Biology:Diagnosis of autism
This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these template messages)
(Learn how and when to remove this template message) |
| It has been suggested that Diagnosis of Asperger syndrome be merged into this page. (Discuss) Proposed since July 2023. |
The diagnosis of autism is based on a person's reported and directly observed behavior.[1] There are no known biomarkers for autism spectrum conditions that allow for a conclusive diagnosis.[2]
In most cases, diagnostic criteria codified in the World Health Organization's International Classification of Diseases (ICD) or the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) are used. These reference manuals are regularly updated based on advances in research, systematic evaluation of clinical experience, and healthcare considerations. Currently, the DSM-5 published in 2013 and the ICD-10 that came into effect in 1994 are used, with the latter in the process of being replaced by the ICD-11 that came into effect in 2022 and is now implemented by healthcare systems across the world. Which autism spectrum diagnoses can be made and which criteria are used depends on the local healthcare system's regulations.
According to the DSM-5-TR (2022), in order to receive a diagnosis of autism spectrum disorder, one must present with "persistent deficits in social communication and social interaction" and "restricted, repetitive patterns of behavior, interests, or activities."[3] These behaviors must begin in early childhood and affect one's ability to perform everyday tasks. Furthermore, the symptoms must not be fully explainable by intellectual developmental disorder or global developmental delay.
Diagnostic process
There are several factors that make autism spectrum disorder difficult to diagnose. First off, there are no standardized imaging, molecular or genetic tests that can be used to diagnose ASD.[4] Additionally, there is a lot of variety in how ASD affects individuals. The behavioral manifestations of ASD depend on one's developmental stage, age of presentation, current support, and individual variability.[5][3] Lastly, there are multiple conditions that may present similarly to autism spectrum disorder, including intellectual disability, hearing impairment, a specific language impairment[6] such as Landau–Kleffner syndrome,[7] ADHD, anxiety disorder, and psychotic disorders.[8] Furthermore, the presence of autism can make it harder to diagnose coexisting psychiatric disorders such as depression.[9]
Ideally the diagnosis of ASD should be given by a team of clinicians (e.g. pediatricians, child psychiatrists, child neurologists) based on information provided from the affected individual, caregivers, other medical professionals and from direct observation.[10] Evaluation of a child or adult for autism spectrum disorder typically starts with a pediatrician or primary care physician taking a developmental history and performing a physical exam. If warranted, the physician may refer the individual to an ASD specialist who will observe and assess cognitive, communication, family, and other factors using standardized tools, and taking into account any associated medical conditions.[6] A pediatric neuropsychologist is often asked to assess behavior and cognitive skills, both to aid diagnosis and to help recommend educational interventions.[11] Further workup may be performed after someone is diagnosed with ASD. This may include a clinical genetics evaluation particularly when other symptoms already suggest a genetic cause.[12] Although up to 40% of ASD cases may be linked to genetic causes,[13] it is not currently recommended to perform complete genetic testing on every individual who is diagnosed with ASD. Consensus guidelines for genetic testing in patients with ASD in the US and UK are limited to high-resolution chromosome and fragile X testing.[12] Metabolic and neuroimaging tests are also not routinely performed for diagnosis of ASD.[12]
The age at which ASD is diagnosed varies. Sometimes ASD can be diagnosed as early as 18 months, however, diagnosis of ASD before the age of two years may not be reliable.[4] Diagnosis becomes increasingly stable over the first three years of life. For example, a one-year-old who meets diagnostic criteria for ASD is less likely than a three-year-old to continue to do so a few years later.[14] Additionally, age of diagnosis may depend on the severity of ASD, with more severe forms of ASD more likely to be diagnosed at an earlier age.[15] Issues with access to healthcare such as cost of appointments or delays in making appointments often lead to delays in the diagnosis of ASD.[16] In the UK the National Autism Plan for Children recommends at most 30 weeks from first concern to completed diagnosis and assessment, though few cases are handled that quickly in practice.[6] Lack of access to appropriate medical care, broadening diagnostic criteria and increased awareness surrounding ASD in recent years has resulted in an increased number of individuals receiving a diagnosis of ASD as adults. Diagnosis of ASD in adults poses unique challenges because it still relies on an accurate developmental history and because autistic adults sometimes learn coping strategies, known as "masking" or "camouflaging", which may make it more difficult to obtain a diagnosis.[17][18]
The presentation and diagnosis of autism spectrum disorder may vary based on sex and gender identity. Most studies that have investigated the impact of gender on presentation and diagnosis of autism spectrum disorder have not differentiated between the impact of sex versus gender.[19] There is some evidence that autistic women and girls tend to show less repetitive behavior and may engage in more camouflaging than autistic males.[20] Camouflaging may include making oneself perform normative facial expressions and eye contact.[21] Differences in behavioral presentation and gender-stereotypes may make it more challenging to diagnose autism spectrum disorder in a timely manner in females.[19][20] A notable percentage of autistic females may be misdiagnosed, diagnosed after a considerable delay, or not diagnosed at all.[20]
