Medicine:Erythema marginatum
| Erythema marginatum | |
|---|---|
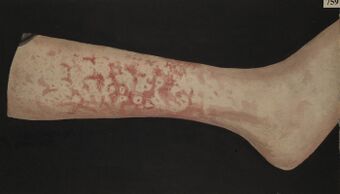 | |
| Painting of a leg with erythema marginatum |
Erythema marginatum (also known as chicken wire erythema)[1] is an acquired skin condition which primarily affects the arms, trunk, and legs.[2] It is a type of erythema (redness of the skin or mucous membranes) characterised by bright pink or red circular lesions which have sharply-defined borders and faint central clearing. The lesions typically range between 3-10cm in size, and are distributed symmetrically over the torso and inner surfaces of the limbs and extensor surfaces.[3] The lesions last between one and four weeks but have been known to be present on patients for as long as several months.[4]
The condition was first reported in 1816 by Dr. Jean Cruveilhier and is thought to be linked to other skin conditions such as urticaria and systemic lupus erythematosus.
An association with bradykinin has been proposed in the case of hereditary angioedema.[5]
Presentation
The rings are barely raised and are non-itchy. The face is generally spared.[citation needed]
The condition is characterised by circular, non-pruritic, erythematous rashes which form on the trunk and extremities of the body. The rash has a known serpiginous edge, and often appears and disappears spontaneously over time.[6] Histological examination of the rash identifies infiltration of mononuclear cells and neutrophils in the papillary and upper half of the reticular dermis layer.[7]
Associated conditions
It occurs in less than 10% of patients with acute rheumatic fever (ARF),[8] but is considered a major Jones criterion when it does occur.[9][10] The four other major criteria include carditis, polyarthritis, Sydenham's chorea, and subcutaneous nodules. In this case, it is often associated with Group A streptococcal infection, otherwise known as Streptococcus pyogenes infection, which can be detected with an ASO titer.[citation needed]
It is an early feature of acute rheumatic fever though not pathognomonic of it.[11] It some cases it may be associated with mild myocarditis (inflammation of heart muscle).
The condition is also seen as a precursor to or accompany an attack of angioedema,[1] and is seen in conditions like allergic drug reactions, sepsis and glomerulonephritis.[11]
It often occurs as a harbinger of attacks in hereditary angioedema. In this case it may occur several hours or up to a day before an attack.[citation needed]
Diagnosis
Types
Some sources distinguish between the following:[citation needed]
- "Erythema marginatum rheumaticum"
- "Erythema marginatum perstans"
The diagnosis of erythema marginatum can be made during examination of skin appearance. A skin biopsy may be performed if needed, to confirm the diagnosis. Medical history and family history may also be taken into account.
Treatment
Erythema marginatum can be treated with hydrocortisone and adrenocorticotropc hormone (ACTH).[12]
In cases where the condition is associated with ARF and severe carditis, corticosteroids are indicated[13] alongside the classic treatment protocol for ARF which is a 10-day course of oral Penicillin. Alternatively, one dosage of Penicillin G benzathine may be injected intramuscularly followed with a daily course of oral Amoxicillin for a total of 10 days. In cases of Penicillin allergy, a Cephalosporin or Macrolide may be considered. To avoid recurrences of ARF, secondary prevention is called for. This may include a period of antibiotic prophylaxis deteremined by the presence of carditis and the amount of remaining heart damage.[14]
References
- ↑ 1.0 1.1 Bygum, Anette; Broesby-Olsen, Sigurd (March 2011). "Rapid resolution of erythema marginatum after icatibant in acquired angioedema". Acta dermato-venereologica 91 (2): 185–186. doi:10.2340/00015555-1055. ISSN 1651-2057.
- ↑ Hinzey, E (June 2023). Arredondo M. ed. "Erythema Marginatum". Patient Education Reference Center (PERC).
- ↑ "erythema marginatum" at Dorland's Medical Dictionary
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. pp. 281. ISBN 978-1-4160-2999-1.
- ↑ "Erythema marginatum and hereditary angioedema". South. Med. J. 97 (10): 948–50. October 2004. doi:10.1097/01.SMJ.0000140850.22535.FA. PMID 15558919.
- ↑ Kliegman, R.M.; Stanton, B.F; Gerne, J.W.; Schor, N.F.; Behrman, R.E. (2011). Group A streptococcus. In: Nelson textbook of pediatrics (9 ed.). Elsevier Saunders.
- ↑ Vijayan, Vini; Sukumaran, Sukesh (July 2023). "Erythema Marginatum". The Journal of Pediatrics 258: 113330. doi:10.1016/j.jpeds.2022.12.038. ISSN 0022-3476.
- ↑ Sharma, Shreya; Biswal, Niranjan (December 2015). "Erythema Marginatum". Indian Pediatrics 52 (12): 1100. ISSN 0974-7559.
- ↑ Tani, L.T.; Veasy, L.G.; Minich, L.L.A.; Shaddy, R.E. (2003). "Rheumatic fever in children younger than 5 years: is the presentation different?". Pediatrics 112: 1065-8.
- ↑ Wolfson, Allan B.; Hendey, Gregory W.; Ling, Louis J.; Rosen, Carlo L.; Schaider, Jeffrey J; Sharieff, Ghazala Q. (2012). Harwood-Nuss' Clinical Practice of Emergency Medicine. Wolters Kluwer Health. pp. 1302. ISBN 9781451153453.
- ↑ 11.0 11.1 Erythema Marginatum Pictorial CME
- ↑ Burke, J. B. (1955-08-01). "Erythema Marginatum" (in en). Archives of Disease in Childhood 30 (152): 359–365. doi:10.1136/adc.30.152.359. ISSN 0003-9888. PMID 13249623.
- ↑ Oski, Frank, A., ed (2004). Oski's Essential Pediatrics. Lippincott Williams & Wilkins. pp. 298. ISBN 9780781737708.
- ↑ Kimberlin, David W., ed (2021). Group A Streptococcal Infections. In: Red Book: 2021-2024 Report of the Committee on Infectious Diseases (32 ed.). American Academy of Pediatrics. pp. 694-707. ISBN 978-1-61002-521-8.
External links
| Classification |
|---|
 |

