Medicine:Feeding tube
| Feeding tube | |
|---|---|
 | |
| ICD-9-CM | 96.35 |
| MeSH | D004750 |
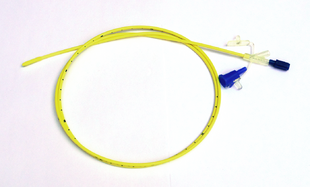
A feeding tube is a medical device used to provide nutrition to people who cannot obtain nutrition by mouth, are unable to swallow safely, or need nutritional supplementation. The state of being fed by a feeding tube is called gavage, enteral feeding or tube feeding. Placement may be temporary for the treatment of acute conditions or lifelong in the case of chronic disabilities. A variety of feeding tubes are used in medical practice. They are usually made of polyurethane or silicone. The diameter of a feeding tube is measured in French units (each French unit equals 1⁄3 mm). They are classified by the site of insertion and intended use.[1]
Medical uses
There are dozens of conditions that may require tube feeding (enteral nutrition) to prevent or treat malnutrition. Conditions that necessitate feeding tubes include prematurity, failure to thrive (or malnutrition), neurologic and neuromuscular disorders, inability to swallow, anatomical and post-surgical malformations of the mouth and esophagus, cancer, Sanfilippo syndrome, and digestive disorders.[2]
Children
Feeding tubes are used widely in children with excellent success for a wide variety of conditions. Some children use them temporarily until they are able to eat on their own, while other children require them for a longer time. Some children only use feeding tubes to supplement their oral diet, while others rely on them exclusively.[3][4]
Dementia
People with advanced dementia who get feeding assistance rather than feeding tubes have better outcomes.[5] Feeding tubes do not increase life expectancy for such people, or protect them from aspiration pneumonia.[5][6] Feeding tubes can also increase the risk of pressure ulcers, require pharmacological or physical restraints, and lead to distress.[5][7][8][9] In the final stages of dementia, assisted feeding may still be preferred over a feeding tube to bring benefits of palliative care and human interaction even when nutritional goals are not being met.[citation needed]
ICU
Feeding tubes are often used in the intensive care unit (ICU) to provide nutrition to people who are critically ill while their medical conditions are addressed; as of 2016 there was no consensus as to whether nasogastric or gastric tubes led to better outcomes.[10]
Mechanical obstruction and dysmotility
There is at least moderate evidence for feeding tubes improving outcomes for chronic malnutrition in people with cancers of the head and neck that obstruct the esophagus and would limit oral intake,[11][12] people with advanced gastroparesis,[13] and ALS.[14] For long term use, gastric tubes appear to have better outcomes than nasogastric tubes.[15]
GI surgery
People who have surgery on their throat or stomach often have a feeding tube while recovering from surgery; a tube leading through the nose and down to the middle part of the small intestine is used, or a tube is directly placed through the abdomen to the small intestine. There is some evidence to suggest that people with a tube through the nose were able to start eating normally sooner.[16]
Product types
Medical nutrition companies make flavored products for drinking and unflavored for tube feeding. In the USA these are regulated as medical foods, which are defined in section 5(b) of the Orphan Drug Act (21 U.S.C. 360ee (b) (3)) as "a food which is formulated to be consumed or administered enterally under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation."[17][18]
Types
The most common types of tubes include those placed through the nose, including nasogastric, nasoduodenal, and nasojejunal tubes, and those placed directly into the abdomen, such as a gastrostomy, gastrojejunostomy, or jejunostomy feeding tube.[19][20]
Nasogastric feeding tube
A nasogastric feeding tube or NG-tube is passed through the nares (nostril), down the esophagus and into the stomach. This type of feeding tube is generally used for short term feeding, usually less than a month, though some infants and children may use an NG-tube longterm. Individuals who need tube feeding for a longer period of time are typically transitioned to a more permanent gastric feeding tube. The primary advantage of the NG-tube is that it is temporary and relatively non-invasive to place, meaning it can be removed or replaced at any time without surgery. NG-tubes can have complications, particularly related to accidental removal of the tube and nasal irritation.[21] More specifically, when nasogastric or nasoenteric tubes are placed incorrectly, they can damage patients' vocal cords, lungs, or trachea, resulting in serious injuries or even death.[22]
