Medicine:Cyclic neutropenia
| Cyclic neutropenia | |
|---|---|
| Other names | Periodic neutropenia, cyclic leucopenia, cyclic hematopoesis |
 | |
| Blood film with a striking absence of neutrophils, leaving only red blood cells and platelets. | |
| Symptoms | Fever, malaise, inflammation and infection of oral mucosa, respiratory tract, digestive tract, skin, and abdominal pain[1] |
| Usual onset | Infancy[1] |
| Causes | Mutation in ELANE gene[1] |
| Diagnostic method | Blood test, genetic testing[1] |
| Treatment | G-CSF[1] |
| Medication | Filgrastim[1] |
| Frequency | 1 in million (2018)[1] |
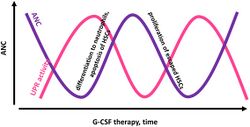
Cyclic neutropenia (CyN) is a rare hematologic disorder and form of congenital neutropenia that tends to occur approximately every three weeks and lasting for few days at a time due to changing rates of neutrophil production by the bone marrow. It causes a temporary condition with a low absolute neutrophil count and because the neutrophils make up the majority of circulating white blood cells it places the body at severe risk of inflammation and infection. In comparison to severe congenital neutropenia, it responds well to treatment with granulocyte colony-stimulating factor (filgrastim), which increases the neutrophil count, shortens the cycle length, as well decreases the severity and frequency of infections.
Signs and symptoms
The common symptoms of neutropenia are recurrent fever, malaise, inflammation of the tissues surrounding the teeth, mouth ulcers, inflammation and bacterial infection of the respiratory tract, digestive tract, skin, and abdominal pain.[1][2] It is considered that the greatest risk for death is from developing necrotizing enterocolitis (NEC), peritonitis, bacteremia or Clostridium and Escherichia coli sepsis and septic shock, and pneumonia.[1][3][4]
Causes
Cyclic neutropenia (CyN), like severe congenital neutropenia (SCN), is a rare disorder. It is considered that in the general population, CyN has a frequency of one in one million.[1] It is the result of autosomal dominant mutation in ELANE gene located on the short arm (p) of chromosome 19 (19p13.3), the gene encoding neutrophil elastase, which is also the most common cause of the SCN.[1][5][6][7] It sporadically occurs as a de novo mutation variant or can be present among members of the same family.[1] In the case of CyN, the mutation variants have been found to mostly cluster in intron 4 and exon 4 and 5,[6][3] but were also located in intron 3, and exon 2 and 3.[8][9][10][11][12] Some mutation variants have been found in both Cyn and SCN, which indicates they are phenotypes of the same disease with different severity.[9]
It is considered that the mutation causes a decrease in the "neutrophil production or excessive apoptosis (shorter half-life)" which results in a deficiency of mature neutrophils in the blood.[13] The exact pathological mechanism is still researched, with the main hypotheses being mislocalization of ELANE or unfolded protein response (UPR) induced by mutant ELANE,[14] however according to Mehta et al. (2016), the "UPR induction by mutant ELANE is not strong enough to promote cell death and that mutant ELANE causes SCN through an alternative mechanism".[15] According to Garg et al. (2020), new "findings challenge the currently prevailing model that SCN results from mutant ELANE, which triggers endoplasmic reticulum stress, UPR, and apoptosis".[16] The expression of the ELANE gene has been linked to GFI1 gene,[8][17] and some considered that interaction with other genes causes the emergence and severity of one or the other phenotypic disorder.[9] It is unclear what causes the cyclic aspect in CyN.[17] According to Donadieu et al. (2011), the "cyclic aspect ... suggests the existence of a cryptic biological clock that regulates granulopoiesis. This putative clock might be revealed by particular mutations".[13] Michael Mackey "postulates that the production of neutrophils is governed by long‐range stimulatory factors in a long feedback loop that has a built‐in time delay in the maturation of promyelocytes to fully differentiated neutrophils".[18] It is also not clear what causes that the levels of secretory leucocyte protease inhibitor (SLPI), which influences the induction of the unfolded protein response (UPR), are not diminished and as such activation of UPR is absent in CyN compared to SCN, in other words, different ELANE mutations "have different effects on UPR activation, and SLPI regulates the extent of ELANE‐triggered UPR".[19]
