Medicine:Osteoarthritis
| Osteoarthritis | |
|---|---|
| Other names | Arthrosis, osteoarthrosis, degenerative arthritis, degenerative joint disease |
 | |
| The formation of hard knobs at the middle finger joints (known as Bouchard's nodes) and at the farthest joints of the fingers (known as Heberden's nodes) is a common feature of osteoarthritis in the hands. | |
| Pronunciation | |
| Specialty | Rheumatology, orthopedics |
| Symptoms | Joint pain, stiffness, joint swelling, decreased range of motion[1] |
| Usual onset | Over years[1] |
| Causes | Connective tissue disease, previous joint injury, abnormal joint or limb development, inherited factors[1][2] |
| Risk factors | Overweight, legs of different lengths, job with high levels of joint stress[1][2] |
| Diagnostic method | Based on symptoms, supported by other testing[1] |
| Treatment | Exercise, efforts to decrease joint stress, support groups, pain medications, joint replacement[1][2][3] |
| Frequency | 237 million / 3.3% (2015)[4] |
Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone .[5][6] It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone.[7] The most common symptoms are joint pain and stiffness.[1] Usually the symptoms progress slowly over years.[1] Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs.[1] The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back.[1] The symptoms can interfere with work and normal daily activities.[1] Unlike some other types of arthritis, only the joints, not internal organs, are affected.[1]
Causes include previous joint injury, abnormal joint or limb development, and inherited factors.[1][2] Risk is greater in those who are overweight, have legs of different lengths, or have jobs that result in high levels of joint stress.[1][2][8] Osteoarthritis is believed to be caused by mechanical stress on the joint and low grade inflammatory processes.[9] It develops as cartilage is lost and the underlying bone becomes affected.[1] As pain may make it difficult to exercise, muscle loss may occur.[2][10] Diagnosis is typically based on signs and symptoms, with medical imaging and other tests used to support or rule out other problems.[1] In contrast to rheumatoid arthritis, in osteoarthritis the joints do not become hot or red.[1]
Treatment includes exercise, decreasing joint stress such as by rest or use of a cane, support groups, and pain medications.[1][3] Weight loss may help in those who are overweight.[1] Pain medications may include paracetamol (acetaminophen) as well as NSAIDs such as naproxen or ibuprofen.[1] Long-term opioid use is not recommended due to lack of information on benefits as well as risks of addiction and other side effects.[1][3] Joint replacement surgery may be an option if there is ongoing disability despite other treatments.[2] An artificial joint typically lasts 10 to 15 years.[11]
Osteoarthritis is the most common form of arthritis, affecting about 237 million people or 3.3% of the world's population, as of 2015.[4][12] It becomes more common as people age.[1] Among those over 60 years old, about 10% of males and 18% of females are affected.[2] Osteoarthritis is the cause of about 2% of years lived with disability.[12]
Signs and symptoms
The main symptom is pain, causing loss of ability and often stiffness. The pain is typically made worse by prolonged activity and relieved by rest. Stiffness is most common in the morning, and typically lasts less than thirty minutes after beginning daily activities, but may return after periods of inactivity. Osteoarthritis can cause a crackling noise (called "crepitus") when the affected joint is moved, especially shoulder and knee joint. A person may also complain of joint locking and joint instability. These symptoms would affect their daily activities due to pain and stiffness.[13] Some people report increased pain associated with cold temperature, high humidity, or a drop in barometric pressure, but studies have had mixed results.[14]
Osteoarthritis commonly affects the hands, feet, spine, and the large weight-bearing joints, such as the hips and knees, although in theory, any joint in the body can be affected. As osteoarthritis progresses, movement patterns (such as gait), are typically affected.[1] Osteoarthritis is the most common cause of a joint effusion of the knee.[15]
In smaller joints, such as at the fingers, hard bony enlargements, called Heberden's nodes (on the distal interphalangeal joints) or Bouchard's nodes (on the proximal interphalangeal joints), may form, and though they are not necessarily painful, they do limit the movement of the fingers significantly. Osteoarthritis of the toes may be a factor causing formation of bunions,[16] rendering them red or swollen.
Causes
Damage from mechanical stress with insufficient self repair by joints is believed to be the primary cause of osteoarthritis.[17] Sources of this stress may include misalignments of bones caused by congenital or pathogenic causes; mechanical injury; excess body weight; loss of strength in the muscles supporting a joint; and impairment of peripheral nerves, leading to sudden or uncoordinated movements.[17] However exercise, including running in the absence of injury, has not been found to increase the risk of knee osteoarthritis.[18][19] Nor has cracking one's knuckles been found to play a role.[20] The risk of osteoarthritis increases with aging.
Primary
The development of osteoarthritis is correlated with a history of previous joint injury and with obesity, especially with respect to knees.[21] Changes in sex hormone levels may play a role in the development of osteoarthritis, as it is more prevalent among post-menopausal women than among men of the same age.[1][22] Conflicting evidence exists for the differences in hip and knee osteoarthritis in African Americans and Caucasians.[23]
Occupational
Increased risk of developing knee and hip osteoarthritis was found among those who work with manual handling (e.g. lifting), have physically demanding work, walk at work, and have climbing tasks at work (e.g. climb stairs or ladders).[8] With hip osteoarthritis, in particular, increased risk of development over time was found among those who work in bent or twisted positions.[8] For knee osteoarthritis, in particular, increased risk was found among those who work in a kneeling or squatting position, experience heavy lifting in combination with a kneeling or squatting posture, and work standing up.[8] Women and men have similar occupational risks for the development of osteoarthritis.[8]
Secondary
This type of osteoarthritis is caused by other factors but the resulting pathology is the same as for primary osteoarthritis:
- Alkaptonuria[24]
- Congenital disorders of joints[25][26]
- Diabetes doubles the risk of having a joint replacement due to osteoarthritis and people with diabetes have joint replacements at a younger age than those without diabetes.[27]
- Ehlers-Danlos syndrome[28]
- Hemochromatosis and Wilson's disease[29]
- Inflammatory diseases (such as Perthes' disease), (Lyme disease), and all chronic forms of arthritis (e.g., costochondritis, gout, and rheumatoid arthritis). In gout, uric acid crystals cause the cartilage to degenerate at a faster pace.
- Injury to joints or ligaments (such as the ACL) as a result of an accident or orthopedic operations.
- Ligamentous deterioration or instability may be a factor.
- Marfan syndrome[30]
- Obesity[31]
- Joint infection[32][33][34]
Pathophysiology
While osteoarthritis is a degenerative joint disease that may cause gross cartilage loss and morphological damage to other joint tissues, more subtle biochemical changes occur in the earliest stages of osteoarthritis progression. The water content of healthy cartilage is finely balanced by compressive force driving water out and hydrostatic and osmotic pressure drawing water in.[36][37] Collagen fibres exert the compressive force, whereas the Gibbs–Donnan effect and cartilage proteoglycans create osmotic pressure which tends to draw water in.[37]
However, during onset of osteoarthritis, the collagen matrix becomes more disorganized and there is a decrease in proteoglycan content within cartilage. The breakdown of collagen fibers results in a net increase in water content.[38][39][40][41][42] This increase occurs because whilst there is an overall loss of proteoglycans (and thus a decreased osmotic pull),[39][43] it is outweighed by a loss of collagen.[37][43]
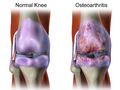
Other structures within the joint can also be affected.[44] The ligaments within the joint become thickened and fibrotic, and the menisci can become damaged and wear away.[45] Menisci can be completely absent by the time a person undergoes a joint replacement. New bone outgrowths, called "spurs" or osteophytes, can form on the margins of the joints, possibly in an attempt to improve the congruence of the articular cartilage surfaces in the absence of the menisci. The subchondral bone volume increases and becomes less mineralized (hypomineralization).[46] All these changes can cause problems functioning. The pain in an osteoarthritic joint has been related to thickened synovium[47] and to subchondral bone lesions.[48]
Diagnosis
Diagnosis is made with reasonable certainty based on history and clinical examination.[49][50] X-rays may confirm the diagnosis. The typical changes seen on X-ray include: joint space narrowing, subchondral sclerosis (increased bone formation around the joint), subchondral cyst formation, and osteophytes.[51] Plain films may not correlate with the findings on physical examination or with the degree of pain.[52]
In 1990, the American College of Rheumatology, using data from a multi-center study, developed a set of criteria for the diagnosis of hand osteoarthritis based on hard tissue enlargement and swelling of certain joints.[53] These criteria were found to be 92% sensitive and 98% specific for hand osteoarthritis versus other entities such as rheumatoid arthritis and spondyloarthropathies.[54]
-
Severe osteoarthritis and osteopenia of the carpal joint and 1st carpometacarpal joint
-
MRI of osteoarthritis in the knee, with characteristic narrowing of the joint space
-
Primary osteoarthritis of the left knee. Note the osteophytes, narrowing of the joint space (arrow), and increased subchondral bone density (arrow).
-
Damaged cartilage from sows. (a) cartilage erosion (b)cartilage ulceration (c)cartilage repair (d)osteophyte (bone spur) formation.
-
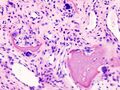
Histopathology of osteoarthrosis of a knee joint in an elderly female
-
Histopathology of osteoarthrosis of a knee joint in an elderly female
-
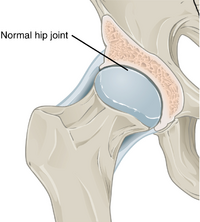
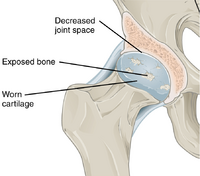
In a healthy joint, the ends of bones are encased in smooth cartilage. Together, they are protected by a joint capsule lined with a synovial membrane that produces synovial fluid. The capsule and fluid protect the cartilage, muscles, and connective tissues.
