Medicine:Circadian rhythm sleep disorder
| Circadian rhythm sleep disorder | |
|---|---|
| Other names | Circadian rhythm sleep-wake disorders |
| Specialty | Psychiatry, neurology, chronobiology |
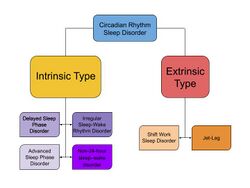
Circadian rhythm sleep disorders (CRSD), also known as circadian rhythm sleep-wake disorders (CRSWD), are a family of sleep disorders which affect the timing of sleep. CRSDs arise from a persistent pattern of sleep/wake disturbances that can be caused either by dysfunction in one's biological clock system, or by misalignment between one's endogenous oscillator and externally imposed cues. As a result of this mismatch, those affected by circadian rhythm sleep disorders have a tendency to fall asleep at unconventional time points in the day. These occurrences often lead to recurring instances of disturbed rest, where individuals affected by the disorder are unable to go to sleep and awaken at "normal" times for work, school, and other social obligations. Delayed sleep phase disorder, advanced sleep phase disorder, non-24-hour sleep–wake disorder and irregular sleep–wake rhythm disorder represents the four main types of CRSD.[1]
Overview
Humans, like most living organisms, have various biological rhythms. These biological clocks control processes that fluctuate daily (e.g., body temperature, alertness, hormone secretion), generating circadian rhythms. Among these physiological characteristics, the sleep-wake propensity can also be considered one of the daily rhythms regulated by the biological clock system. Human's sleeping cycles are tightly regulated by a series of circadian processes working in tandem, allowing for the experience of moments of consolidated sleep during the night and a long wakeful moment during the day. Conversely, disruptions to these processes and the communication pathways between them can lead to problems in sleeping patterns, which are collectively referred to as circadian rhythm sleep disorders.
Normal rhythm
A circadian rhythm is an entrainable, endogenous, biological activity that has a period of roughly twenty-four hours. This internal time-keeping mechanism is centralized in the suprachiasmatic nucleus (SCN) of humans, and allows for the internal physiological mechanisms underlying sleep and alertness to become synchronized to external environmental cues, like the light-dark cycle.[2] The SCN also sends signals to peripheral clocks in other organs, like the liver, to control processes such as glucose metabolism.[3] Although these rhythms will persist in constant light or dark conditions, different Zeitgebers (time givers such as the light-dark cycle) give context to the clock and allow it to entrain and regulate expression of physiological processes to adjust to the changing environment. Genes that help control light-induced entrainment include positive regulators BMAL1 and CLOCK and negative regulators PER1 and CRY.[4] A full circadian cycle can be described as a twenty-four hour circadian day, where circadian time zero (CT 0) marks the beginning of a subjective day for an organism and CT 12 marks the start of subjective night.[5]
Humans with regular circadian function have been shown to maintain regular sleep schedules, regulate daily rhythms in hormone secretion, and sustain oscillations in core body temperature.[6] Even in the absence of Zeitgebers, humans will continue to maintain a roughly 24-hour rhythm in these biological activities. Regarding sleep, normal circadian function allows people to maintain balance rest and wakefulness that allows people to work and maintain alertness during the day's activities, and rest at night.[7]
Some misconceptions regarding circadian rhythms and sleep commonly mislabel irregular sleep as a circadian rhythm sleep disorder. In order to be diagnosed with CRSD, there must be either a misalignment between the timing of the circadian oscillator and the surrounding environment, or failure in the clock entrainment pathway.[8] Among people with typical circadian clock function, there is variation in chronotypes, or preferred wake and sleep times, of individuals. Although chronotype varies from individual to individual, as determined by rhythmic expression of clock genes, people with typical circadian clock function will be able to entrain to environmental cues. For example, if a person wishes to shift the onset of a biological activity, like waking time, light exposure during the late subjective night or early subjective morning can help advance one's circadian cycle earlier in the day, leading to an earlier wake time.[9]
Diagnosis
