Biology:Open flow microperfusion
Open flow microperfusion (OFM) is a sampling method for clinical and preclinical drug development studies and biomarker research. OFM is designed for continuous sampling of analytes from the interstitial fluid (ISF) of various tissues. It provides direct access to the ISF by insertion of a small, minimally invasive, membrane-free probe with macroscopic openings.[1] Thus, the entire biochemical information of the ISF becomes accessible regardless of the analyte's molecular size, protein-binding property or lipophilicity.[citation needed] OFM is capable of sampling lipophilic and hydrophilic compounds,[2] protein bound and unbound drugs,[3][4] neurotransmitters, peptides and proteins, antibodies,[5][6][7] nanoparticles and nanocarriers, enzymes and vesicles.
Method
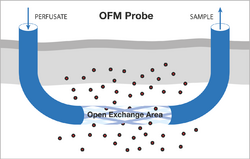
The OFM probes are perfused with a physiological solution (the perfusate) which equilibrates with the ISF of the surrounding tissue. Operating flow rates range from 0.1 to 10 μL/min. OFM allows unrestricted exchange of compounds via an open structure across the open exchange area of the probe. This exchange of compounds between the probe’s perfusate and the surrounding ISF is driven by convection and diffusion, and occurs non-selectively in either direction (Figure 1).
The direct liquid pathway between the probe’s perfusate and the surrounding fluid results in collection of ISF samples. These samples can be collected frequently and are then subjected to bioanalytical analysis to enable monitoring of substance concentrations with temporal resolution during the whole sampling period.[8][9]
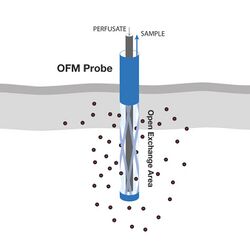
The concentric OFM probe (Figure 2) works according to the same principle. The perfusate is pumped to the tip of the OFM probe through the inner, thin lumen and exits beyond the Open Exchange Area, where it then mixes with exogenous substances present in the ISF before being withdrawn through the outer, thick lumen.[citation needed]
History
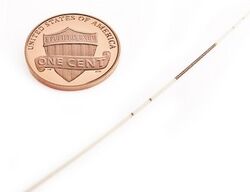
The first OFM sampling probe to be used as an alternative to microdialysis was described in an Austrian patent application filed by Falko Skrabal in 1987, where OFM was described as a device, which can be implanted into the tissue of living organisms.[10] In 1992, a US patent was filed claiming a device for determining at least one medical variable in the tissue of living organisms.[11] In a later patent by Helmut Masoner, Falko Skrabal and Helmut List a linear type of the sampling probe with macroscopic circular holes was also disclosed.[12] Alternative and current OFM versions for dermal and adipose tissue application were developed by Joanneum Research, and were patented by Manfred Bodenlenz et al.[13][14] Alternative materials featuring low absorption were used to enable manufacturing of probes with diameters of 0.55 mm and exchange areas of 15 mm in length. For cerebral application, special OFM probes were patented by Birngruber et al.[15] Additionally, a patent was filed to manage the fluid handling of the ISF by using a portable peristaltic pump with a flow range of 0.1 to 10 µL/min that enables operation of up to three probes per pump.[16]
OFM System
Two types of OFM probes are currently available: Linear OFM probes for implantation into superficial tissues such as skin (dermal OFM, dOFM) and subcutaneous adipose tissue (adipose OFM, aOFM) as well as concentric probes for implantation into various regions of the brain (cerebral OFM, cOFM).[citation needed]
Areas of application
OFM is routinely applied in pharmaceutical research in preclinical (e.g. mice, rats, pigs, primates) and in clinical studies in humans (Figure 3). OFM-related procedures such as probe insertions or prolonged sampling with numerous probes are well tolerated by the subjects.[1]
Dermal OFM (dOFM)
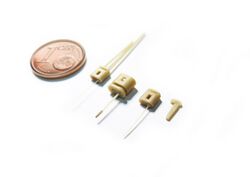
dOFM (Figure 4) allows the investigation of transport of drugs in the dermis and their penetration into the dermis after local, topical or systemic application, and dOFM is mentioned by the U.S. Food and Drug Administration as a new method for assessment of bioequivalence of topical drugs.[17][18][19]
dOFM is used for:
- conduct tissue-specific pharmacokinetic (PK) and pharmacodynamic (PD) studies of drugs.[20]
- perform head-to-head comparison of novel topical drug formulations
- assess dermal bioavailability.[9][1]
- investigate high molecular weight compounds, e.g. antibodies[5]
Head-to-head settings with OFM have proven particularly useful for the evaluation of topical generic products, which need to demonstrate bioequivalence[9] to the reference listed drug product to obtain market approval.
