N of 1 trial
An N of 1 trial (N=1) is a multiple crossover clinical trial, conducted in a single patient.[1] A trial in which random allocation is used to determine the order in which an experimental and a control intervention are given to a single patient is an N of 1 randomized controlled trial. Some N of 1 trials involve randomized assignment and blinding, but the order of experimental and control interventions can also be fixed by the researcher.[2] This type of study has enabled practitioners to achieve experimental progress without the overwhelming work of designing a group comparison study. This design, especially if including blinding and wash-out periods, can be very effective in confirming causality. The N of 1 trials can be designed in many ways. For example, Single-Patient Open Trials (SPOTs) are located somewhere in between the formal (explanatory) N of 1 trials and the trial and error approach used in clinical practice and are characterized by at least one crossover period with washout in between.[3] One of the most common procedures is the ABA withdrawal experimental design, where the patient problem is measured before a treatment is introduced (baseline) and then measured again during the treatment and finally when the treatment has terminated. If the problem vanished during the treatment it can be established that the treatment was effective. But the N=1 study can also be executed in an AB quasi experimental way; such type-2 N of 1 studies can be effective for testing treatments for severe, rare diseases when the expected effect of the intervention exceeds the effect size of confounders.[4] Another variation is non-concurrent experimental design where different points in time are compared with one another. The standard approach to therapy choice, the trial and error method, may also be included in the N of 1 design.[5] This experimental design also has a problem with causality, whereby statistical significance under a frequentist paradigm may be un-interpretable but other methods, such as clinical significance[6] or Bayesian methods should be considered. Many consider this framework to be a proof of concept or hypothesis generating process to inform subsequent, larger clinical trials. However, N-of-1 trials, if used in clinical practice to inform therapeutic decisions concerned with the patient participating in the trial, can be a promising source of evidence about individual treatment responses, fulfilling the promise of personalized medicine.[7][8]
List of variation in N of 1 trial
| Design | Causality | Use |
|---|---|---|
| A-B | Quasi experiment | Often the only possible method |
| A-A1-A | Experiment | Placebo design where A is no drug and A1 is a placebo |
| A-B-A | Experiment | Withdrawal design where effects of B phase can be established |
| A-B-A-B | Experiment | Withdrawal design where effects of B phase can be established |
| A-B-A-B-A-B | Experiment | Withdrawal design where effects of B phase can be established |
| A-B1-B2-B3-Bn-A | Experiment | Establishing the effect of different versions of B phase |
Quasi experiment means that causality cannot be definitively demonstrated.
Experiment means that it can be demonstrated.
Examples
An N of 1 trial is usually used to assess individual responses to treatments targeting chronic diseases.[9] This design can be successfully implemented to determine optimal treatments for patients with diseases as diverse as osteoarthritis, chronic neuropathic pain and attention deficit hyperactivity disorder.[10]
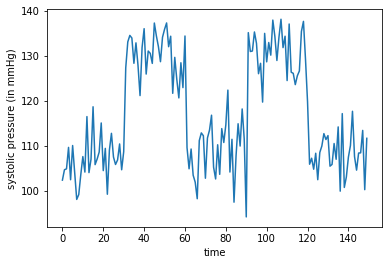
N-of-1 designs can also be observational and describe natural intra-individual changes in health-related behaviours or symptoms longitudinally. N-of-1 observational designs require complex statistical analysis of N-of-1 data however, a simple 10-step procedure is available. [11] There has also been work to adapt causal inference counterfactual methods for using n-of-1 observational studies to design subsequent n-of-1 trials.[12]
While N-of-1 trials are increasing, results of a recent systematic review found that statistical analyses in these studies would improve with more methodological and statistical rigor across all periods of the studies.[13]
The Quantified Self
Recently, a proliferation of personal experiments akin to N=1 is occurring, along with some detailed reports about them. This trend has been sparked in part by the growing ease of collecting data and analysing it, and also motivated by the ability of individuals to report such data easily.[14]
A famous proponent and active experimenter was Seth Roberts, who reported on his self-experimental findings on his blog, and later published The Shangri-La Diet based on his conclusions from these self-experiments.
Global networks
The International Collaborative Network for N-of-1 Trials and Single-Case Designs (ICN) is a global network for clinicians, researchers and consumers who have an interest in these methods. There are over 400 members of the ICN who are based in over 30 countries across the globe. The ICN was established in 2017 and is co-chaired by A/Prof. Jane Nikles and Dr Suzanne McDonald.
See also
References
- ↑ "Introduction to N-of-1 Trials: Indications and Barriers (Chapter 1) | Effective Health Care (EHC) Program". https://effectivehealthcare.ahrq.gov/products/n-1-trials/research-2014-4#toc-1.
- ↑ Punja, Salima; Bukutu, Cecilia; Shamseer, Larissa; Sampson, Margaret; Hartling, Lisa; Urichuk, Liana; Vohra, Sunita (August 2016). "N-of-1 trials are a tapestry of heterogeneity". Journal of Clinical Epidemiology 76: 47–56. doi:10.1016/j.jclinepi.2016.03.023. ISSN 1878-5921. PMID 27079847. https://pubmed.ncbi.nlm.nih.gov/27079847/.