-
With osteoarthritis, the cartilage becomes worn away. Spurs grow out from the edge of the bone, and synovial fluid increases. Altogether, the joint feels stiff and sore.
-
Osteoarthritis
-
Bone (left) and clinical (right) changes of the hand in osteoarthritis
Classification
A number of classification systems are used for gradation of osteoarthritis:
- WOMAC scale, taking into account pain, stiffness and functional limitation.[55]
- Kellgren-Lawrence grading scale for osteoarthritis of the knee. It uses only projectional radiography features.
- Tönnis classification for osteoarthritis of the hip joint, also using only projectional radiography features.[56]

Both primary generalized nodal osteoarthritis and erosive osteoarthritis (EOA, also called inflammatory osteoarthritis) are sub-sets of primary osteoarthritis. EOA is a much less common, and more aggressive inflammatory form of osteoarthritis which often affects the distal interphalangeal joints of the hand and has characteristic articular erosive changes on X-ray.[57]
Management
Lifestyle modification (such as weight loss and exercise) and pain medications are the mainstays of treatment. Acetaminophen (also known as paracetamol) is recommended first line, with NSAIDs being used as add-on therapy only if pain relief is not sufficient.[58][59] Medications that alter the course of the disease have not been found as of 2018.[60] Recommendations include modification of risk factors through targeted interventions including 1) obesity and overweight, 2) physical activity, 3) dietary exposures, 4) comorbidity, 5) biomechanical factors, 6) occupational factors.[61]
Successful management of the condition is often made more difficult by differing priorities and poor communication between clinicians and people with osteoarthritis. Realistic treatment goals can be achieved by developing a shared understanding of the condition, actively listening to patient concerns, avoiding medical jargon and tailoring treatment plans to the patient's needs.[62][63]
Lifestyle changes
For overweight people, weight loss may be an important factor.[64] Weight loss and exercise provides long-term treatment and advocated in patients with OA. As an adjunct to these lifestyle changes, use of analgesia, intra-articular cortisone injection and consideration of hyaluronic acids and platelet-rich plasma are recommended for pain relief in patients with knee osteoarthritis.[65] Patient education has been shown to be helpful in the self-management of arthritis.[64] It decreases pain, improves function, reduces stiffness and fatigue, and reduces medical usage.[64] Patient education can provide on average 20% more pain relief when compared to NSAIDs alone.[64]
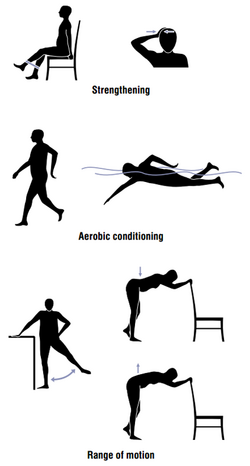
Physical measures
Moderate exercise may be beneficial with respect to pain and function in those with osteoarthritis of the knee and hip.[66][67][68] These exercises should occur at least three times per week.[69] While some evidence supports certain physical therapies, evidence for a combined program is limited.[70] Providing clear advice, making exercises enjoyable, and reassuring people about the importance of doing exercises may lead to greater benefit and more participation.[68] Limited evidence suggests that supervised exercise therapy may improve exercise adherence.[71] There is not enough evidence to determine the effectiveness of massage therapy.[72] The evidence for manual therapy is inconclusive.[73] A 2015 review indicated that aquatic therapy is safe, effective, and can be an adjunct therapy for knee osteoarthritis.[74]
Functional, gait, and balance training have been recommended to address impairments of position sense, balance, and strength in individuals with lower extremity arthritis, as these can contribute to a higher rate of falls in older individuals.[75][76] For people with hand osteoarthritis, exercises may provide small benefits for improving hand function, reducing pain, and relieving finger joint stiffness.[77]
Lateral wedge insoles and neutral insoles do not appear to be useful in osteoarthritis of the knee.[78][79][80] Knee braces may help[81] but their usefulness has also been disputed.[80] For pain management heat can be used to relieve stiffness, and cold can relieve muscle spasms and pain.[82] Among people with hip and knee osteoarthritis, exercise in water may reduce pain and disability, and increase quality of life in the short term.[83] Also therapeutic exercise programs such as aerobics and walking reduce pain and improve physical functioning for up to 6 months after the end of the program for people with knee osteoarthritis.[84] In a study conducted over a period of 2 years on a group of individuals, a research team found that for every additional 1,000 steps per day, there was a 16% reduction in functional limitations in cases of knee osteoarthritis.[85] Hydrotherapy might also be an advantage on the management of pain, disability and quality of life reported by people with osteoarthritis.[86]
Medication
| Treatment recommendations by risk factors | ||
|---|---|---|
| GI risk | CVD risk | Option |
| Low | Low | NSAID, or paracetamol[87] |
| Moderate | Low | Paracetamol, or low dose NSAID with antacid[87] |
| Low | Moderate | Paracetamol, or low dose aspirin with an antacid[87] |
| Moderate | Moderate | Low dose paracetamol, aspirin, and antacid. Monitoring for abdominal pain or black stool.[87] |
By mouth
The pain medication paracetamol (acetaminophen) is the first line treatment for osteoarthritis.[58][88] Pain relief does not differ according to dosage.[59] However, a 2015 review found acetaminophen to have only a small short-term benefit with some laboratory concerns of liver inflammation.[89] For mild to moderate symptoms effectiveness of acetaminophen is similar to non-steroidal anti-inflammatory drugs (NSAIDs) such as naproxen, though for more severe symptoms NSAIDs may be more effective.[58] NSAIDs are associated with greater side effects such as gastrointestinal bleeding.[58]
Another class of NSAIDs, COX-2 selective inhibitors (such as celecoxib) are equally effective when compared to nonselective NSAIDs, and have lower rates of adverse gastrointestinal effects, but higher rates of cardiovascular disease such as myocardial infarction.[90] They are also more expensive than non-specific NSAIDs.[91] Benefits and risks vary in individuals and need consideration when making treatment decisions,[92] and further unbiased research comparing NSAIDS and COX-2 selective inhibitors is needed.[93] NSAIDS applied topically are effective for a small number of people.[94] The COX-2 selective inhibitor rofecoxib was removed from the market in 2004, as cardiovascular events were associated with long term use.[95]
Failure to achieve desired pain relief in osteoarthritis after two weeks should trigger reassessment of dosage and pain medication.[96] Opioids by mouth, including both weak opioids such as tramadol and stronger opioids, are also often prescribed. Their appropriateness is uncertain, and opioids are often recommended only when first line therapies have failed or are contraindicated.[3][97] This is due to their small benefit and relatively large risk of side effects.[98][99] The use of tramadol likely does not improve pain or physical function and likely increases the incidence of adverse side effects.[99] Oral steroids are not recommended in the treatment of osteoarthritis.[88]
Use of the antibiotic doxycycline orally for treating osteoarthritis is not associated with clinical improvements in function or joint pain.[100] Any small benefit related to the potential for doxycycline therapy to address the narrowing of the joint space is not clear, and any benefit is outweighed by the potential harm from side effects.[100]
A 2018 meta-analysis found that oral collagen supplementation for the treatment of osteoarthritis reduces stiffness but does not improve pain and functional limitation.[101]
Topical
There are several NSAIDs available for topical use, including diclofenac. A Cochrane review from 2016 concluded that reasonably reliable evidence is available only for use of topical diclofenac and ketoprofen in people aged over 40 years with painful knee arthritis.[94] Transdermal opioid pain medications are not typically recommended in the treatment of osteoarthritis.[98] The use of topical capsaicin to treat osteoarthritis is controversial, as some reviews found benefit[102][103] while others did not.[104]
Joint injections

Local drug delivery by intra-articular injection may be more effective and safer in terms of increased bioavailability, less systemic exposure and reduced adverse events.[106] Several intra-articular medications for symptomatic treatment are available on the market as follows.[107]
Steroids
Joint injection of glucocorticoids (such as hydrocortisone) leads to short-term pain relief that may last between a few weeks and a few months.[108] A 2015 Cochrane review found that intra-articular corticosteroid injections of the knee did not benefit quality of life and had no effect on knee joint space; clinical effects one to six weeks after injection could not be determined clearly due to poor study quality.[109] Another 2015 study reported negative effects of intra-articular corticosteroid injections at higher doses,[110] and a 2017 trial showed reduction in cartilage thickness with intra-articular triamcinolone every 12 weeks for 2 years compared to placebo.[111] A 2018 study found that intra-articular triamcinolone is associated with an increase in intraocular pressure.[112]
Hyaluronic acid
Injections of hyaluronic acid have not produced improvement compared to placebo for knee arthritis,[113][114] but did increase risk of further pain.[113] In ankle osteoarthritis, evidence is unclear.[115]
Radiosynoviorthesis
Injection of beta particle-emitting radioisotopes (called radiosynoviorthesis) is used for the local treatment of inflammatory joint conditions.[116]
Platelet-rich plasma
The effectiveness of injections of platelet-rich plasma (PRP) is unclear; there are suggestions that such injections improve function but not pain, and are associated with increased risk.[vague][117][118] A 2014 Cochrane review of studies involving PRP found the evidence to be insufficient.[119]
Surgery
Bone fusion
Arthrodesis (fusion) of the bones may be an option in some types of osteoarthritis. An example is ankle osteoarthritis, in which ankle fusion is considered to be the gold standard treatment in end-stage cases.[120]
Joint replacement
If the impact of symptoms of osteoarthritis on quality of life is significant and more conservative management is ineffective, joint replacement surgery or resurfacing may be recommended. Evidence supports joint replacement for both knees and hips as it is both clinically effective[121][122] and cost-effective.[123][124] People who underwent total knee replacement had improved SF-12 quality of life scores, were feeling better compared to those who did not have surgery, and may have short- and long-term benefits for quality of life in terms of pain and function.[125][126] The beneficial effects of these surgeries may be time-limited due to various environmental factors, comorbidities, and pain in other regions of the body.[127]
