". Basic & Clinical Pharmacology & Toxicology 102 (1): 15–24. January 2008. doi:10.1111/j.1742-7843.2007.00159.x. PMID 18047478.
- ↑ Straud, Casey L.; Siev, Jedidiah; Messer, Stephen; Zalta, Alyson K. (Oct 2019). "Examining military population and trauma type as moderators of treatment outcome for first-line psychotherapies for PTSD: A meta-analysis". Journal of Anxiety Disorders 67: 102133. doi:10.1016/j.janxdis.2019.102133. ISSN 1873-7897. PMID 31472332.
- ↑ 14.0 14.1 14.2 14.3 "Current Perspective on MDMA-Assisted Psychotherapy for Posttraumatic Stress Disorder". Journal of Contemporary Psychotherapy 48 (2): 99–108. 2018. doi:10.1007/s10879-017-9379-2. PMID 29720767.
- ↑ Ponte, Linnae; Jerome, Lisa; Hamilton, Scott; Mithoefer, Michael C.; Yazar-Klosinski, Berra B.; Vermetten, Eric; Feduccia, Allison A. (August 2021). "Sleep Quality Improvements After MDMA-Assisted Psychotherapy for the Treatment of Posttraumatic Stress Disorder" (in en). Journal of Traumatic Stress 34 (4): 851–863. doi:10.1002/jts.22696. ISSN 0894-9867. PMID 34114250.
- ↑ "The Efficacy of MDMA (3,4-Methylenedioxymethamphetamine) for Post-traumatic Stress Disorder in Humans: A Systematic Review and Meta-Analysis". Cureus 13 (5): e15070. May 2021. doi:10.7759/cureus.15070. PMID 34150406.
- ↑ "MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study". Nature Medicine 27 (6): 1025–1033. June 2021. doi:10.1038/s41591-021-01336-3. PMID 33972795.
- ↑ "Caution at psychiatry's psychedelic frontier". Nature Medicine 27 (10): 1687–1688. October 2021. doi:10.1038/s41591-021-01524-1. PMID 34635858.
- ↑ "Blinding and expectancy confounds in psychedelic randomized controlled trials". Expert Review of Clinical Pharmacology 14 (9): 1133–1152. September 2021. doi:10.1080/17512433.2021.1933434. ISSN 1751-2433. PMID 34038314.
- ↑ "Challenges with benchmarking of MDMA-assisted psychotherapy". Nature Medicine 27 (10): 1689–1690. October 2021. doi:10.1038/s41591-021-01525-0. PMID 34635857. https://hal.archives-ouvertes.fr/hal-03414583/file/Halvorsen%20et%20al%20-%202021%20-%20Challenges%20with%20benchmarking%20of%20MDMA-assisted%20psychotherapy.pdf.
- ↑ Kvam, Tor-Morten; Goksøyr, Ivar W.; Stewart, Lowan H.; Repantis, Dimitris; Røssberg, Jan Ivar; Andreassen, Ole A. (2022). "Study protocol for "MDMA-assisted therapy as a treatment for major depressive disorder: A proof of principle study"". Frontiers in Psychiatry 13: 954388. doi:10.3389/fpsyt.2022.954388. ISSN 1664-0640. PMID 36386973.
- ↑ "Oxytocin modulates neural circuitry for social cognition and fear in humans". The Journal of Neuroscience 25 (49): 11489–11493. December 2005. doi:10.1523/JNEUROSCI.3984-05.2005. PMID 16339042.
- ↑ "The prosocial effects of 3,4-methylenedioxymethamphetamine (MDMA): Controlled studies in humans and laboratory animals". Neuroscience and Biobehavioral Reviews 57: 433–446. October 2015. doi:10.1016/j.neubiorev.2015.08.016. PMID 26408071.
- ↑ "Prefrontal-amygdala circuits in social decision-making". Nature Neuroscience 24 (1): 5–18. January 2021. doi:10.1038/s41593-020-00738-9. PMID 33169032.
- ↑ 25.0 25.1 25.2 25.3 "A Review of 3,4-methylenedioxymethamphetamine (MDMA)-Assisted Psychotherapy" (in English). Frontiers in Psychiatry 10: 138. 2019. doi:10.3389/fpsyt.2019.00138. PMID 30949077.
- ↑ "A Review of 3,4-methylenedioxymethamphetamine (MDMA)-Assisted Psychotherapy" (in English). Frontiers in Psychiatry 10: 138. 2019. doi:10.3389/fpsyt.2019.00138. PMID 30949077.
- ↑ 27.0 27.1 Colliver, Victoria (2023-09-18). "MDMA's Latest Trial Results Offer Hope for Patients with PTSD | UC San Francisco" (in en). https://www.ucsf.edu/news/2023/09/426116/mdmas-latest-trial-results-offer-hope-for-patients-ptsd.
- ↑ Carpenter, David E.. "Australia The First Nation To Approve The Legal Use Of MDMA And Psilocybin" (in en). https://www.forbes.com/sites/davidcarpenter/2023/02/06/australia-the-first-nation-to-approve-the-legal-use-of-mdma-and-psilocybin/.
- ↑ "Ecstasy 'too child-friendly' as deaths rise to record levels" (in en-GB). BBC News. 2019-08-15. https://www.bbc.co.uk/news/newsbeat-49357157.
External links
- MDMA Facts and Statistics National Institute on Drug Abuse
- Methylenedioxymethamphetamine (MDMA or 'Ecstasy') drug profile European Monitoring Centre for Drugs and Drug Addiction
- MDMA-Assisted Psychotherapy Multidisciplinary Association for Psychedelic Studies
- Dead Dog on the Left Documentary about MDMA-assisted treatment for military PTSD
- Is MDMA psychiatry's antibiotic? Tedx Talk by Ben Sessa.
- MDMA, Psychotherapy, and the Future of PTSD Treatment TEDx talk by Brad Burge
 |