Applications of dOFM include ex vivo studies with tissue explants and preclinical and clinical in vivo studies.
Adipose OFM (aOFM)
aOFM (Figure 4) allows continuous on-line monitoring of metabolic processes in the subcutaneous adipose tissue, e.g. glucose and lactate,[21][22][23] as well as larger analytes such as insulin (5.9 kDa).[24][23] The role of polypeptides for metabolic signaling (leptin, cytokine IL-6, TNFα) has also been studied with aOFM.[25] aOFM allows the quantification of proteins (e.g. albumin size: 68 kDa) in adipose tissue[4] and thus opens up the possibility to investigate protein-bound drugs directly in peripheral target tissues, such as highly protein-bound insulin analogues designed for a prolonged, retarded insulin action.[26] Most recently, aOFM has been used to sample agonists to study obesity, lipid metabolism and immune-inflammation. Applications of aOFM include ex vivo studies with tissue explants and preclinical and clinical in vivo studies.[citation needed]
Cerebral OFM (cOFM)
cOFM (Figure 5) is used to conduct PK/PD preclinical studies in the animal brain. Access to the brain includes monitoring of the blood-brain barrier function and drug transport across the intact blood-brain barrier.[27] cOFM allows taking a look behind the blood-brain barrier and assesses concentrations and effects of neuroactive substances directly in the targeted brain tissue.[28]
The blood-brain barrier is a natural shield that protects the brain and limits the exchange of nutrients, metabolites and chemical messengers between blood and brain. The blood-brain barrier also prevents potential harmful substances from entering and damaging the brain. However, this highly effective barrier also prevents neuroactive substances from reaching appropriate targets. For researchers that develop neuroactive drugs, it is therefore of major interest to know whether and to what extent an active pharmaceutical component can pass the blood-brain barrier. Experiments have shown that the blood-brain barrier has fully reestablished 15 days after implantation of the cOFM probe in the brain of rats.[29] The cOFM probe has been specially designed to avoid a reopening of the blood-brain barrier or causing additional trauma to the brain after implantation. cOFM enables continuous sampling of cerebral ISF with intact blood-brain barrier cOFM and thus allows continuous PK monitoring in brain tissue.[citation needed]
Quantification of ISF compounds
ISF compounds can be quantified either indirectly from merely diluted ISF samples by using OFM and additional calibration techniques, or directly from undiluted ISF samples which can be collected with additional OFM methods. Quantification of compounds from diluted ISF samples requires additional application of calibration methods, such as Zero Flow Rate,[30] No Net Flux[31] or Ionic Reference.[32] Zero Flow Rate has been used in combination with dOFM by Schaupp et al.[3] to quantify potassium, sodium and glucose in adipose ISF samples. No Net Flux has been applied to quantify several analytes in OFM studies in subcutaneous adipose, muscle and dermal ISF: the absolute lactate concentrations[33] and the absolute glucose concentrations in adipose ISF,[3] the absolute albumin concentration in muscle ISF[4] and the absolute insulin concentration in adipose and muscle ISF have been successfully determined.[34] Dragatin et al.[5] used No Net Flux in combination with dOFM to assess the absolute ISF concentration of a fully human therapeutic antibody. Ionic Reference has been used in combination with OFM to assess the absolute glucose concentration[3] and the absolute lactate concentration in adipose ISF.[33] Dermal OFM has also been used to quantify the concentrations of human insulin and an insulin analogue in the ISF with inulin as exogenous marker.[citation needed]
Additional OFM methods, such as OFM recirculation and OFM suction can collect undiluted ISF samples from which direct and absolute quantification of compounds is feasible.[35] OFM recirculation to collect undiluted ISF samples recirculates the perfusate in a closed loop until equilibrium concentrations between perfusate and ISF are established. Using albumin as analyte, 20 recirculation cycles have been enough to reach equilibrium ISF concentrations. OFM suction is performed by applying a mild vacuum, which pulls ISF from the tissue into the OFM probe.[citation needed]
References
- ↑ 1.0 1.1 1.2 Bodenlenz, M.; Aigner, B.; Dragatin, C.; Liebenberger, L.; Zahiragic, S.; Höfferer, C.; Birngruber, T.; Priedl, J. et al. (April 2013). "Clinical applicability of dOFM devices for dermal sampling". Skin Research and Technology 19 (4): 474–483. doi:10.1111/srt.12071. PMID 23581539.