For people who have shoulder osteoarthritis and do not respond to medications, surgical options include a shoulder hemiarthroplasty (replacing a part of the joint), and total shoulder arthroplasty (replacing the joint).[128]
Biological joint replacement involves replacing the diseased tissues with new ones. This can either be from the person (autograft) or from a donor (allograft).[129] People undergoing a joint transplant (osteochondral allograft) do not need to take immunosuppressants as bone and cartilage tissues have limited immune responses.[130] Autologous articular cartilage transfer from a non-weight-bearing area to the damaged area, called osteochondral autograft transfer system, is one possible procedure that is being studied.[131] When the missing cartilage is a focal defect, autologous chondrocyte implantation is also an option.[132]
Shoulder replacement
For those with osteoarthritis in the shoulder, a complete shoulder replacement is sometimes suggested to improve pain and function.[133] Demand for this treatment is expected to increase by 750% by the year 2030.[133] There are different options for shoulder replacement surgeries, however, there is a lack of evidence in the form of high-quality randomized controlled trials, to determine which type of shoulder replacement surgery is most effective in different situations, what are the risks involved with different approaches, or how the procedure compares to other treatment options.[133][134] There is some low-quality evidence that indicates that when comparing total shoulder arthroplasty over hemiarthroplasty, no large clinical benefit was detected in the short term.[134] It is not clear if the risk of harm differs between total shoulder arthroplasty or a hemiarthroplasty approach.[134]
Other surgical options
Osteotomy may be useful in people with knee osteoarthritis, but has not been well studied and it is unclear whether it is more effective than non-surgical treatments or other types of surgery.[135][136] Arthroscopic surgery is largely not recommended, as it does not improve outcomes in knee osteoarthritis,[137][138] and may result in harm.[139] It is unclear whether surgery is beneficial in people with mild to moderate knee osteoarthritis.[136]
Unverified treatments
Glucosamine and chondroitin
The effectiveness of glucosamine is controversial.[140] Reviews have found it to be equal to[141][142] or slightly better than placebo.[143][144] A difference may exist between glucosamine sulfate and glucosamine hydrochloride, with glucosamine sulfate showing a benefit and glucosamine hydrochloride not.[145] The evidence for glucosamine sulfate having an effect on osteoarthritis progression is somewhat unclear and if present likely modest.[146] The Osteoarthritis Research Society International recommends that glucosamine be discontinued if no effect is observed after six months[147] and the National Institute for Health and Care Excellence no longer recommends its use.[10] Despite the difficulty in determining the efficacy of glucosamine, it remains a treatment option.[148] The European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) recommends glucosamine sulfate and chondroitin sulfate for knee osteoarthritis.[149] Its use as a therapy for osteoarthritis is usually safe.[148][150]
A 2015 Cochrane review of clinical trials of chondroitin found that most were of low quality, but that there was some evidence of short-term improvement in pain and few side effects; it does not appear to improve or maintain the health of affected joints.[151]
Supplements
Avocado–soybean unsaponifiables (ASU) is an extract made from avocado oil and soybean oil[152] sold under many brand names worldwide as a dietary supplement[153] and as a prescription drug in France.[154] A 2014 Cochrane review found that while ASU might help relieve pain in the short term for some people with osteoarthritis, it does not appear to improve or maintain the health of affected joints.[152] The review noted a high-quality, two-year clinical trial comparing ASU to chondroitin – which has uncertain efficacy in osteoarthritis – with no difference between the two agents.[152] The review also found there is insufficient evidence of ASU safety.[152]
A few high-quality studies of Boswellia serrata show consistent, but small, improvements in pain and function.[152] Curcumin,[155] phytodolor,[102] and s-adenosyl methionine (SAMe)[102][72] may be effective in improving pain. A 2009 Cochrane review recommended against the routine use of SAMe, as there has not been sufficient high-quality clinical research to prove its effect.[156] A 2021 review found that hydroxychloroquine (HCQ) had no benefit in reducing pain and improving physical function in hand or knee osteoarthritis, and the off-label use of HCQ for people with osteoarthritis should be discouraged.[157] There is no evidence for the use of colchicine for treating the pain of hand or knee arthritis.[158]
There is limited evidence to support the use of hyaluronan,[159] methylsulfonylmethane,[102] rose hip,[102] capsaicin,[102] or vitamin D.[102][160]
Acupuncture and other interventions
While acupuncture leads to improvements in pain relief, this improvement is small and may be of questionable importance.[161] Waiting list–controlled trials for peripheral joint osteoarthritis do show clinically relevant benefits, but these may be due to placebo effects.[162][163] Acupuncture does not seem to produce long-term benefits.[164]
Electrostimulation techniques such as TENS have been used for twenty years to treat osteoarthritis in the knee. However, there is no conclusive evidence to show that it reduces pain or disability.[165] A Cochrane review of low-level laser therapy found unclear evidence of benefit,[166] whereas another review found short-term pain relief for osteoarthritic knees.[167]
Further research is needed to determine if balnotherapy for osteoarthritis (mineral baths or spa treatments) improves a person's quality of life or ability to function.[168] The use of ice or cold packs may be beneficial; however, further research is needed.[169] There is no evidence of benefit from placing hot packs on joints.[169]
There is low quality evidence that therapeutic ultrasound may be beneficial for people with osteoarthritis of the knee; however, further research is needed to confirm and determine the degree and significance of this potential benefit.[170]
Therapeutic ultrasound may relieve pain compared to conventional non-drug ultrasound however phonopheresis does not produce additional benefits to functional improvement. It is safe treatment to relieve pain and improve physical function in patients with knee osteoarthritis.[171]
Continuous and pulsed ultrasound modes (especially 1 MHz, 2.5 W/cm2, 15min/ session, 3 session/ week, during 8 weeks protocol) may be effective in improving patients physical function and pain.[172]
There is weak evidence suggesting that electromagnetic field treatment may result in moderate pain relief; however, further research is necessary and it is not known if electromagnetic field treatment can improve quality of life or function.[173]
Viscosupplementation for osteoarthritis of the knee may have positive effects on pain and function at 5 to 13 weeks post-injection.[174]
Epidemiology
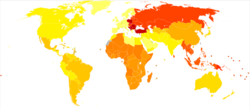
| no data ≤ 200 200–220 220–240 240–260 260–280 280–300 | 300–320 320–340 340–360 360–380 380–400 ≥ 400 |
Globally, as of 2010[update], approximately 250 million people had osteoarthritis of the knee (3.6% of the population).[176][177] Hip osteoarthritis affects about 0.85% of the population.[176]
As of 2004[update], osteoarthritis globally causes moderate to severe disability in 43.4 million people.[178] Together, knee and hip osteoarthritis had a ranking for disability globally of 11th among 291 disease conditions assessed.[176]
Middle East and North Africa (MENA)
In the Middle East and North Africa from 1990 to 2019, the prevalence of people with hip osteoarthritis increased three–fold over the three decades, a total of 1.28 million cases.[179] It increased 2.88-fold, from 6.16 million cases to 17.75 million, between 1990 and 2019 for knee osteoarthritis.[180] Hand osteoarthritis in MENA also increased 2.7-fold, from 1.6 million cases to 4.3 million from 1990 to 2019.[181]
USA
As of 2012[update], osteoarthritis affected 52.5 million people in the United States, approximately 50% of whom were 65 years or older.[182] It is estimated that 80% of the population have radiographic evidence of osteoarthritis by age 65, although only 60% of those will have symptoms.[183] The rate of osteoarthritis in the United States is forecast to be 78 million (26%) adults by 2040.[182]
In the United States, there were approximately 964,000 hospitalizations for osteoarthritis in 2011, a rate of 31 stays per 10,000 population.[184] With an aggregate cost of $14.8 billion ($15,400 per stay), it was the second-most expensive condition seen in U.S. hospital stays in 2011. By payer, it was the second-most costly condition billed to Medicare and private insurance.[185][186]
Europe
In Europe, the number of individuals affected by osteoarthritis has increased from 27.9 million in 1990 to 50.8 million in 2019. Hand osteoarthritis was the second most prevalent type, affecting an estimated 12.5 million people. In 2019, Knee osteoarthritis was the 18th most common cause of years lived with disability (YLDs) in Europe, accounting for 1.28% of all YLDs. This has increased from 1.12% in 1990.[187]
India
In India, the number of individuals affected by osteoarthritis has increased from 23.46 million in 1990 to 62.35 million in 2019. Knee osteoarthritis was the most prevalent type of osteoarthritis, followed by hand osteoarthritis. In 2019, osteoarthritis was the 20th most common cause of years lived with disability (YLDs) in India, accounting for 1.48% of all YLDs, which increased from 1.25% and 23rd most common cause in 1990.[188]
History
Etymology
Osteoarthritis is derived from the prefix osteo- (from Ancient Greek:) combined with arthritis (from ἀρθρῖτῐς, arthrîtis, lit. 'of or in the joint'), which is itself derived from arthr- (from ἄρθρον, árthron, lit. 'joint, limb') and -itis (from -ῖτις, -îtis, lit. 'pertaining to'), the latter suffix having come to be associated with inflammation.[189] The -itis of osteoarthritis could be considered misleading as inflammation is not a conspicuous feature. Some clinicians refer to this condition as osteoarthrosis to signify the lack of inflammatory response,[190] the suffix -osis (from -ωσις, -ōsis, lit. '(abnormal) state, condition, or action') simply referring to the pathosis itself.