- ↑ Smith, Jane; Yelland, Michael; Del Mar, Christopher (2015), Nikles, Jane; Mitchell, Geoffrey, eds., "Single Patient Open Trials (SPOTs)" (in en), The Essential Guide to N-of-1 Trials in Health (Dordrecht: Springer Netherlands): pp. 195–209, doi:10.1007/978-94-017-7200-6_15, ISBN 978-94-017-7200-6, https://doi.org/10.1007/978-94-017-7200-6_15, retrieved 2023-12-31
- ↑ Selker, Harry P.; Cohen, Theodora; D’Agostino, Ralph B.; Dere, Willard H.; Ghaemi, S. Nassir; Honig, Peter K.; Kaitin, Kenneth I.; Kaplan, Heather C. et al. (August 2022). "A Useful and Sustainable Role for N-of-1 Trials in the Healthcare Ecosystem" (in en). Clinical Pharmacology & Therapeutics 112 (2): 224–232. doi:10.1002/cpt.2425. ISSN 0009-9236. PMID 34551122.
- ↑ Kravitz, R. L., Duan, N., Vohra, S., Li, J. (2014). Introduction to N-of-1 trials: indications and barriers. Design and implementation of N-of-1 trials: A user's guide. AHRQ Publication No. 13(14)-EHC122-EF.
- ↑ "Finding Benefit in n-of-1 Trials". JAMA Internal Medicine 179 (3): 453–454. March 2019. doi:10.1001/jamainternmed.2018.8379. PMID 30830189.
- ↑ Serpico, Davide; Maziarz, Mariusz (2023-12-14). "Averaged versus individualized: pragmatic N-of-1 design as a method to investigate individual treatment response" (in en). European Journal for Philosophy of Science 13 (4): 59. doi:10.1007/s13194-023-00559-0. ISSN 1879-4920. https://doi.org/10.1007/s13194-023-00559-0.
- ↑ Nikles, J., & Mitchell, G. (2015). "The Essential Guide to N-of-1 Trials in Health" (in en). SpringerLink. doi:10.1007/978-94-017-7200-6. ISBN 978-94-017-7199-3. https://link.springer.com/content/pdf/10.1007/978-94-017-7200-6.pdf.
- ↑ Duan, Naihua; Kravitz, Richard L.; Schmid, Christopher H. (2013-08-01). "Single-patient (n-of-1) trials: a pragmatic clinical decision methodology for patient-centered comparative effectiveness research". Journal of Clinical Epidemiology. Methods for Comparative Effectiveness Research/Patient-Centered Outcomes Research: From Efficacy to Effectiveness 66 (8, Supplement): S21–S28. doi:10.1016/j.jclinepi.2013.04.006. ISSN 0895-4356. PMID 23849149.
- ↑ "Using N-of-1 trials to improve patient management and save costs". Journal of General Internal Medicine 25 (9): 906–13. September 2010. doi:10.1007/s11606-010-1352-7. PMID 20386995. PMC 2917656. http://iospress.metapress.com/content/t51wg3207328hv38/?genre=article&issn=1387-2877&volume=21&issue=3&spage=967.
- ↑ McDonald, S; Vieira, R; Johnston, D W. (1 January 2020). "Analysing N-of-1 observational data in health psychology and behavioural medicine: a 10-step SPSS tutorial for beginners". Health Psychology and Behavioral Medicine 8 (1): 32–54. doi:10.1080/21642850.2019.1711096. PMID 34040861.
- ↑ "Causal Analysis of Self-tracked Time Series Data Using a Counterfactual Framework for N-of-1 Trials". Methods of Information in Medicine 57 (1): e10–e21. February 2018. doi:10.3414/ME16-02-0044. PMID 29621835.
- ↑ "N-of-1 Randomized Intervention Trials in Health Psychology: A Systematic Review and Methodology Critique". Annals of Behavioral Medicine 52 (9): 731–742. August 2018. doi:10.1093/abm/kax026. PMID 30124759.
- ↑ "The Quantified Self: Fundamental Disruption in Big Data Science and Biological Discovery". Big Data 1 (2): 85–99. June 2013. doi:10.1089/big.2012.0002. PMID 27442063.
Further reading
- "The n-of-1 randomized controlled trial: clinical usefulness. Our three-year experience". Annals of Internal Medicine 112 (4): 293–9. February 1990. doi:10.7326/0003-4819-112-4-293. PMID 2297206.
- "n-of-1 randomized controlled trials: an opportunity for complementary and alternative medicine evaluation". Journal of Alternative and Complementary Medicine 10 (6): 979–84. December 2004. doi:10.1089/acm.2004.10.979. PMID 15673992.
- "Use of an embedded N-of-1 trial to improve adherence and increase information from a clinical study". Contemporary Clinical Trials 26 (3): 397–401. June 2005. doi:10.1016/j.cct.2005.02.004. PMID 15911473.
- "An n-of-1 trial service in clinical practice: testing the effectiveness of stimulants for attention-deficit/hyperactivity disorder". Pediatrics 117 (6): 2040–6. June 2006. doi:10.1542/peds.2005-1328. PMID 16740846.
 |