A 2020 study published in Annals of the New York Academy of Sciences about the pathomechanism of CyN revealed that "some HSPCs escape the UPR‐induced endoplasmic reticulum (ER) stress and proliferate in response to granulocyte colony‐stimulating factor (G‐CSF) to a certain threshold at which UPR again affects the majority of HSPCs. There is a cyclic balance between ER stress-induced apoptosis of HSPCs and compensatory G‐CSF–stimulated HSPC proliferation followed by granulocytic differentiation"; in other words, CyN is "characterized by cycling UPR activities and cycling UPR‐escaping cells". Also, the most probable reason that from the same mutation variant develops SCN and not CyN is due to more severe damage caused by UPR stress in SCN.[18]
Diagnosis
A diagnosis is usually confirmed by monitoring absolute neutrophil (ANC) count three times per week for at least six weeks.[1][3] The confirmation can be assisted with Lomb periodogram.[20] During the condition, which lasts for three to six days and tends to occur approximately every three weeks (but can range from 14 to 36 days),[2][3] the absolute neutrophil count (ANC) is less than 200-500 cells/microL (<0.2-0.5x109/L), with increase of monocyte counts, and mild oscillations of other cells, including a mild anemia.[1][21] Between cycles the neutrophil count mostly peaks at subnormal or normal values.[17]
Genetic testing is advised for mutations in the ELANE and other neutropenia related genes (like HAX1, G6PC3, GFI1 etc.) to differentiate it from other secondary causes and forms of neutropenia.[1][22] In some cases intervals and oscillations can be lower, making the ANC analysis insufficient,[1] and since both disorders can have the same mutation variants in ELANE it is preferable to have both ANC and genetic analysis to confirm in the diagnosis whether it is severe congenital or cyclic neutropenia.[21][20]
Treatment

Although individuals between cycles are generally healthy and symptoms tend to improve in adulthood, it is advised avoiding activities prone to injuries, to have regular oral and dental care,[2] and BCG vaccine to be avoided.[1][13] It is advised monitoring white blood cells several times a year. The treatment following the symptoms should be immediate to prevent infections, especially during a fever when it requires broad-spectrum antibiotic therapy (see febrile neutropenia). The most important and often life-saving treatment is the preventive therapy of granulocyte colony-stimulating factor (G-CSF), in the form of filgrastim, which regulates the production of neutrophils within the bone marrow, but shortens the neutropenic cycle to about 7-14 days and the duration of the severe condition.[1][17] The subcutaneous injections, with median dosage of 1.5 μg/kg/day,[18] can be given daily, intermittently once every three days, or timed to just treat the neutropenic period.[13][23] The therapy is considered to be "safe and effective", with no significant adverse effects,[24] besides a possibility of development of osteopenia.[21]
The granulocyte-macrophage colony-stimulating factor (GM-CSF) is less effective with more adverse effects. Another alternative is hematopoietic stem cell transplantation (HSCT), but is usually practiced in SCN,[1] and in one case between two sibling donors, one of which was undergoing HSCT treatment for acute myeloid leukemia (AML) while the second had CyN and whose marrow was transferred, was also transferred CyN through allogeneic marrow grafting. It shows that CyN is a stem cell disorder.[25] Yearly bone marrow examinations are not recommended.[23]
Prognosis
There is a very high risk of life-threatening infections and death at an early age.[13] The quality of life and survival greatly improves with G-CSF treatment, which is practiced since the late 1980s.[21] Unlike severe congenital neutropenia, individuals with cyclic neutropenia have a better response to G-CSF and do not have a risk of developing myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML).[1][3] However, in long-term observation of over 300 patients with CyN, there has been one case of developing chronic myelogenous leukemia (CML) and one of AML,[21][24] indicating it is also a pre-leukemic condition, but the risk is "very low" (1%[18]),[26] and the risk is "correlated with disease severity rather than with occurrence of an ELANE mutation".[10] According to Donadieu et al. (2011), "the cumulative risk of experiencing at least one serious (potentially life-threatening) infection by age 20 years is similar in patients with permanent and cyclic neutropenia, although the former patients tend to have earlier manifestations".[13]
History
First described in 1910,[21][2] it was suggested and confirmed to have an autosomal dominant (AD) inheritance in the 1940s and 1960s,[27] but was differentiated from congenital neutropenias until the 1990s when were analyzed pedigrees and identified genetic mutations shared by patients with severe congenital neutropenia.[13]
See also
- Leukopenia
- Agranulocytosis
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 "ELANE-Related Neutropenia". GeneReviews. 2018. PMID 20301705. https://www.ncbi.nlm.nih.gov/books/NBK1533/.