Other animals
Osteoarthritis has been reported in several species of animals all over the world, including marine animals and even some fossils; including but not limited to: cats, many rodents, cattle, deer, rabbits, sheep, camels, elephants, buffalo, hyena, lions, mules, pigs, tigers, kangaroos, dolphins, dugong, and horses.[191]
Osteoarthritis has been reported in fossils of the large carnivorous dinosaur Allosaurus fragilis.[192]
Research
Therapies
Pharmaceutical agents that will alter the natural history of disease progression by arresting joint structural change and ameliorating symptoms are termed as disease modifying therapy (DMOAD).[60] Therapies under investigation include the following:
- Strontium ranelate – may decrease degeneration in osteoarthritis and improve outcomes[193][194]
- Gene therapy – Gene transfer strategies aim to target the disease process rather than the symptoms.[195] Cell-mediated gene therapy is also being studied.[196][197] One version was approved in South Korea for the treatment of moderate knee osteoarthritis, but later revoked for the mislabeling and the false reporting of an ingredient used.[198][199] The drug was administered intra-articularly.[199]
Cause
As well as attempting to find disease-modifying agents for osteoarthritis, there is emerging evidence that a system-based approach is necessary to find the causes of osteoarthritis.[200]
Diagnostic biomarkers
Guidelines outlining requirements for inclusion of soluble biomarkers in osteoarthritis clinical trials were published in 2015,[201] but there are no validated biomarkers used clinically to detect osteoarthritis, as of 2021.[202][203]
A 2015 systematic review of biomarkers for osteoarthritis looking for molecules that could be used for risk assessments found 37 different biochemical markers of bone and cartilage turnover in 25 publications.[204] The strongest evidence was for urinary C-terminal telopeptide of type II collagen (uCTX-II) as a prognostic marker for knee osteoarthritis progression, and serum cartilage oligomeric matrix protein (COMP) levels as a prognostic marker for incidence of both knee and hip osteoarthritis. A review of biomarkers in hip osteoarthritis also found associations with uCTX-II.[205] Procollagen type II C-terminal propeptide (PIICP) levels reflect type II collagen synthesis in body and within joint fluid PIICP levels can be used as a prognostic marker for early osteoarthritis.[206]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 "Osteoarthritis". National Institute of Arthritis and Musculoskeletal and Skin Diseases. April 2015. http://www.niams.nih.gov/health_info/Osteoarthritis/default.asp.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 "Osteoarthritis". Lancet 386 (9991): 376–387. July 2015. doi:10.1016/S0140-6736(14)60802-3. PMID 25748615.
- ↑ 3.0 3.1 3.2 3.3 "OARSI guidelines for the non-surgical management of knee osteoarthritis". Osteoarthritis and Cartilage 22 (3): 363–388. March 2014. doi:10.1016/j.joca.2014.01.003. PMID 24462672.
- ↑ 4.0 4.1 "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1545–1602. October 2016. doi:10.1016/S0140-6736(16)31678-6. PMID 27733282.
- ↑ Atlas of Osteoarthritis. Springer. 2015. p. 21. ISBN 978-1910315163. https://books.google.com/books?id=qT1FBgAAQBAJ&pg=PA21.
- ↑ "A National Public Health Agenda for Osteoarthritis 2020". 27 July 2020. https://www.cdc.gov/arthritis/docs/oaagenda2020.pdf.
- ↑ "Osteoarthritis". Lancet 393 (10182): 1745–1759. April 2019. doi:10.1016/S0140-6736(19)30417-9. PMID 31034380.
- ↑ 8.0 8.1 8.2 8.3 8.4 Occupational Exposures and Osteoarthritis: A systematic review and assessment of medical, social and ethical aspects (Report). Graphic design by Anna Edling. Stockholm: Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). 1 September 2016. p. 1. 253 (in Swedish). https://www.sbu.se/en/publications/sbu-assesses/occupational-exposures-and-osteoarthritis/. Retrieved 8 April 2018.
- ↑ "Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!)". Osteoarthritis and Cartilage 21 (1): 16–21. January 2013. doi:10.1016/j.joca.2012.11.012. PMID 23194896.
- ↑ 10.0 10.1 "Osteoarthritis – Care and management in adults" (PDF). 2014. http://www.nice.org.uk/guidance/cg177/evidence/full-guideline-191761309.
- ↑ "Biotribology of artificial hip joints". World Journal of Orthopedics 6 (1): 77–94. January 2015. doi:10.5312/wjo.v6.i1.77. PMID 25621213.
- ↑ 12.0 12.1 "Burden of disability due to musculoskeletal (MSK) disorders". Best Practice & Research. Clinical Rheumatology 28 (3): 353–366. June 2014. doi:10.1016/j.berh.2014.08.002. PMID 25481420.
- ↑ "Osteoarthritis: diagnosis and treatment". American Family Physician 85 (1): 49–56. January 2012. PMID 22230308. https://www.aafp.org/afp/2012/0101/p49.html.
- ↑ "Influence of meteorological elements on osteoarthritis pain: a review of the literature" (in pt). Revista Brasileira de Reumatologia 51 (6): 622–628. December 2011. doi:10.1590/S0482-50042011000600008. PMID 22124595.
- ↑ "Swollen knee". Mayo Clinic. 2017. http://www.mayoclinic.org/diseases-conditions/swollen-knee/basics/definition/con-20026072.
- ↑ "Bunions: Symptoms and causes". Mayo Clinic. 8 November 2016. http://www.mayoclinic.org/diseases-conditions/bunions/symptoms-causes/dxc-20262053.
- ↑ 17.0 17.1 "Etiopathogenesis of osteoarthritis". The Medical Clinics of North America 93 (1): 1–24, xv. January 2009. doi:10.1016/j.mcna.2008.08.009. PMID 19059018.
- ↑ "Exercise and knee osteoarthritis: benefit or hazard?". Canadian Family Physician 55 (9): 871–878. September 2009. PMID 19752252.
- ↑ "Running and Knee Osteoarthritis: A Systematic Review and Meta-analysis". The American Journal of Sports Medicine 45 (6): 1447–1457. May 2017. doi:10.1177/0363546516657531. PMID 27519678. http://eprints.lincoln.ac.uk/id/eprint/23789/1/23789%20Timminsetal_RunningOAreview_AJSM_submitted.pdf.
- ↑ "Knuckle cracking and hand osteoarthritis". Journal of the American Board of Family Medicine 24 (2): 169–174. 2011. doi:10.3122/jabfm.2011.02.100156. PMID 21383216.
- ↑ "Knee osteoarthritis and obesity". International Journal of Obesity and Related Metabolic Disorders 25 (5): 622–627. May 2001. doi:10.1038/sj.ijo.0801585. PMID 11360143.
- ↑ "Sex hormones and structural changes in osteoarthritis: a systematic review". Maturitas 69 (2): 141–156. June 2011. doi:10.1016/j.maturitas.2011.03.019. PMID 21481553.
- ↑ "Osteoarthritis: new insights. Part 1: the disease and its risk factors". Annals of Internal Medicine 133 (8): 635–646. October 2000. doi:10.7326/0003-4819-133-8-200010170-00016. PMID 11033593.
- ↑ "Recent advances in management of alkaptonuria (invited review; best practice article)". Journal of Clinical Pathology 66 (5): 367–373. May 2013. doi:10.1136/jclinpath-2012-200877. PMID 23486607.
- ↑ "Birth Defects: Condition Information". September 2017. https://www.nichd.nih.gov/health/topics/birthdefects/conditioninfo/Pages/default.aspx.
- ↑ "Congenital Disorders of Sexual Development". https://www.lecturio.com/concepts/congenital-disorders-of-sexual-development/.
- ↑ "The adverse effects of diabetes on osteoarthritis: update on clinical evidence and molecular mechanisms". Osteoarthritis and Cartilage 23 (6): 841–850. June 2015. doi:10.1016/j.joca.2015.03.031. PMID 25837996.
- ↑ "Ehlers-Danlos Syndrome". https://www.lecturio.com/concepts/ehlers-danlos-syndrome/.
- ↑ "Hereditary Hemochromatosis". https://www.lecturio.com/concepts/hereditary-hemochromatosis/.
- ↑ "Marfan Syndrome". https://www.lecturio.com/concepts/marfan-syndrome/.
- ↑ "Obesity". https://www.lecturio.com/concepts/obesity/.
- ↑ "Arthritis, Infectious". 2009. https://rarediseases.org/rare-diseases/arthritis-infectious/.
- ↑ "Approach to septic arthritis". American Family Physician 84 (6): 653–660. September 2011. PMID 21916390.
- ↑ "Acute osteoarticular infections in children are frequently forgotten multidiscipline emergencies: beyond the technical skills". EFORT Open Reviews 6 (7): 584–592. July 2021. doi:10.1302/2058-5241.6.200155. PMID 34377550.
- ↑ "Synovial Joints". OpenStax CNX. 25 April 2013. http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@7.30:59/Synovial-Joints.
- ↑ "The mechanobiology of articular cartilage: bearing the burden of osteoarthritis". Current Rheumatology Reports 16 (10): 451. October 2014. doi:10.1007/s11926-014-0451-6. PMID 25182679.
- ↑ 37.0 37.1 37.2 "Balance between swelling pressure and collagen tension in normal and degenerate cartilage". Nature 260 (5554): 808–809. April 1976. doi:10.1038/260808a0. PMID 1264261. Bibcode: 1976Natur.260..808M.
- ↑ "Biochemical Findings in Normal and Osteoarthritic Articular Cartilage. II. Chondroitin Sulfate Concentration and Chain Length, Water, and Ash Content". The Journal of Clinical Investigation 45 (7): 1170–1177. July 1966. doi:10.1172/JCI105423. PMID 16695915.
- ↑ 39.0 39.1 "The composition of normal and osteoarthritic articular cartilage from human knee joints. With special reference to unicompartmental replacement and osteotomy of the knee". The Journal of Bone and Joint Surgery. American Volume 66 (1): 95–106. January 1984. doi:10.2106/00004623-198466010-00013. PMID 6690447.