The International Classification of Sleep Disorders classifies Circadian Rhythm Sleep Disorder as a type of sleep dyssomnia. Although studies suggest that 3% of the adult population has a CRSD, many people are often misdiagnosed with insomnia instead of a CRSD. Of adults diagnosed with sleep disorders, an estimated 10% have a CRSD and of adolescents with sleep disorders, an estimated 16% may have a CRSD.[10] Patients diagnosed with circadian rhythm sleep disorders typically express a pattern of disturbed sleep, whether that be excessive sleep that intrudes on working schedules and daily functions, or insomnia at desired times of sleep. Note that having a preference for extreme early or late wake times is not related to a circadian rhythm sleep disorder diagnosis. There must be distinct impairment of biological rhythms that affects the person's desired work and daily behavior. For a CRSD diagnosis, a sleep specialist gathers the history of a patient's sleep and wake habits, body temperature patterns, and dim-light melatonin onset (DLMO).[10] Gathering this data gives insight into the patient's current schedule, as well as the physiological phase markers of the patient's biological clock.[11]
The start of the CRSD diagnostic process is a thorough sleep history assessment. A standard questionnaire is used to record the sleep habits of the patient, including typical bedtime, sleep duration, sleep latency, and instances of waking up. The professional will further inquire about other external factors that may impact sleep. Prescription drugs that treat mood disorders like tricyclic antidepressants, selective serotonin reuptake inhibitors and other antidepressants are associated with abnormal sleep behaviors. Other daily habits like work schedule and timing of exercise are also recorded—because they may impact an individual's sleep and wake patterns. To measure sleep variables candidly, patients wear actigraphy watches that record sleep onset, wake time, and many other physiological variables. Patients are similarly asked to self-report their sleep habits with a week-long sleep diary to document when they go to bed, when they wake up, etc. to supplement the actigraphy data. Collecting this data allows sleep professionals to carefully document and measure patient's sleep habits and confirm patterns described in their sleep history.[10]
Other additional ways to classify the nature of a patient's sleep and biological clock are the morningness-eveningness questionnaire (MEQ) and the Munich ChronoType Questionnaire, both of which have fairly strong correlations with accurately reporting phase advanced or delayed sleep.[9] Questionnaires like the Pittsburgh Sleep Quality Index (PSQI) and the Insomnia Severity Index (ISI) help gauge the severity of sleep disruption. Specifically, these questionnaires can help the professional assess the patient's problems with sleep latency, undesired early-morning wakefulness, and problems with falling or staying asleep.[10] Tayside children's sleep questionnaire is a ten-item questionnaire for sleep disorders in children aged between one and five years old.[12][13][14]
Types
Currently, the International Classification of Sleep Disorders (ICSD-3) lists 6 disorders under the category of circadian rhythm sleep disorders.[15]
CRSDs can be categorized into two groups based on their underlying mechanisms: The first category is composed of disorders where the endogenous oscillator has been altered, known as intrinsic type disorders. The second category consists of disorders in which the external environment and the endogenous circadian clock are misaligned, called extrinsic type CRSDs.[16]
Intrinsic
- Delayed sleep phase disorder (DSPD): Individuals who have been diagnosed with delayed sleep phase disorder have sleep-wake times which are delayed when compared to normal functioning individuals. People with DSPD typically have very long periods of sleep latency when they attempt to go to sleep during conventional sleeping times. Similarly, they also have trouble waking up at conventional times.[17]
- Advanced sleep phase disorder (ASPD): People with advanced sleep phase disorder exhibit characteristics opposite to those with delayed sleep phase disorder. These individuals have advanced sleep wake times, so they tend to go to bed and wake up much earlier as compared to normal individuals. ASPD is less common than DSPD, and is most prevalent within older populations.[11]
- Familial Advanced Sleep Phase Syndrome (FASPS) is linked to an autosomal dominant mode of inheritance. It is associated with a missense mutation in human PER2 that replaces serine for glycine at position 662 (S662G).[18] Families that have this mutation in PER2 experience extreme phase advances in sleep, waking up around 2:00 a.m. and going to bed around 7:00 p.m.[citation needed]
- Irregular sleep–wake rhythm disorder (ISWRD) is characterized by a normal 24-hr sleeping period. However, individuals with this disorder experience fragmented and highly disorganized sleep that can manifest in the form of waking frequently during the night and taking naps during the day, yet still maintaining sufficient total time asleep. People with ISWRD often experience a range of symptoms from insomnia to excessive daytime sleepiness.[11]
