Biology:Glucose-6-phosphate translocase
Glucose-6-Phosphate Translocase is an enzyme that in humans is encoded by the SLC37A4 gene.[1][2] It consists of three subunits, each of which are vital components of the multi-enzyme Glucose-6-Phosphatase Complex (G6Pase). This important enzyme complex is located within the membrane of the endoplasmic reticulum, and catalyzes the terminal reactions in both glycogenolysis and gluconeogenesis.[3] The G6Pase complex is most abundant in liver tissue, but also present in kidney cells, small intestine, pancreatic islets and at a lower concentration in the gallbladder.[4][5] The G6Pase complex is highly involved in the regulation of homeostasis and blood glucose levels. Within this framework of glucose regulation, the translocase components are responsible for transporting the substrates and products across the endoplasmic reticulum membrane, resulting in the release of free glucose into the bloodstream.[3]
Structure
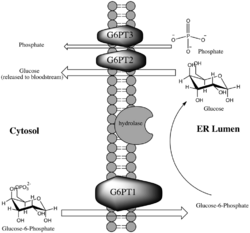
Glucose-6-Phosphate Translocase is a transmembrane protein providing a selective channel between the endoplasmic reticulum lumen and the cytosol. The enzyme is made up of three separate transporting subunits referred to as G6PT1 (subunit 1), G6PT2 (subunit 2) and G6PT3 (subunit 3). While the hydrolyzing component of the G6Pase complex is located on the side of the membrane on which it acts, namely facing the lumen, the translocases are all integral membrane proteins in order to perform their function as cross-membrane transporters. The translocases are spatially located on either side of the active site of the hydrolyzing component within the membrane, which allows the greatest speed and facility of the reaction.[6]
Mechanism
Each of the translocase subunits performs a specific function in the transport of substrates and products, and finally release of glucose (which will eventually reach the bloodstream), as a step in glycogenolysis or gluconeogenesis. G6PT1 transports Glucose-6-Phosphate from the cytosol into the lumen of the endoplasmic reticulum, where it is hydrolyzed by the catalytic subunit of G6Pase. After hydrolysis, glucose and inorganic phosphate are transported back into the cytosol by G6PT2 and G6PT3, respectively.[7] While the exact chemistry of the enzyme remains unknown, studies have shown that the mechanism of the enzyme complex is highly dependent upon the membrane structure. For instance, the Michaelis Constant of the enzyme for glucose-6-phosphate decreases significantly upon membrane disruption.[8] The originally proposed mechanism of the G6Pase system involved a relatively unspecific hydrolase, suggesting that G6PT1 alone provides the high specificity for the overall reaction by selective transport into the lumen, where hydrolysis occurs. Supporting evidence for this proposed reaction includes the marked decrease in substrate specificity of hydrolysis upon membrane degradation.[8]
Figure 1 illustrates the role of G6P-Translocase within the G6Pase complex.
Inhibitors
Many inhibitors of Glucose-6-Phosphate Translocase of novel, semi-synthetic or natural origin are known and of medical importance. Genetic algorithms for synthesizing novel inhibitors of G6PT1 have been developed and utilized in drug discovery.[9] Inhibitors of G6PT1 are the most studied as this subunit catalyzes the rate limiting step in glucose production through gluconeogenesis or glycogenolysis, and without its function these two processes could not occur. This inhibition holds great potential in drug development (discussed in "Medical and Disease Relevance"). Small-molecule inhibitors, such as mercaptopicolinic acid and diazobenzene sulfonate have some degree of inhibiting potential for G6PT1 but systematically lack specificity in inhibition, rendering them poor drug candidates.[10] Since the late 1990s, natural products have been increasingly studied as potent and specific inhibitors of G6PT1. Prominent examples of natural inhibitors include mumbaistatin and analogs, kodaistatin (harvested from extracts of Aspergillus terreus)[4] and chlorogenic acid.[11] Other natural product inhibitors of G6PT1 are found in the fungi Chaetomium carinthiacum, Bauhinia magalandra leaves, and streptomyces bacteria.[4][10]
Medical and disease relevance
1) Excessive activity of G6PT1 may contribute to the development of diabetes. Diabetes mellitus type 2 is a disease characterized by chronically elevated blood glucose levels, even when fasting.[12] The rapidly rising prevalence of type 2 diabetes, along with its strong correlation to heart disease and other health complications has rendered it an area of intense research with an urgent need for treatment options.[12] Studies monitoring blood glucose levels in rabbits revealed that the activity of G6Pase, and therefore G6PT1, is increased in specimens with diabetes.[citation needed] This strong correlation with diabetes type 2 makes the G6Pase complex, and G6PT1 in particular, an appealing drug target for control of blood glucose levels as its inhibition would directly prevent the release of free glucose into the bloodstream. It is possible that this mechanism of inhibition could be developed into a treatment for diabetes.[4]
2) The absence of a functional G6PT1 enzyme causes glycogen storage disease type Ib, commonly referred to as von Gierke disease, in humans. A common symptom of this disease is a build-up of glycogen in the liver and kidney causing enlargement of the organs.[11]
3) G6PT1 activity contributes to the survival of cells during hypoxia, which enables tumor cell growth and proliferation.[13]
References
- ↑ "The gene for glycogen-storage disease type 1b maps to chromosome 11q23". Am J Hum Genet 62 (2): 400–5. Apr 1998. doi:10.1086/301727. PMID 9463334.
