Biology:Podocyte
| Podocyte | |
|---|---|
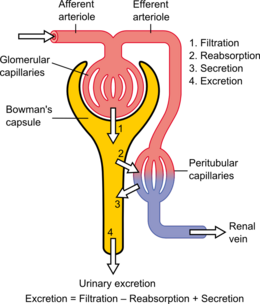
 Renal corpuscle structure
Blood flows in the afferent arteriole at the top, and out the efferent arteriole at the bottom. Blood flows through the capillaries of the glomerulus, where it is filtered by pressure. The podocytes (green) are wrapped around the capillaries. Blood is filtered through the slit diaphragm (or filtration slit), between the feet or processes of the podocytes. The filtered blood passes out the proximal tubule (yellow) on the right. | |
| Details | |
| Precursor | Intermediate mesoderm |
| Location | Bowman's capsule of the kidney |
| Identifiers | |
| Latin | podocytus |
| Anatomical terms of microanatomy | |
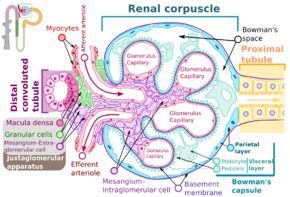
Podocytes are cells in Bowman's capsule in the kidneys that wrap around capillaries of the glomerulus. Podocytes make up the epithelial lining of Bowman's capsule, the third layer through which filtration of blood takes place.[1] Bowman's capsule filters the blood, retaining large molecules such as proteins while smaller molecules such as water, salts, and sugars are filtered as the first step in the formation of urine. Although various viscera have epithelial layers, the name visceral epithelial cells usually refers specifically to podocytes, which are specialized epithelial cells that reside in the visceral layer of the capsule.
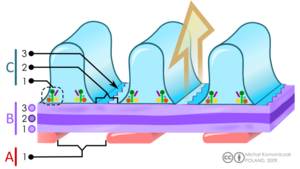
The podocytes have long foot processes called pedicels, for which the cells are named (podo- + -cyte). The pedicels wrap around the capillaries and leave slits between them. Blood is filtered through these slits, each known as a filtration slit, slit diaphragm, or slit pore.[2] Several proteins are required for the pedicels to wrap around the capillaries and function. When infants are born with certain defects in these proteins, such as nephrin and CD2AP, their kidneys cannot function. People have variations in these proteins, and some variations may predispose them to kidney failure later in life. Nephrin is a zipper-like protein that forms the slit diaphragm, with spaces between the teeth of the zipper big enough to allow sugar and water through but too small to allow proteins through. Nephrin defects are responsible for congenital kidney failure. CD2AP regulates the podocyte cytoskeleton and stabilizes the slit diaphragm.[3][4]
Structure
Podocytes are found lining the Bowman's capsules in the nephrons of the kidney. The foot processes known as pedicels that extend from the podocytes wrap themselves around the capillaries of the glomerulus to form the filtration slits. The pedicels increase the surface area of the cells enabling efficient ultrafiltration.[5]
Podocytes secrete and maintain the basement membrane.[2]
There are numerous coated vesicles and coated pits along the basolateral domain of the podocytes which indicate a high rate of vesicular traffic.
Podocytes possess a well-developed endoplasmic reticulum and a large Golgi apparatus, indicative of a high capacity for protein synthesis and post-translational modifications.
There is also growing evidence of a large number of multivesicular bodies and other lysosomal components seen in these cells, indicating a high endocytic activity.
Function
Podocytes have primary processes called trabeculae, which wrap around the glomerular capillaries.[6] The trabeculae in turn have secondary processes called pedicels.[6] Pedicels interdigitate, thereby giving rise to thin gaps called filtration slits.[2] The slits are covered by slit diaphragms which are composed of a number of cell-surface proteins including nephrin, podocalyxin, and P-cadherin, which restrict the passage of large macromolecules such as serum albumin and gamma globulin and ensure that they remain in the bloodstream.[7] Proteins that are required for the correct function of the slit diaphragm include nephrin,[8] NEPH1, NEPH2,[9] podocin, CD2AP.[10] and FAT1.[11]
Small molecules such as water, glucose, and ionic salts are able to pass through the filtration slits and form an ultrafiltrate in the tubular fluid, which is further processed by the nephron to produce urine.