Considering the unique challenges in diagnosing ASD using behavioral and observational assessment, specific US practice parameters for its assessment were published by the American Academy of Neurology in the year 2000,[22] the American Academy of Child and Adolescent Psychiatry in 1999,[5] and a consensus panel with representation from various professional societies in 1999.[22] The practice parameters outlined by these societies include an initial screening of children by general practitioners (i.e., "Level 1 screening") and for children who fail the initial screening, a comprehensive diagnostic assessment by experienced clinicians (i.e. "Level 2 evaluation"). Furthermore, it has been suggested that assessments of children with suspected ASD be evaluated within a developmental framework, include multiple informants (e.g., parents and teachers) from diverse contexts (e.g., home and school), and employ a multidisciplinary team of professionals (e.g., clinical psychologists, neuropsychologists, and psychiatrists).[23]
(As of 2019), psychologists wait until a child showed initial evidence of ASD tendencies, then administer various psychological assessment tools to assess for ASD.[23] Among these measurements, the Autism Diagnostic Interview-Revised (ADI-R) and the Autism Diagnostic Observation Schedule (ADOS) are considered the "gold standards" for assessing autistic children.[24][25] The ADI-R is a semi-structured parent interview that probes for symptoms of autism by evaluating a child's current behavior and developmental history. The ADOS is a semi-structured interactive evaluation of ASD symptoms that is used to measure social and communication abilities by eliciting several opportunities for spontaneous behaviors (e.g., eye contact) in standardized context. Various other questionnaires (e.g., The Childhood Autism Rating Scale, Autism Treatment Evaluation Checklist) and tests of cognitive functioning (e.g., The Peabody Picture Vocabulary Test) are typically included in an ASD assessment battery. The diagnostic interview for social and communication disorders (DISCO) may also be used.[26]
Screening
About half of parents of children with ASD notice their child's atypical behaviors by age 18 months, and about four-fifths notice by age 24 months.[14] If a child does not meet any of the following milestones, it "is an absolute indication to proceed with further evaluations. Delay in referral for such testing may delay early diagnosis and treatment and affect the [child's] long-term outcome."[22]
- No response to name (or gazing with direct eye contact) by 6 months.[27]
- No babbling by 12 months.
- No gesturing (pointing, waving, etc.) by 12 months.
- No single words by 16 months.
- No two-word (spontaneous, not just echolalic) phrases by 24 months.
- Loss of any language or social skills, at any age.
The Japanese practice is to screen all children for ASD at 18 and 24 months, using autism-specific formal screening tests. In contrast, in the UK, children whose families or doctors recognize possible signs of autism are screened. It is not known which approach is more effective.[28][clarification needed] The UK National Screening Committee does not recommend universal ASD screening in young children. Their main concerns includes higher chances of misdiagnosis at younger ages and lack of evidence of effectiveness of early interventions.[29] There is no consensus between professional and expert bodies in the US on screening for autism in children younger than 3 years.[30]
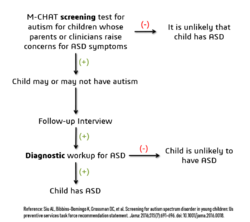
Screening tools include the Modified Checklist for Autism in Toddlers (M-CHAT), the Early Screening of Autistic Traits Questionnaire, and the First Year Inventory; initial data on M-CHAT and its predecessor, the Checklist for Autism in Toddlers (CHAT), on children aged 18–30 months suggests that it is best used in a clinical setting and that it has low sensitivity (many false-negatives) but good specificity (few false-positives).[14] It may be more accurate to precede these tests with a broadband screener that does not distinguish ASD from other developmental disorders.[31] Screening tools designed for one culture's norms for behaviors like eye contact may be inappropriate for a different culture.[32] Although genetic screening for autism is generally still impractical, it can be considered in some cases, such as children with neurological symptoms and dysmorphic features.[33]
Misdiagnosis
There is a significant level of misdiagnosis of autism in neurodevelopmentally typical children; 18–37% of children diagnosed with ASD eventually lose their diagnosis. This high rate of lost diagnosis cannot be accounted for by successful ASD treatment alone. The most common reason parents reported as the cause of lost ASD diagnosis was new information about the child (73.5%), such as a replacement diagnosis. Other reasons included a diagnosis given so the child could receive ASD treatment (24.2%), ASD treatment success or maturation (21%), and parents disagreeing with the initial diagnosis (1.9%).[34][non-primary source needed]
Many of the children who were later found not to meet ASD diagnosis criteria then received diagnosis for another developmental disorder. Most common was ADHD, but other diagnoses included sensory disorders, anxiety, personality disorder, or learning disability.[34][non-primary source needed] Neurodevelopment and psychiatric disorders that are commonly misdiagnosed as ASD include specific language impairment, social communication disorder, anxiety disorder, reactive attachment disorder, cognitive impairment, visual impairment, hearing loss and normal behavioral variation.[35] Some behavioral variations that resemble autistic traits are repetitive behaviors, sensitivity to change in daily routines, focused interests, and toe-walking. These are considered normal behavioral variations when they do not cause impaired function. Boys are more likely to exhibit repetitive behaviors especially when excited, tired, bored, or stressed. Some ways of distinguishing typical behavioral variations from autistic behaviors are the ability of the child to suppress these behaviors and the absence of these behaviors during sleep.[10]
See also
References
- ↑ "Diagnosis of autism". BMJ 327 (7413): 488–493. August 2003. doi:10.1136/bmj.327.7413.488. PMID 12946972.