- ↑ 2.0 2.1 2.2 2.3 "Cyclic neutropenia. Clinical case report". Revista Odontológica Mexicana 19 (4): 246–252. 2015. doi:10.1016/j.rodmex.2015.10.015.
- ↑ 3.0 3.1 3.2 3.3 3.4 "How to approach neutropenia". Hematology. American Society of Hematology. Education Program 2012 (1): 174–82. 2012. doi:10.1182/asheducation.v2012.1.174.3798251. PMID 23233578.
- ↑ James, William D; Elston, Dirk M; Berger, Timothy G; Andrews, George Clinton (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Saunders Elsevier. p. 808–811. ISBN 978-0-7216-2921-6. https://archive.org/details/andrewsdiseasess00mdwi_659.
- ↑ "A comparison of the defective granulopoiesis in childhood cyclic neutropenia and in severe congenital neutropenia". Haematologica 90 (8): 1032–41. August 2005. PMID 16079102. http://www.haematologica.org/cgi/pmidlookup?view=long&pmid=16079102.
- ↑ 6.0 6.1 "The diversity of mutations and clinical outcomes for ELANE-associated neutropenia". Current Opinion in Hematology 22 (1): 3–11. January 2015. doi:10.1182/blood.V118.21.3398.3398. PMID 25427142.
- ↑ "ELANE mutations in cyclic and severe congenital neutropenia: genetics and pathophysiology". Hematology/Oncology Clinics of North America 27 (1): 19–41, vii. February 2013. doi:10.1016/j.hoc.2012.10.004. PMID 23351986. PMC 3559001. https://www.hemonc.theclinics.com/article/S0889-8588(12)00209-2/abstract.
- ↑ 8.0 8.1 "Mutations in the ELA2 gene correlate with more severe expression of neutropenia: a study of 81 patients from the French Neutropenia Register". Blood 103 (11): 4119–25. June 2004. doi:10.1182/blood-2003-10-3518. PMID 14962902. http://www.bloodjournal.org/content/103/11/4119.long.
- ↑ 9.0 9.1 9.2 "Cyclic neutropenia and severe congenital neutropenia in patients with a shared ELANE mutation and paternal haplotype: evidence for phenotype determination by modifying genes". Pediatric Blood & Cancer 55 (2): 314–7. August 2010. doi:10.1002/pbc.22537. PMID 20582973.
- ↑ 10.0 10.1 "The spectrum of ELANE mutations and their implications in severe congenital and cyclic neutropenia". Human Mutation 34 (6): 905–14. June 2013. doi:10.1002/humu.22308. PMID 23463630.
- ↑ "The diversity of mutations and clinical outcomes for ELANE-associated neutropenia". Current Opinion in Hematology 22 (1): 3–11. January 2015. doi:10.1097/MOH.0000000000000105. PMID 25427142.