- Non-24-hour sleep–wake disorder (N24SWD): Most common in individuals that are blind and unable to detect light, is characterized by chronic patterns of sleep/wake cycles which are not entrained to the 24-hr light-dark environmental cycle. As a result of this, individuals with this disorder will usually experience a gradual yet predictable delay of sleep onset and waking times. Patients with DSPD may develop this disorder if their condition is untreated.[11]
Extrinsic
- Shift work sleep disorder (SWSD): Approximately 9% of Americans who work night or irregular work shifts are believed to experience shift work sleep disorder.[19] Night shift work directly opposes the environmental cues that entrain our biological clock, so this disorder arises when an individual's clock is unable to adjust to the socially imposed work schedule. Shift work sleep disorder can lead to severe cases of insomnia as well as excessive daytime sleepiness.[20]
- Jet lag: Jet lag is best characterized by difficulty falling asleep or staying asleep as a result of misalignment between one's internal circadian system and external, or environmental cues. It is typically associated with rapid travel across multiple time zones.[15]
Alzheimer's disease
CRSD has been frequently associated with excessive daytime sleepiness and nighttime insomnia in patients diagnosed with Alzheimer's disease (AD), representing a common characteristic among AD patients as well as a risk factor of progressive functional impairments.[21][22][23] On one hand, it has been stated that people with AD have melatonin alteration and high irregularity in their circadian rhythm that lead to a disrupted sleep-wake cycle, probably due to damage on hypothalamic SCN regions typically observed in AD.[22][23] On the other hand, disturbed sleep and wakefulness states have been related to worsening of an AD patient's cognitive abilities, emotional state and quality of life.[21][22][23] Moreover, the abnormal behavioural symptoms of the disease negatively contribute to overwhelming patient's relatives and caregivers as well.[21][22]
However, the impact of sleep-wake disturbances on the subjective experience of a person with AD is not yet fully understood.[22] Therefore, further studies exploring this field have been highly recommended, mainly considering the increasing life expectancy and significance of neurodegenerative diseases in clinical practices.[23]
Treatment
Possible treatments for circadian rhythm sleep disorders include:
- Chronotherapy, best shown to effectively treat delayed sleep phase disorder, acts by systematically delaying an individual's bedtime until their sleep-wake times coincide with the conventional 24-hr day.[24]
- Light therapy utilizes bright light exposure to induce phase advances and delays in sleep and wake times. This therapy requires 30–60 minutes of exposure to a bright (5,000–10,000 lux) white, blue, or natural light at a set time until the circadian clock is aligned with the desired schedule.[8][25] Treatment is initially administered either upon awakening or before sleeping, and if successful may be continued indefinitely or performed less frequently.[26] Though proven very effective in the treatment of individuals with DSPD and ASPD, the benefits of light therapy on N24SWD, shift work disorder, and jet lag have not been studied as extensively.
- Hypnotics have also been used clinically alongside bright light exposure therapy and pharmacotherapy for the treatment of CRSDs such as Advanced Sleep Phase Disorder.[27] Additionally, in conjunction with cognitive behavioral therapy, short-acting hypnotics also present an avenue for treating co-morbid insomnia in patients with circadian sleep disorders.[28]
- Melatonin, a naturally occurring biological hormone with circadian rhythmicity, has been shown to promote sleep and entrainment to external cues when administered in drug form (0.5–5.0 mg). Melatonin administered in the evening causes phase advances in sleep-wake times while maintaining duration and quality of sleep. Similarly, when administered in the early morning, melatonin can cause phase delays. It has been shown most effective in cases of shift work sleep disorder and delayed phase sleep disorder, but has not been proven particularly useful in cases of jet lag.[25]
- Dark therapy, for example, the use of blue-blocking goggles, is used to block blue and blue-green wavelength light from reaching the eye during evening hours so as not to hinder melatonin production.[29]
See also
- Chronobiology
- Familial sleep traits
- Light effects on circadian rhythm
- Phase response curve
- Sleep diary
- Sleep medicine
References
- ↑ Dagan, Yaron (2002). "Circadian Rhythm Sleep Disorders (CRSD) in psychiatry--a review". The Israel Journal of Psychiatry and Related Sciences 39 (1): 19–27. ISSN 0333-7308. PMID 12013706. https://pubmed.ncbi.nlm.nih.gov/12013706/.