- ↑ Altendorfer-Kroath, Thomas; Schimek, Denise; Eberl, Anita; Rauter, Günther; Ratzer, Maria; Raml, Reingard; Sinner, Frank; Birngruber, Thomas (January 2019). "Comparison of cerebral Open Flow Microperfusion and Microdialysis when sampling small lipophilic and small hydrophilic substances". Journal of Neuroscience Methods 311: 394–401. doi:10.1016/j.jneumeth.2018.09.024. PMID 30266621.
- ↑ 3.0 3.1 3.2 3.3 Schaupp, L.; Ellmerer, M.; Brunner, G. A.; Wutte, A.; Sendlhofer, G.; Trajanoski, Z.; Skrabal, F.; Pieber, T. R. et al. (1 February 1999). "Direct access to interstitial fluid in adipose tissue in humans by use of open-flow microperfusion". American Journal of Physiology. Endocrinology and Metabolism 276 (2): E401–E408. doi:10.1152/ajpendo.1999.276.2.E401. PMID 9950802.
- ↑ 4.0 4.1 4.2 Ellmerer, Martin; Schaupp, Lukas; Brunner, Gernot A.; Sendlhofer, Gerald; Wutte, Andrea; Wach, Paul; Pieber, Thomas R. (1 February 2000). "Measurement of interstitial albumin in human skeletal muscle and adipose tissue by open-flow microperfusion". American Journal of Physiology. Endocrinology and Metabolism 278 (2): E352–E356. doi:10.1152/ajpendo.2000.278.2.E352. PMID 10662720.
- ↑ 5.0 5.1 5.2 Dragatin, Christian; Polus, Florine; Bodenlenz, Manfred; Calonder, Claudio; Aigner, Birgit; Tiffner, Katrin Irene; Mader, Julia Katharina; Ratzer, Maria et al. (February 2016). "Secukinumab distributes into dermal interstitial fluid of psoriasis patients as demonstrated by open flow microperfusion". Experimental Dermatology 25 (2): 157–159. doi:10.1111/exd.12863. PMID 26439798.
- ↑ Kolbinger, Frank; Loesche, Christian; Valentin, Marie-Anne; Jiang, Xiaoyu; Cheng, Yi; Jarvis, Philip; Peters, Thomas; Calonder, Claudio et al. (March 2017). "β-Defensin 2 is a responsive biomarker of IL-17A–driven skin pathology in patients with psoriasis". Journal of Allergy and Clinical Immunology 139 (3): 923–932.e8. doi:10.1016/j.jaci.2016.06.038. PMID 27502297.
- ↑ Kleinert, Maximilian; Kotzbeck, Petra; Altendorfer-Kroath, Thomas; Birngruber, Thomas; Tschöp, Matthias H.; Clemmensen, Christoffer (July 2018). "Time-resolved hypothalamic open flow micro-perfusion reveals normal leptin transport across the blood–brain barrier in leptin resistant mice". Molecular Metabolism 13: 77–82. doi:10.1016/j.molmet.2018.04.008. PMID 29748097.
- ↑ Bodenlenz, Manfred; Dragatin, Christian; Liebenberger, Lisa; Tschapeller, Bernd; Boulgaropoulos, Beate; Augustin, Thomas; Raml, Reingard; Gatschelhofer, Christina et al. (September 2016). "Kinetics of Clobetasol-17-Propionate in Psoriatic Lesional and Non-Lesional Skin Assessed by Dermal Open Flow Microperfusion with Time and Space Resolution". Pharmaceutical Research 33 (9): 2229–2238. doi:10.1007/s11095-016-1960-y. PMID 27271272.
- ↑ 9.0 9.1 9.2 Bodenlenz, Manfred; Tiffner, Katrin I.; Raml, Reingard; Augustin, Thomas; Dragatin, Christian; Birngruber, Thomas; Schimek, Denise; Schwagerle, Gerd et al. (January 2017). "Open Flow Microperfusion as a Dermal Pharmacokinetic Approach to Evaluate Topical Bioequivalence". Clinical Pharmacokinetics 56 (1): 91–98. doi:10.1007/s40262-016-0442-z. PMID 27539717. See also: Bodenlenz, Manfred; Tiffner, Katrin I.; Raml, Reingard; Augustin, Thomas; Dragatin, Christian; Birngruber, Thomas; Schimek, Denise; Schwagerle, Gerd et al. (January 2017). "Erratum to: Open Flow Microperfusion as a Dermal Pharmacokinetic Approach to Evaluate Topical Bioequivalence". Clinical Pharmacokinetics 56 (1): 99. doi:10.1007/s40262-016-0487-z. PMID 27873172.