- ↑ "A Case Report on Recurrent Oral Ulcers Associated with Cyclic Neutropenia". Annals of Clinical Case Reports 2: 905–914. 2017. ISSN 2474-1655.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 "Congenital neutropenia: diagnosis, molecular bases and patient management". Orphanet Journal of Rare Diseases 6: 26. May 2011. doi:10.1186/1750-1172-6-26. PMID 21595885.
- ↑ "ELANE whole gene deletion mutation". Blood Advances 3 (16): 2470–2473. August 2019. doi:10.1182/bloodadvances.2019000498. PMID 31427279.
- ↑ "Conditional Expression of Mutant ELANE Produces Unfolded Protein Response but Fails to Promote Cell Death or Differentiation Block: What Is the Mechanism for Severe Congenital Neutropenia?". Blood 128 (22): 3899. December 2016. doi:10.1182/blood.V128.22.3899.3899.
- ↑ "ELANE mutation impairs granulocytic differentiation, without eliciting an unfolded protein response". The Journal of Biological Chemistry 295 (21): 7492–7500. May 2020. doi:10.1074/jbc.RA120.012366. PMID 32299910.
- ↑ 17.0 17.1 17.2 17.3 "Neutrophil elastase in cyclic and severe congenital neutropenia". Blood 109 (5): 1817–24. March 2007. doi:10.1182/blood-2006-08-019166. PMID 17053055.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 "New insights into the pathomechanism of cyclic neutropenia". Annals of the New York Academy of Sciences 1466 (1): 83–92. April 2020. doi:10.1111/nyas.14309. PMID 32083314. Bibcode: 2020NYASA1466...83M.
- ↑ "ELANE mutant-specific activation of different UPR pathways in congenital neutropenia". British Journal of Haematology 172 (2): 219–27. January 2016. doi:10.1111/bjh.13823. PMID 26567890.
- ↑ 20.0 20.1 "Cyclic Neutropenia, Congenital and Idiopathic Neutropenia". Blood 130: 2275. 2017. http://www.bloodjournal.org/content/130/Suppl_1/2275. Retrieved 2019-08-12.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 "The Natural History of Cyclic Neutropenia: Long-Term Prospective Observations and Current Perspectives". Blood 120 (21): 2141. 2012. doi:10.1182/blood.V120.21.2141.2141. http://www.bloodjournal.org/content/120/21/2141. Retrieved 2019-08-12.
- ↑ "ELANE mutations in congenital neutropenia: a single-centre study in patients of Indian origin". Journal of Clinical Pathology 71 (12): 1046–1050. December 2018. doi:10.1136/jclinpath-2018-205235. PMID 30171085.
- ↑ 23.0 23.1 "How I manage children with neutropenia". British Journal of Haematology 178 (3): 351–363. August 2017. doi:10.1111/bjh.14677. PMID 28419427.
- ↑ 24.0 24.1 "Long-Term Effects of G-CSF Therapy in Cyclic Neutropenia". The New England Journal of Medicine 377 (23): 2290–2292. December 2017. doi:10.1056/NEJMc1709258. PMID 29211670.
- ↑ "Human cyclic neutropenia transferred by allogeneic bone marrow grafting". Blood 60 (6): 1263–6. December 1982. doi:10.1182/blood.V60.6.1263.1263. PMID 6753968.
- ↑ "First Case of Leukemia in a Child Suffering from Cyclic Neutropenia with ELANE Mutation". Blood 126 (23): 997. 2015. doi:10.1182/blood.V126.23.997.997.
- ↑ "Severe congenital cyclic neutropenia: A case report". International Journal of Applied & Basic Medical Research 6 (4): 293–296. 2016. doi:10.4103/2229-516X.192598. PMID 27857902.
External links
- Severe Chronic Neutropenia International Registry
- "Understanding Neutropenia: The 20 Year Experience of the Severe Chronic Neutropenia International Registry (SCNIR)" (2014)
| Classification | |
|---|---|
| External resources |
 |