- ↑ Lord, Catherine; Charman, Tony; Havdahl, Alexandra; Carbone, Paul; Anagnostou, Evdokia; Boyd, Brian; Carr, Themba; de Vries, Petrus J et al. (2022). "The Lancet Commission on the future of care and clinical research in autism" (in en). The Lancet 399 (10321): 271–334. doi:10.1016/S0140-6736(21)01541-5. PMID 34883054.
- ↑ 3.0 3.1 "Section 2: Neurodevelopmental Disorders". Diagnostic and statistical manual of mental disorders : DSM-5-TR (Print) (Fifth edition, text revision. ed.). Washington, DC: American Psychiatric Association Publishing. 2022. ISBN 978-0-89042-575-6.
- ↑ 4.0 4.1 CDC (31 March 2022). "Screening and Diagnosis | Autism Spectrum Disorder (ASD) | NCBDDD" (in en-us). https://www.cdc.gov/ncbddd/autism/screening.html.
- ↑ 5.0 5.1 "Practice parameters for the assessment and treatment of children, adolescents, and adults with autism and other pervasive developmental disorders. American Academy of Child and Adolescent Psychiatry Working Group on Quality Issues". Journal of the American Academy of Child and Adolescent Psychiatry 38 (12 Suppl): 32S–54S. December 1999. doi:10.1016/s0890-8567(99)80003-3. PMID 10624084.
- ↑ 6.0 6.1 6.2 "How to diagnose autism". Archives of Disease in Childhood 92 (6): 540–545. June 2007. doi:10.1136/adc.2005.086280. PMID 17515625.
- ↑ "Autistic regression and Landau-Kleffner syndrome: progress or confusion?". Developmental Medicine and Child Neurology 42 (5): 349–353. May 2000. doi:10.1017/S0012162200210621. PMID 10855658.
- ↑ "Diagnosis of autism spectrum disorder: reconciling the syndrome, its diverse origins, and variation in expression". The Lancet. Neurology 15 (3): 279–91. March 2016. doi:10.1016/s1474-4422(15)00151-9. PMID 26497771. https://kclpure.kcl.ac.uk/ws/files/49746512/Constantino_Charman_post_print_Lancet_Neurology.pdf.
- ↑ "Cormorbidity: diagnosing comorbid psychiatric conditions". Psychiatric Times 26 (4). 2009. http://www.psychiatrictimes.com/display/article/10168/1403043.
- ↑ 10.0 10.1 "When Autistic Behavior Suggests a Disease Other than Classic Autism". Pediatric Clinics of North America 64 (1): 127–138. February 2017. doi:10.1016/j.pcl.2016.08.009. PMID 27894440.
- ↑ "Diagnostic and assessment findings: a bridge to academic planning for children with autism spectrum disorders". Neuropsychology Review 18 (4): 367–384. December 2008. doi:10.1007/s11065-008-9072-z. PMID 18855144.
- ↑ 12.0 12.1 12.2 "Autism spectrum disorders: clinical and research frontiers". Archives of Disease in Childhood 93 (6): 518–523. June 2008. doi:10.1136/adc.2006.115337. PMID 18305076.
- ↑ "Genetics evaluation for the etiologic diagnosis of autism spectrum disorders". Genetics in Medicine 10 (1): 4–12. January 2008. doi:10.1097/GIM.0b013e31815efdd7. PMID 18197051.
- ↑ 14.0 14.1 14.2 "Diagnosis of autism spectrum disorders in the first 3 years of life". Nature Clinical Practice. Neurology 4 (3): 138–147. March 2008. doi:10.1038/ncpneuro0731. PMID 18253102.