- ↑ F. Skrabal, Vorrichtung zur Bestimmung zumindestens einer medizinischen Substanz in lebenden Organismen, AT391998B, 1987
- ↑ F. Skrabal, Process for determining parameters of interest in living organisms, 5,097,834, 1992.
- ↑ H. Marsoner, F. Skrabal, H. List, Device for determining at least one medical variable, 5,193,545, 1993.
- ↑ M. Bodenlenz, L. Schaupp, Catheter having an oblong slit, WO 2007/131780 A1, 2007.
- ↑ M. Bodenlenz, C. Hoefferer, T. Birngruber, L. Schaupp, Filament-based catheter, WO 2010/031515, 2010
- ↑ WO2012156478A1
- ↑ M. Bodenlenz, C. Hoefferer, T. Birngruber, R. Schaller, J. Priedl, F. Feichtner, S. Schock, P. Tkaczyk, and L. Schaupp, “Pump for medical applications” DE102011090210A1, 2011. EP;US;CA; 2011. Patent pending.
- ↑ A New Possible Way to Evaluate Bioequivalence of Topical Drugs. U.S. Food and Drug Administration. 25 June 2019.
- ↑ Center for Drug Evaluation and Research (22 September 2017). "Impact Story: Developing New Ways to Evaluate Bioequivalence for Topical Drugs". U.S. Food and Drug Administration. https://www.fda.gov/drugs/regulatory-science-action/impact-story-developing-new-ways-evaluate-bioequivalence-topical-drugs.
- ↑ Center for Drug Evaluation and Research (14 May 2021). "Topical Dermatological Products". FY2020 GDUFA Science and Research Report. pp. 122–126. https://www.fda.gov/media/146749/download#page=122.
- ↑ Bodenlenz, Manfred; Höfferer, Christian; Magnes, Christoph; Schaller-Ammann, Roland; Schaupp, Lukas; Feichtner, Franz; Ratzer, Maria; Pickl, Karin et al. (August 2012). "Dermal PK/PD of a lipophilic topical drug in psoriatic patients by continuous intradermal membrane-free sampling". European Journal of Pharmaceutics and Biopharmaceutics 81 (3): 635–641. doi:10.1016/j.ejpb.2012.04.009. PMID 22554768.
- ↑ Skrabal, F.; Trajanoski, Z.; Kontscheider, H.; Kotanko, P.; Wach, P. (1 January 1995). "Portable system for on-line continuous ex vivo monitoring of subcutaneous tissue glucose using open tissue perfusion". Medical and Biological Engineering and Computing 33 (1): 116–118. doi:10.1007/BF02522959. PMID 7616773.
- ↑ Ellmerer, M; Schaupp, L; Trajanoski, Z; Jobst, G; Moser, I; Urban, G; Skrabal, F; Wach, P (October 1998). "Continuous measurement of subcutaneous lactate concentration during exercise by combining open-flow microperfusion and thin-film lactate sensors". Biosensors and Bioelectronics 13 (9): 1007–1013. doi:10.1016/S0956-5663(98)00002-5. PMID 9839389.
- ↑ 23.0 23.1 Cline, Gary W.; Petersen, Kitt Falk; Krssak, Martin; Shen, Jun; Hundal, Ripudaman S.; Trajanoski, Zlatko; Inzucchi, Silvio; Dresner, Alan et al. (22 July 1999). "Impaired Glucose Transport as a Cause of Decreased Insulin-Stimulated Muscle Glycogen Synthesis in Type 2 Diabetes". New England Journal of Medicine 341 (4): 240–246. doi:10.1056/NEJM199907223410404. PMID 10413736.
- ↑ Cline, Gary W.; Jucker, Beat M.; Trajanoski, Zlatko; Rennings, Alexander J. M.; Shulman, Gerald I. (1 February 1998). "A novel 13 C NMR method to assess intracellular glucose concentration in muscle, in vivo". American Journal of Physiology. Endocrinology and Metabolism 274 (2): E381–E389. doi:10.1152/ajpendo.1998.274.2.E381. PMID 9486172.
- ↑ Orban, Zsolt; Remaley, Alan T.; Sampson, Maureen; Trajanoski, Zlatko; Chrousos, George P. (June 1999). "The Differential Effect of Food Intake and β-Adrenergic Stimulation on Adipose-Derived Hormones and Cytokines in Man". The Journal of Clinical Endocrinology & Metabolism 84 (6): 2126–2133. doi:10.1210/jcem.84.6.5747. PMID 10372721.