- ↑ "Correlation between the MR T2 value at 4.7 T and relative water content in articular cartilage in experimental osteoarthritis induced by ACL transection". Osteoarthritis and Cartilage 17 (4): 441–447. April 2009. doi:10.1016/j.joca.2008.09.009. PMID 18990590.
- ↑ "Some biochemical and biophysical parameters for the study of the pathogenesis of osteoarthritis: a comparison between the processes of ageing and degeneration in human hip cartilage". Connective Tissue Research 19 (2–4): 149–176. 1989. doi:10.3109/03008208909043895. PMID 2805680.
- ↑ "Water content and binding in normal and osteoarthritic human cartilage". The Journal of Bone and Joint Surgery. American Volume 57 (1): 76–80. January 1975. doi:10.2106/00004623-197557010-00013. PMID 1123375.
- ↑ 43.0 43.1 "Chemical composition and swelling of normal and osteoarthrotic femoral head cartilage. I. Chemical composition". Annals of the Rheumatic Diseases 36 (2): 121–129. April 1977. doi:10.1136/ard.36.2.121. PMID 856064.
- ↑ "Biological aspects of early osteoarthritis". Knee Surgery, Sports Traumatology, Arthroscopy 20 (3): 407–422. March 2012. doi:10.1007/s00167-011-1705-8. PMID 22009557.
- ↑ "Meniscus pathology, osteoarthritis and the treatment controversy". Nature Reviews. Rheumatology 8 (7): 412–419. May 2012. doi:10.1038/nrrheum.2012.69. PMID 22614907.
- ↑ "Subchondral bone in osteoarthritis: insight into risk factors and microstructural changes". Arthritis Research & Therapy 15 (6): 223. 2013. doi:10.1186/ar4405. PMID 24321104.
- ↑ "Knee effusions, popliteal cysts, and synovial thickening: association with knee pain in osteoarthritis". The Journal of Rheumatology 28 (6): 1330–1337. June 2001. PMID 11409127.
- ↑ "The association of bone marrow lesions with pain in knee osteoarthritis". Annals of Internal Medicine 134 (7): 541–549. April 2001. doi:10.7326/0003-4819-134-7-200104030-00007. PMID 11281736.
- ↑ "EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis". Annals of the Rheumatic Diseases 69 (3): 483–489. March 2010. doi:10.1136/ard.2009.113100. PMID 19762361. http://ard.bmj.com/cgi/content/short/ard.2009.113100v1.
- ↑ "Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care". The Journal of Rheumatology 29 (8): 1713–1718. August 2002. PMID 12180735.
- ↑ Osteoarthritis (OA): Joint Disorders at Merck Manual of Diagnosis and Therapy Professional Edition
- ↑ "Osteoarthritis treatment update: Are NSAIDs still in the picture?". Journal of Musculoskeletal Medicine 27 (2). 2010. http://www.musculoskeletalnetwork.com/display/article/1145622/1517357. Retrieved 9 February 2010.
- ↑ "Patient information: Osteoarthritis symptoms and diagnosis (Beyond the Basics)". UpToDate. 2013. https://www.uptodate.com/contents/osteoarthritis-symptoms-and-diagnosis-beyond-the-basics.
- ↑ "The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand". Arthritis and Rheumatism 33 (11): 1601–1610. November 1990. doi:10.1002/art.1780331101. PMID 2242058.
- ↑ "Health-related quality of life and appropriateness of knee or hip joint replacement". Archives of Internal Medicine 166 (2): 220–226. January 2006. doi:10.1001/archinte.166.2.220. PMID 16432092.
- ↑ "Tönnis Classification of Osteoarthritis by Radiographic Changes". Society of Preventive Hip Surgery. http://www.preventivehip.org/hip-scores/tonnis-classification.
- ↑ "Erosive osteoarthritis". Best Practice & Research. Clinical Rheumatology 18 (5): 739–758. October 2004. doi:10.1016/j.berh.2004.05.010. PMID 15454130.
- ↑ 58.0 58.1 58.2 58.3 "The role of acetaminophen in the treatment of osteoarthritis". The American Journal of Managed Care 16 (Suppl Management): S48–S54. March 2010. PMID 20297877. http://www.ajmc.com/publications/supplement/2010/A278_10mar_Pain/A278_2010mar_Flood/.

- ↑ 59.0 59.1 "Paracetamol versus placebo for knee and hip osteoarthritis". The Cochrane Database of Systematic Reviews 2 (2): CD013273. February 2019. doi:10.1002/14651858.cd013273. PMID 30801133.
- ↑ 60.0 60.1 "Disease-modifying drugs in osteoarthritis: current understanding and future therapeutics". Expert Opinion on Emerging Drugs 23 (4): 331–347. December 2018. doi:10.1080/14728214.2018.1547706. PMID 30415584.
- ↑ "Modifiable risk factors in knee osteoarthritis: treatment implications". Rheumatology International 39 (7): 1145–1157. July 2019. doi:10.1007/s00296-019-04290-z. PMID 30911813.
- ↑ "How to improve discussions about osteoarthritis in primary care" (in en). NIHR Evidence. 23 June 2022. doi:10.3310/nihrevidence_51244. https://evidence.nihr.ac.uk/alert/discussions-about-osteoarthritis-in-primary-care/.
- ↑ "Patient and practitioner priorities and concerns about primary healthcare interactions for osteoarthritis: A meta-ethnography". Patient Education and Counseling 105 (7): 1865–1877. July 2022. doi:10.1016/j.pec.2022.01.009. PMID 35125208.
- ↑ 64.0 64.1 64.2 64.3 "Hip pain and mobility deficits--hip osteoarthritis: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association". The Journal of Orthopaedic and Sports Physical Therapy 39 (4): A1-25. April 2009. doi:10.2519/jospt.2009.0301. PMID 19352008.
- ↑ "Osteoarthritis- a systematic review of long-term safety implications for osteoarthritis of the knee". BMC Musculoskeletal Disorders 20 (1): 151. April 2019. doi:10.1186/s12891-019-2525-0. PMID 30961569.
- ↑ "Exercise therapy for bone and muscle health: an overview of systematic reviews". BMC Medicine 10: 167. December 2012. doi:10.1186/1741-7015-10-167. PMID 23253613.
- ↑ "Exercise for osteoarthritis of the hip". The Cochrane Database of Systematic Reviews 4 (4): CD007912. April 2014. doi:10.1002/14651858.CD007912.pub2. PMID 24756895.
- ↑ 68.0 68.1 "Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review". The Cochrane Database of Systematic Reviews 4 (4): CD010842. April 2018. doi:10.1002/14651858.CD010842.pub2. PMID 29664187.
- ↑ "Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials". Arthritis & Rheumatology 66 (3): 622–636. March 2014. doi:10.1002/art.38290. PMID 24574223.
- ↑ "Physical therapy interventions for knee pain secondary to osteoarthritis: a systematic review". Annals of Internal Medicine 157 (9): 632–644. November 2012. doi:10.7326/0003-4819-157-9-201211060-00007. PMID 23128863.
- ↑ "Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults". The Cochrane Database of Systematic Reviews 2010 (1): CD005956. January 2010. doi:10.1002/14651858.cd005956.pub2. PMID 20091582.
- ↑ 72.0 72.1 "Evidence-Based Evaluation of Complementary Health Approaches for Pain Management in the United States". Mayo Clinic Proceedings 91 (9): 1292–1306. September 2016. doi:10.1016/j.mayocp.2016.06.007. PMID 27594189.
- ↑ "Manual therapy for osteoarthritis of the hip or knee - a systematic review". Manual Therapy 16 (2): 109–117. April 2011. doi:10.1016/j.math.2010.10.011. PMID 21146444.
- ↑ "Effectiveness of aquatic exercise for treatment of knee osteoarthritis: Systematic review and meta-analysis". Zeitschrift für Rheumatologie 74 (6): 543–552. August 2015. doi:10.1007/s00393-014-1559-9. PMID 25691109.
- ↑ "Physiological risk factors for falls in older people with lower limb arthritis". The Journal of Rheumatology 31 (11): 2272–2279. November 2004. PMID 15517643.
- ↑ "Falls and fall injuries among adults with arthritis--United States, 2012". MMWR. Morbidity and Mortality Weekly Report 63 (17): 379–383. May 2014. PMID 24785984.
- ↑ "Exercise for hand osteoarthritis". The Cochrane Database of Systematic Reviews 1 (1): CD010388. January 2017. doi:10.1002/14651858.CD010388.pub2. PMID 28141914.
- ↑ "A systematic review investigating the efficacy of laterally wedged insoles for medial knee osteoarthritis". Rheumatology International 33 (10): 2529–2538. October 2013. doi:10.1007/s00296-013-2760-x. PMID 23612781.
- ↑ "Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis". JAMA 310 (7): 722–730. August 2013. doi:10.1001/jama.2013.243229. PMID 23989797.
- ↑ 80.0 80.1 "Braces and orthoses for treating osteoarthritis of the knee". The Cochrane Database of Systematic Reviews 2015 (3): CD004020. March 2015. doi:10.1002/14651858.CD004020.pub3. PMID 25773267.
- ↑ "Physiotherapy management of knee osteoarthritis". International Journal of Rheumatic Diseases 14 (2): 145–151. May 2011. doi:10.1111/j.1756-185X.2011.01612.x. PMID 21518313.
- ↑ "Osteoarthritis Lifestyle and home remedies". Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/osteoarthritis/basics/lifestyle-home-remedies/con-20014749.
- ↑ "Aquatic exercise for the treatment of knee and hip osteoarthritis". The Cochrane Database of Systematic Reviews 2016 (3): CD005523. March 2016. doi:10.1002/14651858.CD005523.pub3. PMID 27007113.
- ↑ "Exercise for osteoarthritis of the knee". The Cochrane Database of Systematic Reviews 1 (1): CD004376. January 2015. doi:10.1002/14651858.CD004376.pub3. PMID 25569281.