- ↑ "Basic science review on circadian rhythm biology and circadian sleep disorders". Annals of the Academy of Medicine, Singapore 37 (8): 662–8. August 2008. doi:10.47102/annals-acadmedsg.V37N8p662. PMID 18797559.
- ↑ "The mammalian circadian timing system: organization and coordination of central and peripheral clocks". Annual Review of Physiology 72 (1): 517–49. 2010-03-17. doi:10.1146/annurev-physiol-021909-135821. PMID 20148687. http://doc.rero.ch/record/17505/files/alb_mct.pdf.
- ↑ "Molecular bases for circadian clocks". Cell 96 (2): 271–90. January 1999. doi:10.1016/s0092-8674(00)80566-8. PMID 9988221.
- ↑ "Overview of circadian rhythms". Alcohol Research & Health 25 (2): 85–93. December 2001. PMID 11584554.
- ↑ "Circadian Rhythm, Lifestyle and Health: A Narrative Review". Iranian Journal of Public Health 47 (8): 1068–1076. August 2018. PMID 30186777.
- ↑ "Body Clock & Sleep - National Sleep Foundation". https://www.sleepfoundation.org/articles/sleep-drive-and-your-body-clock.
- ↑ Jump up to: 8.0 8.1 "Therapeutics for Circadian Rhythm Sleep Disorders". Sleep Medicine Clinics 5 (4): 701–715. December 2010. doi:10.1016/j.jsmc.2010.08.001. PMID 21243069.
- ↑ Jump up to: 9.0 9.1 "Circadian rhythm sleep disorders". Neurologic Clinics 30 (4): 1167–91. November 2012. doi:10.1016/j.ncl.2012.08.011. PMID 23099133.
- ↑ Jump up to: 10.0 10.1 10.2 10.3 "Circadian Rhythm Sleep Disorders". Journal of Clinical Outcomes Management 20 (11): 513–528. November 2013. PMID 25368503.
- ↑ Jump up to: 11.0 11.1 11.2 11.3 Dagan, Yaron; Borodkin, Katy MA (December 2005). "Behavioral and psychiatric consequences of sleep-wake schedule disorders". Dialogues in Clinical Neuroscience 7 (4): 357–365. doi:10.31887/DCNS.2005.7.4/ydagan. PMID 16416711.
- ↑ McGreavey, J. A.; Donnan, P. T.; Pagliari, H. C.; Sullivan, F. M. (September 2005). "The Tayside children's sleep questionnaire: a simple tool to evaluate sleep problems in young children". Child: Care, Health and Development 31 (5): 539–544. doi:10.1111/j.1365-2214.2005.00548.x. ISSN 0305-1862. PMID 16101649. https://pubmed.ncbi.nlm.nih.gov/16101649/.
- ↑ "Tayside Children's Sleep Questionnaire (TCSQ)". https://www.thoracic.org/members/assemblies/assemblies/srn/questionaires/tcsq.php.
- ↑ Rajaee Rizi, Farid; Asgarian, Fatemeh Sadat (2022-08-24). "Reliability, validity, and psychometric properties of the Persian version of the Tayside children's sleep questionnaire" (in en). Sleep and Biological Rhythms 21: 97–103. doi:10.1007/s41105-022-00420-6. ISSN 1479-8425. https://doi.org/10.1007/s41105-022-00420-6.
- ↑ Jump up to: 15.0 15.1 "International classification of sleep disorders-third edition: highlights and modifications". Chest 146 (5): 1387–1394. November 2014. doi:10.1378/chest.14-0970. PMID 25367475.