- ↑ Bodenlenz, M.; Ellmerer, M.; Schaupp, L.; Jacobsen, L. V.; Plank, J.; Brunner, G. A.; Wutte, A.; Aigner, B. et al. (December 2015). "Bioavailability of insulin detemir and human insulin at the level of peripheral interstitial fluid in humans, assessed by open-flow microperfusion". Diabetes, Obesity and Metabolism 17 (12): 1166–1172. doi:10.1111/dom.12551. PMID 26260082.
- ↑ Birngruber, Thomas; Sinner, Frank (June 2016). "Cerebral open flow microperfusion (cOFM) an innovative interface to brain tissue". Drug Discovery Today: Technologies 20: 19–25. doi:10.1016/j.ddtec.2016.07.003. PMID 27986219.
- ↑ Birngruber, Thomas; Raml, Reingard; Gladdines, Werner; Gatschelhofer, Christina; Gander, Edgar; Ghosh, Arijit; Kroath, Thomas; Gaillard, Pieter J. et al. (July 2014). "Enhanced Doxorubicin Delivery to the Brain Administered Through Glutathione PEGylated Liposomal Doxorubicin (2B3-101) as Compared with Generic Caelyx,®/Doxil®—A Cerebral Open Flow Microperfusion Pilot Study". Journal of Pharmaceutical Sciences 103 (7): 1945–1948. doi:10.1002/jps.23994. PMID 24801480.
- ↑ Birngruber, Thomas; Ghosh, Arijit; Perez-Yarza, Veronica; Kroath, Thomas; Ratzer, Maria; Pieber, Thomas R; Sinner, Frank (December 2013). "Cerebral open flow microperfusion: A new in vivo technique for continuous measurement of substance transport across the intact blood-brain barrier". Clinical and Experimental Pharmacology and Physiology 40 (12): 864–871. doi:10.1111/1440-1681.12174. PMID 24256164.
- ↑ Jacobson, I.; Sandberg, M.; Hamberger, A. (November 1985). "Mass transfer in brain dialysis devices—a new method for the estimation of extracellular amino acids concentration". Journal of Neuroscience Methods 15 (3): 263–268. doi:10.1016/0165-0270(85)90107-4. PMID 4094481.
- ↑ Lonnroth, P.; Jansson, P. A.; Smith, U. (1 August 1987). "A microdialysis method allowing characterization of intercellular water space in humans". American Journal of Physiology. Endocrinology and Metabolism 253 (2): E228–E231. doi:10.1152/ajpendo.1987.253.2.E228. PMID 3618773.
- ↑ Trajanoski, Z.; Brunner, G. A.; Schaupp, L.; Ellmerer, M.; Wach, P.; Pieber, T. R.; Kotanko, P.; Skrabal, F. (1 July 1997). "Open-Flow Microperfusion of Subcutaneous Adipose Tissue for On-Line Continuous Ex Vivo Measurement of Glucose Concentration". Diabetes Care 20 (7): 1114–1121. doi:10.2337/diacare.20.7.1114. PMID 9203447.
- ↑ 33.0 33.1 Ellmerer, M.; Schaupp, L.; Sendlhofer, G.; Wutte, A.; Brunner, G. A.; Trajanoski, Z.; Skrabal, F.; Wach, P. et al. (December 1998). "Lactate Metabolism of Subcutaneous Adipose Tissue Studied by Open Flow Microperfusion". The Journal of Clinical Endocrinology & Metabolism 83 (12): 4394–4401. doi:10.1210/jcem.83.12.5303. PMID 9851784.
- ↑ Bodenlenz, Manfred; Schaupp, Lukas A.; Druml, Tatjana; Sommer, Romana; Wutte, Andrea; Schaller, Helga C.; Sinner, Frank; Wach, Paul et al. (August 2005). "Measurement of interstitial insulin in human adipose and muscle tissue under moderate hyperinsulinemia by means of direct interstitial access". American Journal of Physiology. Endocrinology and Metabolism 289 (2): E296–E300. doi:10.1152/ajpendo.00431.2004. PMID 15769794.
- ↑ Hummer, Joanna; Schwingenschuh, Simon; Raml, Reingard; Boulgaropoulos, Beate; Schwagerle, Gerd; Augustin, Thomas; Sinner, Frank; Birngruber, Thomas (1 November 2020). "OFM-recirculation and OFM-suction: advanced in-vivo open flow microperfusion (OFM) methods for direct and absolute quantification of albumin in interstitial fluid". Biomedical Physics & Engineering Express 6 (6): 065031. doi:10.1088/2057-1976/abc3a7. PMID 33843658.
External links
 |