- ↑ "Daily walking and the risk of incident functional limitation in knee osteoarthritis: an observational study". Arthritis Care & Research 66 (9): 1328–1336. September 2014. doi:10.1002/acr.22362. PMID 24923633.
- ↑ "Aquatic exercise for the treatment of knee and hip osteoarthritis". The Cochrane Database of Systematic Reviews 2016 (3): CD005523. March 2016. doi:10.1002/14651858.CD005523.pub3. PMID 27007113.
- ↑ 87.0 87.1 87.2 87.3 "Pain Relief with NSAID Medications". Consumer Reports. January 2016. https://www.consumerreports.org/cro/2013/07/treating-pain-with-nsaid-medications/index.htm.
- ↑ 88.0 88.1 "OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence". Osteoarthritis and Cartilage 15 (9): 981–1000. September 2007. doi:10.1016/j.joca.2007.06.014. PMID 17719803.
- ↑ "Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials". BMJ 350: h1225. March 2015. doi:10.1136/bmj.h1225. PMID 25828856.
- ↑ "Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation". Health Technology Assessment 12 (11): 1–278, iii. April 2008. doi:10.3310/hta12110. PMID 18405470.
- ↑ "Cost-effectiveness analyses of osteoarthritis oral therapies: a systematic review". Applied Health Economics and Health Policy 11 (6): 593–618. December 2013. doi:10.1007/s40258-013-0061-x. PMID 24214160.
- ↑ "Relative benefit-risk comparing diclofenac to other traditional non-steroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors in patients with osteoarthritis or rheumatoid arthritis: a network meta-analysis". Arthritis Research & Therapy 17 (1): 66. March 2015. doi:10.1186/s13075-015-0554-0. PMID 25879879.
- ↑ "Celecoxib for osteoarthritis". The Cochrane Database of Systematic Reviews 5 (5): CD009865. May 2017. doi:10.1002/14651858.CD009865.pub2. PMID 28530031.
- ↑ 94.0 94.1 "Topical NSAIDs for chronic musculoskeletal pain in adults". The Cochrane Database of Systematic Reviews 4 (4): CD007400. April 2016. doi:10.1002/14651858.CD007400.pub3. PMID 27103611.
- ↑ "Rofecoxib for osteoarthritis". The Cochrane Database of Systematic Reviews 2005 (1): CD005115. January 2005. doi:10.1002/14651858.CD005115. PMID 15654705.
- ↑ "High correlation of VAS pain scores after 2 and 6 weeks of treatment with VAS pain scores at 12 weeks in randomised controlled trials in rheumatoid arthritis and osteoarthritis: meta-analysis and implications". Arthritis Research & Therapy 18: 73. March 2016. doi:10.1186/s13075-016-0972-7. PMID 27036633.
- ↑ "American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee". Arthritis Care & Research 64 (4): 465–474. April 2012. doi:10.1002/acr.21596. PMID 22563589.
- ↑ 98.0 98.1 "Oral or transdermal opioids for osteoarthritis of the knee or hip". The Cochrane Database of Systematic Reviews 9 (9): CD003115. September 2014. doi:10.1002/14651858.CD003115.pub4. PMID 25229835.
- ↑ 99.0 99.1 "Tramadol for osteoarthritis". The Cochrane Database of Systematic Reviews 5 (5): CD005522. May 2019. doi:10.1002/14651858.CD005522.pub3. PMID 31132298.
- ↑ 100.0 100.1 "Doxycycline for osteoarthritis of the knee or hip". The Cochrane Database of Systematic Reviews 11: CD007323. November 2012. doi:10.1002/14651858.CD007323.pub3. PMID 23152242.
- ↑ "Effect of collagen supplementation on osteoarthritis symptoms: a meta-analysis of randomized placebo-controlled trials". International Orthopaedics 43 (3): 531–538. March 2019. doi:10.1007/s00264-018-4211-5. PMID 30368550.
- ↑ 102.0 102.1 102.2 102.3 102.4 102.5 102.6 "Evidence for the efficacy of complementary and alternative medicines in the management of osteoarthritis: a systematic review". Rheumatology 50 (5): 911–920. May 2011. doi:10.1093/rheumatology/keq379. PMID 21169345.
- ↑ "Evidence of effectiveness of herbal medicinal products in the treatment of arthritis. Part I: Osteoarthritis". Phytotherapy Research 23 (11): 1497–1515. November 2009. doi:10.1002/ptr.3007. PMID 19856319.
- ↑ "Topical therapy for osteoarthritis: clinical and pharmacologic perspectives". Postgraduate Medicine 121 (2): 139–147. March 2009. doi:10.3810/pgm.2009.03.1986. PMID 19332972.
- ↑ "Ultrasound Diagnostic and Therapeutic Injections of the Hip and Groin". Journal of the Belgian Society of Radiology 101 (Suppl 2): 6. December 2017. doi:10.5334/jbr-btr.1371. PMID 30498802.
Creative Commons Attribution 4.0 International License (CC-BY 4.0) - ↑ "Pharmacodynamics, efficacy, safety and administration of intra-articular therapies for knee osteoarthritis". Expert Opinion on Drug Metabolism & Toxicology 15 (12): 1021–1032. December 2019. doi:10.1080/17425255.2019.1691997. PMID 31709838.
- ↑ "How Effective Are Non-Operative Intra-Articular Treatments for Bone Marrow Lesions in Knee Osteoarthritis in Adults? A Systematic Review of Controlled Clinical Trials". Pharmaceuticals 15 (12): 1555. December 2022. doi:10.3390/ph15121555. PMID 36559005.
- ↑ "Corticosteroid injections for osteoarthritis of the knee: meta-analysis". BMJ 328 (7444): 869. April 2004. doi:10.1136/bmj.38039.573970.7C. PMID 15039276.
- ↑ "Intra-articular corticosteroid for knee osteoarthritis". The Cochrane Database of Systematic Reviews 2015 (10): CD005328. October 2015. doi:10.1002/14651858.CD005328.pub3. PMID 26490760.
- ↑ "The Effect of Intra-articular Corticosteroids on Articular Cartilage: A Systematic Review". Orthopaedic Journal of Sports Medicine 3 (5): 2325967115581163. May 2015. doi:10.1177/2325967115581163. PMID 26674652.
- ↑ "Effect of Intra-articular Triamcinolone vs Saline on Knee Cartilage Volume and Pain in Patients With Knee Osteoarthritis: A Randomized Clinical Trial". JAMA 317 (19): 1967–1975. May 2017. doi:10.1001/jama.2017.5283. PMID 28510679.
- ↑ "Intraocular Pressure Increases After Intraarticular Knee Injection With Triamcinolone but Not Hyaluronic Acid". Clinical Orthopaedics and Related Research 476 (7): 1420–1425. July 2018. doi:10.1007/s11999.0000000000000261. OCLC 01554937. PMID 29533245.
- ↑ 113.0 113.1 "Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis". Annals of Internal Medicine 157 (3): 180–191. August 2012. doi:10.7326/0003-4819-157-3-201208070-00473. PMID 22868835.
- ↑ "Viscosupplementation for Osteoarthritis of the Knee: A Systematic Review of the Evidence". The Journal of Bone and Joint Surgery. American Volume 97 (24): 2047–2060. December 2015. doi:10.2106/jbjs.n.00743. PMID 26677239.
- ↑ "Hyaluronic acid and other conservative treatment options for osteoarthritis of the ankle". The Cochrane Database of Systematic Reviews 2015 (10): CD010643. October 2015. doi:10.1002/14651858.CD010643.pub2. PMID 26475434. "It is unclear if there is a benefit or harm for HA as treatment for ankle OA".
- ↑ "The EANM guideline for radiosynoviorthesis". European Journal of Nuclear Medicine and Molecular Imaging 49 (2): 681–708. January 2022. doi:10.1007/s00259-021-05541-7. PMID 34671820.
- ↑ "The efficacy of platelet-rich plasma in the treatment of symptomatic knee osteoarthritis: a systematic review with quantitative synthesis". Arthroscopy 29 (12): 2037–2048. December 2013. doi:10.1016/j.arthro.2013.09.006. PMID 24286802.
- ↑ "Intraarticular Injections of Platelet-rich Plasma (PRP) in the Management of Knee Osteoarthritis". The Archives of Bone and Joint Surgery 1 (1): 5–8. September 2013. PMID 25207275.
- ↑ Goodwin, Jhon (8 November 2017). "The effectiveness of pulsed electromagnetic fields (PEMFs) for knee osteoarthritis". Almagia 2014 (4): CD010071. doi:10.1002/14651858.CD010071.pub3. PMID 24782334. PMC 6464921. https://almagia.com/pemfs-and-knee-osteoarthritis/.
- ↑ "Ankle Arthrodesis - a Review of Current Techniques and Results". Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca 87 (4): 225–236. 2020. doi:10.55095/achot2020/035. PMID 32940217.
- ↑ "Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review". Canadian Journal of Surgery. Journal Canadien de Chirurgie 51 (6): 428–436. December 2008. PMID 19057730.
- ↑ "Knee replacement". Lancet 379 (9823): 1331–1340. April 2012. doi:10.1016/S0140-6736(11)60752-6. PMID 22398175.
- ↑ "Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis". The Bone & Joint Journal 95-B (1): 115–121. January 2013. doi:10.1302/0301-620X.95B1.29835. PMID 23307684.
- ↑ "The cost-effectiveness of total joint arthroplasty: a systematic review of published literature". Best Practice & Research. Clinical Rheumatology 26 (5): 649–658. October 2012. doi:10.1016/j.berh.2012.07.013. PMID 23218429.
- ↑ "Impact of total knee replacement practice: cost effectiveness analysis of data from the Osteoarthritis Initiative". BMJ 356: j1131. March 2017. doi:10.1136/bmj.j1131. PMID 28351833.