Podocytes are also involved in regulation of glomerular filtration rate (GFR). When podocytes contract, they cause closure of filtration slits. This decreases the GFR by reducing the surface area available for filtration.
Clinical significance

A loss of the foot processes of the podocytes (i.e., podocyte effacement) is a hallmark of minimal change disease, which has therefore sometimes been called foot process disease.[13]
Disruption of the filtration slits or destruction of the podocytes can lead to massive proteinuria, where large amounts of protein are lost from the blood.
An example of this occurs in the congenital disorder Finnish-type nephrosis, which is characterised by neonatal proteinuria leading to end-stage kidney failure. This disease has been found to be caused by a mutation in the nephrin gene.
In 2002 Professor Moin Saleem at the University of Bristol made the first conditionally immortalised human podocyte cell line.[14][further explanation needed] This meant that podocytes could be grown and studied in the lab. Since then many discoveries have been made. Nephrotic syndrome occurs when there is a breakdown of the glomerular filtration barrier. The podocytes form one layer of the filtration barrier. Genetic mutations can cause podocyte dysfunction leading to an inability of the filtration barrier to restrict urinary protein loss. There are currently 53 genes known to play a role in genetic nephrotic syndrome.[15] In idiopathic nephrotic syndrome, there is no known genetic mutation. It is thought to be caused by a hitherto unknown circulating permeability factor.[16] Recent evidence suggests that the factor could be released by T-cells or B-cells,[17][18] podocyte cell lines can be treated with plasma from patients with nephrotic syndrome to understand the specific responses of the podocyte to the circulating factor. There is growing evidence that the circulating factor could be signalling to the podocyte via the PAR-1 receptor.[19][further explanation needed]
Presence of podocytes in urine has been proposed as an early diagnostic marker for preeclampsia.[20]
See also
- List of human cell types derived from the germ layers
- List of distinct cell types in the adult human body
References
- ↑ "Podocyte" at Dorland's Medical Dictionary
- ↑ 2.0 2.1 2.2 "Glomerular Filtration". Principles of Renal Physiology (5th ed.). New York: Springer Science+Business Media. 2012. p. 34. doi:10.1007/978-1-4614-3785-7_3. ISBN 978-1-4614-3784-0.
- ↑ "First components found for new kidney filter". Science 286 (5438): 225–226. October 1999. doi:10.1126/science.286.5438.225. PMID 10577188.
- ↑ "Molecular genetic analysis of podocyte genes in focal segmental glomerulosclerosis--a review". European Journal of Pediatrics 168 (11): 1291–1304. November 2009. doi:10.1007/s00431-009-1017-x. PMID 19562370.
- ↑ "Epithelium; Cell Types". Essentials of Human Physiology. http://humanphysiology.tuars.com/program/section7/7ch04/7ch04p08.htm.
- ↑ 6.0 6.1 (in en) Netter's Essential Histology E-Book. Elsevier Health Sciences. 28 February 2013. ISBN 978-1-4557-0307-4. https://books.google.com/books?id=mhy0BQAAQBAJ&q=podocyte+trabeculae&pg=PT380. Retrieved 2 June 2020.
- ↑ "Update on the glomerular filtration barrier". Current Opinion in Nephrology and Hypertension 18 (3): 226–232. May 2009. doi:10.1097/mnh.0b013e3283296044. PMID 19374010.
- ↑ "Nephrin strands contribute to a porous slit diaphragm scaffold as revealed by electron tomography". The Journal of Clinical Investigation 114 (10): 1475–1483. November 2004. doi:10.1172/JCI22562. PMID 15545998.
- ↑ "A model organism approach: defining the role of Neph proteins as regulators of neuron and kidney morphogenesis". Human Molecular Genetics 19 (12): 2347–2359. June 2010. doi:10.1093/hmg/ddq108. PMID 20233749.
- ↑ "Slit diaphragms contain tight junction proteins". Journal of the American Society of Nephrology 20 (7): 1491–1503. July 2009. doi:10.1681/ASN.2008101117. PMID 19478094.
- ↑ "Mice lacking the giant protocadherin mFAT1 exhibit renal slit junction abnormalities and a partially penetrant cyclopia and anophthalmia phenotype". Molecular and Cellular Biology 23 (10): 3575–3582. May 2003. doi:10.1128/mcb.23.10.3575-3582.2003. PMID 12724416.