- ↑ Zhu, Lirong; Zee, Phyllis C. (November 2012). "Circadian Rhythm Sleep Disorders". Neurologic Clinics 30 (4): 1167–1191. doi:10.1016/j.ncl.2012.08.011. PMID 23099133. PMC 3523094. https://www.lecturio.com/concepts/circadian-rhythm-sleep-wake-disorder/. Retrieved June 24, 2021.
- ↑ "Circadian Rhythm Sleep–Wake Disorder". https://www.lecturio.com/concepts/circadian-rhythm-sleep-wake-disorder/.
- ↑ "Genetic basis of human circadian rhythm disorders". Experimental Neurology 243: 28–33. May 2013. doi:10.1016/j.expneurol.2012.07.012. PMID 22849821.
- ↑ "Shift work disorder in a random population sample--prevalence and comorbidities". PLOS ONE 8 (1): e55306. 2013-01-25. doi:10.1371/journal.pone.0055306. PMID 23372847. Bibcode: 2013PLoSO...855306D.
- ↑ "Circadian Rhythm Sleep–Wake Disorder". https://www.lecturio.com/concepts/circadian-rhythm-sleep-wake-disorder/.
- ↑ Jump up to: 21.0 21.1 21.2 Malkani, R., & Attarian, H. (2015). Sleep in Neurodegenerative Disorders. Current Sleep Medicine Reports, 1(2), 81-90.
- ↑ Jump up to: 22.0 22.1 22.2 22.3 22.4 Dick-Muehlke, C. (2015). Psychosocial studies of the individual's changing perspectives in Alzheimer's disease (Premier Reference Source). Hershey, PA: Medical Information Science Reference.
- ↑ Jump up to: 23.0 23.1 23.2 23.3 Zhong G, Naismith SL, Rogers NL, Lewis SJG (2011). "Sleep–wake disturbances in common neurodegenerative diseases: A closer look at selected aspects of the neural circuitry". Journal of the Neurological Sciences 307 (1–2): 9–14. doi:10.1016/j.jns.2011.04.020. PMID 21570695.
- ↑ "Behavioral Treatment of Circadian Rhythm Disorder" (in en). https://www.webmd.com/sleep-disorders/behavioral-treatment-circadian-rhythm-disorders.
- ↑ Jump up to: 25.0 25.1 "Circadian rhythm sleep disorders (CRSD)". Sleep Medicine Reviews 6 (1): 45–54. February 2002. doi:10.1053/smrv.2001.0190. PMID 12531141.
- ↑ "Light treatment for sleep disorders: consensus report. II. Basic properties of circadian physiology and sleep regulation". Journal of Biological Rhythms 10 (2): 113–25. June 1995. doi:10.1177/074873049501000204. PMID 7632985.
- ↑ "A clinical approach to circadian rhythm sleep disorders". Sleep Medicine 8 (6): 566–77. September 2007. doi:10.1016/j.sleep.2006.11.017. PMID 17395535.
- ↑ "Dorlands Medical Dictionary:hypnotic". http://www.mercksource.com/pp/us/cns/cns_hl_dorlands_split.jsp?pg=/ppdocs/us/common/dorlands/dorland/four/000051451.htm.
- ↑ "Blue light has a dark side". Harvard Health Letter. May 2012. http://www.health.harvard.edu/newsletters/Harvard_Health_Letter/2012/May/blue-light-has-a-dark-side/.
External links
- Circadian Sleep Disorders Network
- An American Academy of Sleep Medicine Review: Circadian Rhythm Sleep Disorders: Part I, Basic Principles, Shift Work and Jet Lag Disorders. PDF, 24 pages. November 2007.
- An American Academy of Sleep Medicine Review: Circadian Rhythm Sleep Disorders: Part II, Advanced Sleep Phase Disorder, Delayed Sleep Phase Disorder, Free-Running Disorder, and Irregular Sleep–Wake Rhythm. PDF, 18 pages. November 2007.
- An American Academy of Sleep Medicine Report: Practice Parameters for the Clinical Evaluation and Treatment of Circadian Rhythm Sleep Disorders, November 1, 2007
- NASA Sleep–Wake Actigraphy and Light Exposure During Spaceflight-Long Experiment
 |