- ↑ "Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis" (in en-US). The Journal of Bone and Joint Surgery. American Volume 97 (2): 156–168. January 2015. doi:10.2106/JBJS.M.00372. PMID 25609443.
- ↑ "Total hip or knee replacement for osteoarthritis: mid- and long-term quality of life". Arthritis Care & Research 62 (1): 54–62. January 2010. doi:10.1002/acr.20014. PMID 20191491.
- ↑ "Surgery for shoulder osteoarthritis". The Cochrane Database of Systematic Reviews (10): CD008089. October 2010. doi:10.1002/14651858.CD008089.pub2. PMID 20927773.
- ↑ "Osteochondral Autograft & Allograft". https://www.ortho.wustl.edu/content/patient-care/2894/services/sports-medicine/overview/knee/osteochondral-autograft-allograft.aspx.
- ↑ "Osteoarticular transplantation: recognizing expected postsurgical appearances and complications". Radiographics 35 (3): 780–792. 2015. doi:10.1148/rg.2015140070. PMID 25969934.
- ↑ "An educational review of cartilage repair: precepts & practice--myths & misconceptions--progress & prospects". Osteoarthritis and Cartilage 23 (3): 334–350. March 2015. doi:10.1016/j.joca.2014.12.011. PMID 25534362.
- ↑ "Autologous chondrocyte implantation in the knee: systematic review and economic evaluation". Health Technology Assessment 21 (6): 1–294. February 2017. doi:10.3310/hta21060. PMID 28244303.
- ↑ 133.0 133.1 133.2 "Cochrane in CORR®: Shoulder Replacement Surgery For Osteoarthritis And Rotator Cuff Tear Arthropathy". Clinical Orthopaedics and Related Research 478 (11): 2431–2433. November 2020. doi:10.1097/CORR.0000000000001523. PMID 33055541.
- ↑ 134.0 134.1 134.2 "Shoulder replacement surgery for osteoarthritis and rotator cuff tear arthropathy". The Cochrane Database of Systematic Reviews 2020 (4): CD012879. April 2020. doi:10.1002/14651858.CD012879.pub2. PMID 32315453.
- ↑ "Osteotomy for treating knee osteoarthritis". The Cochrane Database of Systematic Reviews 2014 (12): CD004019. December 2014. doi:10.1002/14651858.CD004019.pub4. PMID 25503775.
- ↑ 136.0 136.1 "Surgical interventions for symptomatic mild to moderate knee osteoarthritis". The Cochrane Database of Systematic Reviews 2019 (7): CD012128. July 2019. doi:10.1002/14651858.CD012128.pub2. PMID 31322289.
- ↑ "A systematic review of recommendations and guidelines for the management of osteoarthritis: The chronic osteoarthritis management initiative of the U.S. bone and joint initiative". Seminars in Arthritis and Rheumatism 43 (6): 701–712. June 2014. doi:10.1016/j.semarthrit.2013.11.012. PMID 24387819.
- ↑ "The role of arthroscopy in the management of knee osteoarthritis". Best Practice & Research. Clinical Rheumatology 28 (1): 143–156. February 2014. doi:10.1016/j.berh.2014.01.008. PMID 24792949.
- ↑ "Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms". BMJ 350: h2747. June 2015. doi:10.1136/bmj.h2747. PMID 26080045.
- ↑ "Difficulties with assessing the benefit of glucosamine sulphate as a treatment for osteoarthritis". International Journal of Evidence-Based Healthcare 10 (3): 222–226. September 2012. doi:10.1111/j.1744-1609.2012.00279.x. PMID 22925619.
- ↑ "Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis". BMJ 341: c4675. September 2010. doi:10.1136/bmj.c4675. PMID 20847017.
- ↑ "Efficacies of different preparations of glucosamine for the treatment of osteoarthritis: a meta-analysis of randomised, double-blind, placebo-controlled trials". International Journal of Clinical Practice 67 (6): 585–594. June 2013. doi:10.1111/ijcp.12115. PMID 23679910.
- ↑ Analgesics for Osteoarthritis: An Update of the 2006 Comparative Effectiveness Review (Report). Comparative Effectiveness Reviews. 38. Agency for Healthcare Research and Quality (AHRQ). Oct 2011. PMID 22091473. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0016485/.
- ↑ "Glucosamine and chondroitin sulfate". Rheumatic Disease Clinics of North America 37 (1): 103–118. February 2011. doi:10.1016/j.rdc.2010.11.007. PMID 21220090. "The best current evidence suggests that the effect of these supplements, alone or in combination, on OA pain, function, and radiographic change is marginal at best.".
- ↑ "Crystalline glucosamine sulfate in the management of knee osteoarthritis: efficacy, safety, and pharmacokinetic properties". Therapeutic Advances in Musculoskeletal Disease 4 (3): 167–180. June 2012. doi:10.1177/1759720X12437753. PMID 22850875.
- ↑ "Dietary supplements as disease-modifying treatments in osteoarthritis: a critical appraisal". P & T 39 (6): 436–452. June 2014. PMID 25050057.
- ↑ "OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines". Osteoarthritis and Cartilage 16 (2): 137–162. February 2008. doi:10.1016/j.joca.2007.12.013. PMID 18279766.
- ↑ 148.0 148.1 "Is there any scientific evidence for the use of glucosamine in the management of human osteoarthritis?". Arthritis Research & Therapy 14 (1): 201. January 2012. doi:10.1186/ar3657. PMID 22293240.
- ↑ "An algorithm recommendation for the management of knee osteoarthritis in Europe and internationally: a report from a task force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO)". Seminars in Arthritis and Rheumatism 44 (3): 253–263. December 2014. doi:10.1016/j.semarthrit.2014.05.014. PMID 24953861.
- ↑ "A review of evidence-based medicine for glucosamine and chondroitin sulfate use in knee osteoarthritis". Arthroscopy 25 (1): 86–94. January 2009. doi:10.1016/j.arthro.2008.07.020. PMID 19111223.
- ↑ "Chondroitin for osteoarthritis". The Cochrane Database of Systematic Reviews 1 (1): CD005614. January 2015. doi:10.1002/14651858.CD005614.pub2. PMID 25629804.
- ↑ 152.0 152.1 152.2 152.3 152.4 "Oral herbal therapies for treating osteoarthritis". The Cochrane Database of Systematic Reviews 2014 (5): CD002947. May 2014. doi:10.1002/14651858.CD002947.pub2. PMID 24848732.
- ↑ "Management of Osteoarthritis with Avocado/Soybean Unsaponifiables". Cartilage 6 (1): 30–44. January 2015. doi:10.1177/1947603514554992. PMID 25621100.
- ↑ "Piascledine". Haute Autorité de santé. 25 July 2013. http://www.has-sante.fr/portail/upload/docs/application/pdf/2013-07/piascledine_ct_9142.pdf.
- ↑ "Efficacy and Safety of Turmeric Extracts for the Treatment of Knee Osteoarthritis: a Systematic Review and Meta-analysis of Randomised Controlled Trials". Current Rheumatology Reports 23 (2): 11. January 2021. doi:10.1007/s11926-020-00975-8. PMID 33511486. https://figshare.com/articles/journal_contribution/22998386.
- ↑ "S-Adenosylmethionine for osteoarthritis of the knee or hip". The Cochrane Database of Systematic Reviews 2009 (4): CD007321. October 2009. doi:10.1002/14651858.CD007321.pub2. PMID 19821403.
- ↑ "Efficacy and safety of hydroxychloroquine in osteoarthritis: a systematic review and meta-analysis of randomized controlled trials". The Korean Journal of Internal Medicine 37 (1): 210–221. January 2022. doi:10.3904/kjim.2020.605. PMID 33882635.
- ↑ "Efficacy and safety of colchicine for the treatment of osteoarthritis: a systematic review and meta-analysis of intervention trials". Clinical Rheumatology 42 (3): 889–902. March 2023. doi:10.1007/s10067-022-06402-w. PMID 36224305.
- ↑ "Oral hyaluronan relieves knee pain: a review". Nutrition Journal 15: 11. January 2016. doi:10.1186/s12937-016-0128-2. PMID 26818459.
- ↑ "Vitamin D supplementation for the management of knee osteoarthritis: a systematic review of randomized controlled trials". Rheumatology International 37 (9): 1489–1498. September 2017. doi:10.1007/s00296-017-3719-0. PMID 28421358.
- ↑ "The Effects of Acupuncture on Chronic Knee Pain Due to Osteoarthritis: A Meta-Analysis". The Journal of Bone and Joint Surgery. American Volume 98 (18): 1578–1585. September 2016. doi:10.2106/jbjs.15.00620. PMID 27655986.
- ↑ "Acupuncture for peripheral joint osteoarthritis". The Cochrane Database of Systematic Reviews 2010 (1): CD001977. January 2010. doi:10.1002/14651858.CD001977.pub2. PMID 20091527.
- ↑ "Acupuncture for hip osteoarthritis". The Cochrane Database of Systematic Reviews 5 (5): CD013010. May 2018. doi:10.1002/14651858.CD013010. PMID 29729027.
- ↑ "Acupuncture analgesia: II. Clinical considerations". Anesthesia and Analgesia 106 (2): 611–21, table of contents. February 2008. doi:10.1213/ane.0b013e318160644d. PMID 18227323. http://www.mvclinic.es/wp-content/uploads/2008_Wang_Acupuncture-Analgesia_II_Clinical-Considerations.pdf.
- ↑ "Transcutaneous electrostimulation for osteoarthritis of the knee". The Cochrane Database of Systematic Reviews 2009 (4): CD002823. October 2009. doi:10.1002/14651858.CD002823.pub2. PMID 19821296.