- ↑ "Factors associated with age of diagnosis among children with autism spectrum disorders". Pediatrics 116 (6): 1480–1486. December 2005. doi:10.1542/peds.2005-0185. PMID 16322174.
- ↑ "Issues related to the diagnosis and treatment of autism spectrum disorders". Developmental Disabilities Research Reviews 13 (2): 129–135. 2007. doi:10.1002/mrdd.20143. PMID 17563895.
- ↑ "Diagnosis of autism in adulthood: A scoping review". Autism 24 (6): 1311–1327. August 2020. doi:10.1177/1362361320903128. PMID 32106698.
- ↑ "6A02 Autism spectrum disorder.". https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/437815624. "Some individuals with Autism Spectrum Disorder are capable of functioning adequately by making an exceptional effort to compensate for their symptoms during childhood, adolescence or adulthood. Such sustained effort, which may be more typical of affected females, can have a deleterious impact on mental health and well-being."
- ↑ 19.0 19.1 "Sex and gender impacts on the behavioural presentation and recognition of autism". Current Opinion in Psychiatry 33 (2): 117–123. March 2020. doi:10.1097/YCO.0000000000000575. PMID 31815760.
- ↑ 20.0 20.1 20.2 "Barriers to Autism Spectrum Disorder Diagnosis for Young Women and Girls: a Systematic Review". Review Journal of Autism and Developmental Disorders (Springer Science and Business Media LLC) 8 (4): 454–470. 29 October 2020. doi:10.1007/s40489-020-00225-8. PMID 34868805.
- ↑ ""Putting on My Best Normal": Social Camouflaging in Adults with Autism Spectrum Conditions". Journal of Autism and Developmental Disorders 47 (8): 2519–2534. August 2017. doi:10.1007/s10803-017-3166-5. PMID 28527095.
- ↑ 22.0 22.1 22.2 "Practice parameter: screening and diagnosis of autism: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society". Neurology 55 (4): 468–79. August 2000. doi:10.1212/wnl.55.4.468. PMID 10953176.
- ↑ 23.0 23.1 "Evidence-based assessment of autism spectrum disorders in children and adolescents". Journal of Clinical Child and Adolescent Psychology (Taylor & Francis) 34 (3): 523–40. September 2005. doi:10.1207/s15374424jccp3403_8. ISSN 1537-4416. PMID 16083393. http://webmedia.unmc.edu/mmi/mathews/4_Autism-%20evidence-based%20assessment.pdf. Retrieved 3 September 2019.
- ↑ "Between a ROC and a hard place: decision making and making decisions about using the SCQ". Journal of Child Psychology and Psychiatry, and Allied Disciplines 48 (9): 932–40. September 2007. doi:10.1111/j.1469-7610.2007.01762.x. ISSN 0021-9630. OCLC 01307942. PMID 17714378.
- ↑ "Diagnostic evaluation of autism spectrum disorders". Pediatric Clinics of North America 59 (1): 103–11, xi. February 2012. doi:10.1016/j.pcl.2011.10.018. PMID 22284796.
- ↑ "Autismespectrumstoornissen bij volwassenen" (in nl). Nederlands Tijdschrift voor Geneeskunde 152 (24): 1365–1369. June 2008. PMID 18664213.
- ↑ "Autism case training part 1: A closer look – key developmental milestones". CDC.gov. 18 August 2016. https://www.cdc.gov/ncbddd/actearly/autism/case-modules/early-warning-signs/03-closer-look.html#tabs-1-1.
- ↑ "Autism". Lancet 374 (9701): 1627–1638. November 2009. doi:10.1016/S0140-6736(09)61376-3. PMID 19819542. (Erratum: doi:10.1016/S0140-6736(11)61666-8, [1])
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedSiu 2016 - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedUS screening - ↑ "Validation of the Infant-Toddler Checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age". Autism 12 (5): 487–511. September 2008. doi:10.1177/1362361308094501. PMID 18805944.
- ↑ "The challenge of screening for autism spectrum disorder in a culturally diverse society". Acta Paediatrica 97 (5): 539–540. May 2008. doi:10.1111/j.1651-2227.2008.00720.x. PMID 18373717.
- ↑ "Autistic phenotypes and genetic testing: state-of-the-art for the clinical geneticist". Journal of Medical Genetics 46 (1): 1–8. January 2009. doi:10.1136/jmg.2008.060871. PMID 18728070.
- ↑ 34.0 34.1 Cite error: Invalid
<ref>tag; no text was provided for refs namedBlumberg 2016 - ↑ "Conditions That May Look Like Autism, but Aren't". WebMD. https://www.webmd.com/brain/autism/autism-similar-conditions.
 |