- ↑ Cutrim ÉMM, Neves PDMM, Campos MAG, Wanderley DC, Teixeira-Júnior AAL, Muniz MPR (2022). "Collapsing Glomerulopathy: A Review by the Collapsing Brazilian Consortium.". Front Med (Lausanne) 9: 846173. doi:10.3389/fmed.2022.846173. PMID 35308512.
- CC-BY 4.0 license - ↑ "Minimal Change Disease". Clinical Journal of the American Society of Nephrology 12 (2): 332–345. February 2017. doi:10.2215/CJN.05000516. PMID 27940460.
- ↑ Saleem, Moin A.; O'Hare, Michael J.; Reiser, Jochen; Coward, Richard J.; Inward, Carol D.; Farren, Timothy; Xing, Chang Ying; Ni, Lan et al. (March 2002). "A conditionally immortalized human podocyte cell line demonstrating nephrin and podocin expression". Journal of the American Society of Nephrology 13 (3): 630–638. doi:10.1681/ASN.V133630. ISSN 1046-6673. PMID 11856766.
- ↑ Bierzynska, Agnieszka; McCarthy, Hugh J.; Soderquest, Katrina; Sen, Ethan S.; Colby, Elizabeth; Ding, Wen Y.; Nabhan, Marwa M.; Kerecuk, Larissa et al. (April 2017). "Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management". Kidney International 91 (4): 937–947. doi:10.1016/j.kint.2016.10.013. ISSN 1523-1755. PMID 28117080. https://pubmed.ncbi.nlm.nih.gov/28117080/.
- ↑ Maas, Rutger J.; Deegens, Jeroen K.; Wetzels, Jack F. (2014). "Permeability factors in idiopathic nephrotic syndrome: historical perspectives and lessons for the future". Nephrology Dialysis Transplantation (academic.oup.com) 29 (12): 2207–2216. doi:10.1093/ndt/gfu355. https://academic.oup.com/ndt/article/29/12/2207/1853198. Retrieved 2023-04-26.
- ↑ Hackl, Agnes; Zed, Seif El Din Abo; Diefenhardt, Paul; Binz-Lotter, Julia; Ehren, Rasmus; Weber, Lutz Thorsten (2021-11-18). "The role of the immune system in idiopathic nephrotic syndrome". Molecular and Cellular Pediatrics 8 (1): 18. doi:10.1186/s40348-021-00128-6. ISSN 2194-7791. PMID 34792685.
- ↑ May, Carl J.; Welsh, Gavin I.; Chesor, Musleeha; Lait, Phillipa J.; Schewitz-Bowers, Lauren P.; Lee, Richard W. J.; Saleem, Moin A. (2019-10-01). "Human Th17 cells produce a soluble mediator that increases podocyte motility via signaling pathways that mimic PAR-1 activation". American Journal of Physiology. Renal Physiology 317 (4): F913–F921. doi:10.1152/ajprenal.00093.2019. ISSN 1522-1466. PMID 31339775.
- ↑ May, Carl J.; Chesor, Musleeha; Hunter, Sarah E.; Hayes, Bryony; Barr, Rachel; Roberts, Tim; Barrington, Fern A.; Farmer, Louise et al. (March 2023). "Podocyte protease activated receptor 1 stimulation in mice produces focal segmental glomerulosclerosis mirroring human disease signaling events". Kidney International 104 (2): 265–278. doi:10.1016/j.kint.2023.02.031. ISSN 0085-2538. PMID 36940798.
- ↑ "Podocytes in urine, a novel biomarker of preeclampsia?". Advances in Clinical and Experimental Medicine 22 (2): 145–149. 2013. PMID 23709369. http://www.advances.am.wroc.pl/pdf/2013/22/2/145.pdf.
External links
- Anatomy photo: Urinary/mammal/vasc1/vasc1 - Comparative Organology at University of California, Davis - "Mammal, renal vasculature (EM, High)
- Histology image: 22401loa – Histology Learning System at Boston University - ". Ultrastructure of the Cell: podocytes and glomerular capillaries"
- UIUC Histology Subject 1400
- podocyte.ca[yes|permanent dead link|dead link}}] at Samuel Lunenfeld Research Institute
- Histology image: 22402loa – Histology Learning System at Boston University
- Histology image: 22403loa – Histology Learning System at Boston University
 |