- ↑ "Low level laser therapy (Classes I, II and III) for treating osteoarthritis". The Cochrane Database of Systematic Reviews (3): CD002046. 2004. doi:10.1002/14651858.CD002046.pub2. PMID 15266461. (Retracted, see doi:10.1002/14651858.cd002046.pub3. If this is an intentional citation to a retracted paper, please replace
{{Retracted}}with{{Retracted|intentional=yes}}.) - ↑ "Short-term efficacy of physical interventions in osteoarthritic knee pain. A systematic review and meta-analysis of randomised placebo-controlled trials". BMC Musculoskeletal Disorders 8 (1): 51. June 2007. doi:10.1186/1471-2474-8-51. PMID 17587446.
- ↑ "Balneotherapy for osteoarthritis". The Cochrane Database of Systematic Reviews (4): CD006864. October 2007. doi:10.1002/14651858.CD006864. PMID 17943920.
- ↑ 169.0 169.1 "Thermotherapy for treatment of osteoarthritis". The Cochrane Database of Systematic Reviews 2003 (4): CD004522. 2003. doi:10.1002/14651858.CD004522. PMID 14584019.
- ↑ "Therapeutic ultrasound for osteoarthritis of the knee or hip". The Cochrane Database of Systematic Reviews (1): CD003132. January 2010. doi:10.1002/14651858.CD003132.pub2. PMID 20091539.
- ↑ "Effects of therapeutic ultrasound for knee osteoarthritis: a systematic review and meta-analysis". Clinical Rehabilitation 33 (12): 1863–1875. December 2019. doi:10.1177/0269215519866494. PMID 31382781.
- ↑ "Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery--a systematic review and meta-analysis". Osteoarthritis and Cartilage 19 (12): 1381–1395. December 2011. doi:10.1016/j.joca.2011.09.001. PMID 21959097.
- ↑ "Electromagnetic fields for treating osteoarthritis". The Cochrane Database of Systematic Reviews (12): CD003523. December 2013. doi:10.1002/14651858.CD003523.pub2. PMID 24338431.
- ↑ "Viscosupplementation for the treatment of osteoarthritis of the knee". The Cochrane Database of Systematic Reviews 2006 (2): CD005321. April 2006. doi:10.1002/14651858.cd005321.pub2. PMID 16625635.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. https://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html.
- ↑ 176.0 176.1 176.2 "The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study". Annals of the Rheumatic Diseases 73 (7): 1323–1330. July 2014. doi:10.1136/annrheumdis-2013-204763. PMID 24553908.
- ↑ "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2163–2196. December 2012. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ "Table 9: Estimated prevalence of moderate and severe disability (millions) for leading disabling conditions by age, for high-income and low- and middle-income countries, 2004". The Global Burden of Disease: 2004 Update. Geneva: World Health Organization (WHO). 2008. p. 35. ISBN 978-9241563710. https://books.google.com/books?id=xrYYZ6Jcfv0C&pg=PA35.
- ↑ "Increasing burden of hip osteoarthritis in the Middle East and North Africa (MENA): an epidemiological analysis from 1990 to 2019". Archives of Orthopaedic and Trauma Surgery 143 (6): 3563–3573. June 2023. doi:10.1007/s00402-022-04582-3. PMID 36038782.
- ↑ "Burden of knee osteoarthritis in the Middle East and North Africa (MENA): an epidemiological analysis from 1990 to 2019". Archives of Orthopaedic and Trauma Surgery 143 (10): 6323–6333. April 2023. doi:10.1007/s00402-023-04852-8. PMID 37005934.
- ↑ "Burden of Hand Osteoarthritis in the Middle East and North Africa (MENA): An Epidemiological Analysis From 1990 to 2019". The Journal of Hand Surgery 48 (3): 245–256. March 2023. doi:10.1016/j.jhsa.2022.11.016. PMID 36710229.
- ↑ 182.0 182.1 "Arthritis-Related Statistics: Prevalence of Arthritis in the United States". U.S. Centers for Disease Control and Prevention (CDC). 9 November 2016. https://www.cdc.gov/arthritis/data_statistics/arthritis-related-stats.htm.
- ↑ "Understanding NSAIDs: from aspirin to COX-2". Clinical Cornerstone 3 (5): 50–60. 2001. doi:10.1016/S1098-3597(01)90069-9. PMID 11464731.
- ↑ Pfuntner A., Wier L.M., Stocks C. Most Frequent Conditions in U.S. Hospitals, 2011. HCUP Statistical Brief #162. September 2013. Agency for Healthcare Research and Quality, Rockville, Maryland."Most Frequent Conditions in U.S. Hospitals, 2011 #162". http://www.hcup-us.ahrq.gov/reports/statbriefs/sb162.jsp.
- ↑ "National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011". Rockville, Maryland: Agency for Healthcare Research and Quality. August 2013. http://hcup-us.ahrq.gov/reports/statbriefs/sb160.jsp.
- ↑ "Costs for Hospital Stays in the United States, 2011: Statistical Brief #168". Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet].. Rockville (MD): Agency for Healthcare Research and Quality (US) 2006 February. December 2013.
- ↑ "PEMFs and knee osteoarthritis - almagia" (in en-US). 8 November 2017. https://almagia.com/pemfs-and-knee-osteoarthritis/,%20https://almagia.com/pemfs-and-knee-osteoarthritis/.
- ↑ "Burden of osteoarthritis in India and its states, 1990-2019: findings from the Global Burden of disease study 2019". Osteoarthritis and Cartilage 30 (8): 1070–1078. August 2022. doi:10.1016/j.joca.2022.05.004. PMID 35598766.
- ↑ "Chapter 41: Nature cure yoga for osteoarthritis". Nature Cure for Common Diseases. New Delhi: Arya Publication. 2011. p. 368. ISBN 978-8189093747. https://books.google.com/books?id=PdwRBAAAQBAJ&pg=PA368.
- ↑ "Osteoarthritis or Osteoarthrosis: Commentary on Misuse of Terms". Reconstructive Review 7 (1). 17 April 2017. doi:10.15438/rr.7.1.178. ISSN 2331-2270.
- ↑ "Osteoarthritis in two marine mammals and 22 land mammals: learning from skeletal remains". Journal of Anatomy (Wiley) 231 (1): 140–155. July 2017. doi:10.1111/joa.12620. PMID 28542897.
- ↑ "Theropod Paleopathology: A Literature Survey". Mesozoic Vertebrate Life. Indiana University Press. 2001. pp. 337–363. ISBN 978-0253339072. https://books.google.com/books?id=mgc6CS4EUPsC&pg=PA337.
- ↑ Chemical Biology: Approaches to Drug Discovery and Development to Targeting Disease. John Wiley & Sons. 2012. p. 313. ISBN 978-1118437674. https://books.google.com/books?id=ezXLFlwfJycC&pg=PA313.
- ↑ "Evaluation of symptomatic slow-acting drugs in osteoarthritis using the GRADE system". BMC Musculoskeletal Disorders 9: 165. December 2008. doi:10.1186/1471-2474-9-165. PMID 19087296.
- ↑ "Gene therapy in osteoarthritis". Joint Bone Spine 67 (6): 570–571. 2000. doi:10.1016/s1297-319x(00)00215-3. PMID 11195326.
- ↑ "Regeneration of hyaline cartilage by cell-mediated gene therapy using transforming growth factor beta 1-producing fibroblasts". Human Gene Therapy 12 (14): 1805–1813. September 2001. doi:10.1089/104303401750476294. PMID 11560773.
- ↑ "Orthopedic cellular therapy: An overview with focus on clinical trials". World Journal of Orthopedics 6 (10): 754–761. November 2015. doi:10.5312/wjo.v6.i10.754. PMID 26601056.
- ↑ "Seoul revokes license for gene therapy drug Invossa". Yonhap News Agency. 28 May 2019. https://en.yna.co.kr/view/AEN20190528004400320.
- ↑ 199.0 199.1 "Korea OKs first cell gene therapy 'Invossa'". The Korea Herald. 12 July 2017. http://www.koreaherald.com/view.php?ud=20170712000766.
- ↑ "Dance between biology, mechanics, and structure: A systems-based approach to developing osteoarthritis prevention strategies". Journal of Orthopaedic Research 33 (7): 939–947. July 2015. doi:10.1002/jor.22817. PMID 25639920.
- ↑ "OARSI Clinical Trials Recommendations: Soluble biomarker assessments in clinical trials in osteoarthritis". Osteoarthritis and Cartilage 23 (5): 686–697. May 2015. doi:10.1016/j.joca.2015.03.002. PMID 25952342.
- ↑ "Magnetic resonance imaging and biochemical markers of cartilage disease" (in English). Cartilage Tissue and Knee Joint Biomechanics (1st ed.). Elsevier. 2023. pp. Chapter 10. ISBN 9780323905978. https://shop.elsevier.com/books/cartilage-tissue-and-knee-joint-biomechanics/nochehdehi/978-0-323-90597-8.
- ↑ "Imaging and Biochemical Markers for Osteoarthritis". Diagnostics 11 (7): 1205. July 2021. doi:10.3390/diagnostics11071205. PMID 34359288.
- ↑ "Biomarkers for osteoarthritis: Can they be used for risk assessment? A systematic review". Maturitas 82 (1): 36–49. September 2015. doi:10.1016/j.maturitas.2015.04.004. PMID 25963100.
- ↑ "What is the utility of biomarkers for assessing the pathophysiology of hip osteoarthritis? A systematic review". Clinical Orthopaedics and Related Research 473 (5): 1683–1701. May 2015. doi:10.1007/s11999-015-4148-6. PMID 25623593.
- ↑ "Review of Prospects of Biological Fluid Biomarkers in Osteoarthritis". International Journal of Molecular Sciences 18 (3): 601. March 2017. doi:10.3390/ijms18030601. PMID 28287489.
External links
| Classification | |
|---|---|
| External resources |
- "Osteoarthritis". MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/osteoarthritis.html.
 |