- ↑ "Sequence of a putative glucose 6-phosphate translocase, mutated in glycogen storage disease type Ib". FEBS Lett 419 (2–3): 235–8. Jan 1998. doi:10.1016/S0014-5793(97)01463-4. PMID 9428641.
- ↑ 3.0 3.1 Parker JC, VanVolkenburg, MA (Oct 1998). "Plasma glucose levels are reduced in rats and mice treated with an inhibitor of glucose-6-phosphate translocase". Diabetes 47 (10): 1630–6. doi:10.2337/diabetes.47.10.1630. PMID 9753303.
- ↑ 4.0 4.1 4.2 4.3 Parker, JC (2004). "Glucose-6-phosphatase inhibitors". Drugs of the Future 29 (10): 1025–1033. doi:10.1358/dof.2004.029.10.863393.
- ↑ Hill, A (2004). "The microsomal glucose-6-phosphatase enzyme of human gall-bladder". J. Pathol. 158 (1): 53–6. doi:10.1002/path.1711580111. PMID 2547044.
- ↑ van Schaftigen, E; Gerin, I (Mar 2002). "The glucose 6 phosphatase system". Biochem. J. 362 (362, Pt3): 513–32. doi:10.1042/0264-6021:3620513. PMID 11879177.
- ↑ Parker, JC (2001). "Glucose-6-phosphate translocase as a target for the design of antidiabetic agents". Drugs of the Future 26 (7): 687–93. doi:10.1358/dof.2001.026.07.858712.
- ↑ 8.0 8.1 Arion, J (1975). "Involvement of a glucose 6-phosphate transport system in the function of microsomal glucose 6-phosphatase". Mol. Cell. Biochem. 6 (2): 75–83. doi:10.1007/BF01732001. PMID 235736.
- ↑ "Evolutionary chemistry approach toward finding novel inhibitors of the type 2 diabetes target glucose-6-phosphate translocase". J. Comb. Chem. 7 (2): 218–26. Mar–Apr 2005. doi:10.1021/cc049867+. PMID 15762749.
- ↑ 10.0 10.1 Taek Soon, L (Aug 2007). "Structure–activity relationships of semisynthetic mumbaistatin analogs". Bioorg. Med. Chem. 15 (15): 5207–18. doi:10.1016/j.bmc.2007.05.019. PMID 17524653.
- ↑ 11.0 11.1 Charkoudian, LK (April 2012). "Natural product inhibitors of glucose-6-phosphate translocase". Med. Chem. Commun. 3 (8): 926–31. doi:10.1039/C2MD20008B.
- ↑ 12.0 12.1 American Diabetes Association (Jan 2012). "Standards of Medical Care in Diabetes - 2012". Diabetes Care 35 (1): S11–S63. doi:10.2337/dc12-s011. PMID 22187469.
- ↑ Tahanian, E (May 2010). "Inhibition of Tubulogenesis and of Carcinogen-mediated Signaling in Brain Endothelial Cells Highlight the Antiangiogenic Properties of a Mumbaistatin Analog". Chemical Biology & Drug Design 75 (5): 481–8. doi:10.1111/j.1747-0285.2010.00961.x. PMID 20486934.
External links