In March 2022, Avanos Medical's Cortrak2 EAS recall, for instance, has been classified as a Class I recall by the FDA, following reports of injuries and patient deaths caused by misplaced nasoenteric or nasogastric tubes.[22]
Nasojejunal feeding tube
A nasojejunal or NJ-tube is similar to an NG-tube except that it is threaded through the stomach and into the jejunum, the middle section of the small intestine. In some cases, a nasoduodenal or ND-tube may be placed into the duodenum, the first part of the small intestine. These types of tube are used for individuals who are unable to tolerate feeding into the stomach, due to dysfunction of the stomach, impaired gastric motility, severe reflux or vomiting. These types of tubes must be placed in a hospital setting.[16][23]
Gastrostomy or gastric feeding tube
A gastric feeding tube (G-tube or "button") is a tube inserted through a small incision in the abdomen into the stomach and is used for long-term enteral nutrition. One type is the percutaneous endoscopic gastrostomy (PEG) tube which is placed endoscopically. The position of the endoscope can be visualized on the outside of the person's abdomen because it contains a powerful light source. A needle is inserted through the abdomen, visualized within the stomach by the endoscope, and a suture passed through the needle is grasped by the endoscope and pulled up through the esophagus. The suture is then tied to the end of the PEG tube that will be external, and pulled back down through the esophagus, stomach, and out through the abdominal wall. The insertion takes about 20 minutes. The tube is kept within the stomach either by a balloon on its tip (which can be deflated) or by a retention dome which is wider than the tract of the tube. G-tubes may also be placed surgically, using either an open or laparoscopic technique.[24]
Gastric feeding tubes are suitable for long-term use, though they sometimes need to be replaced if used long-term. The G-tube can be useful where there is difficulty with swallowing because of neurologic or anatomic disorders (stroke, esophageal atresia, tracheoesophageal fistula, radiotherapy for head and neck cancer), and to decrease the risk of aspiration pneumonia.[25] However, in people with advanced dementia or adult failure to thrive it does not decrease the risk of pneumonia. There is moderate quality evidence suggesting that the risk of aspiration pneumonia may be reduced by inserting the feeding tube into the duodenum or the jejunum (post-pyloric feeding), when compared to inserting the feeding tube into the stomach.[25] People with dementia may attempt to remove the PEG, which causes complications.[26]
Gastric drainage tube
A G-tube may instead be used for gastric drainage as a longer-term solution to the condition where blockage in the proximal small intestine causes bile and acid to accumulate in the stomach, typically leading to periodic vomiting, or if the vagus nerve is damaged. Where such conditions are only short term, as in a hospital setting, a nasal tube connected to suction is usually used. A blockage lower in the intestinal tract may be addressed with a surgical procedure known as a colostomy, and either type of blockage may be corrected with a bowel resection under appropriate circumstances. If such correction is not possible or practical, nutrition may be supplied by parenteral nutrition.[27][28]
Gastrojejunal feeding tube
A gastrojejunostomy or GJ feeding tube is a combination device that includes access to both the stomach and the jejunum, or middle part of the small intestine. Typical tubes are placed in a G-tube site or stoma, with a narrower long tube continuing through the stomach and into the small intestine. The GJ-tube is used widely in individuals with severely impaired gastric motility, high risk of aspiration, or an inability to feed into the stomach. It allows the stomach to be continually vented or drained while simultaneously feeding into the small intestine. GJ-tubes are typically placed by an interventional radiologist in a hospital setting. The primary complication of a GJ-tube is migration of the long portion of the tube out of the intestine and back into the stomach.[29]
Jejunal feeding tube
A jejunostomy feeding tube (J-tube) is a tube surgically or endoscopically inserted through the abdomen and into the jejunum (the second part of the small intestine).[16]
Complications
Nasogastric and nasojejeunal tubes are meant to convey liquid food to the stomach or intestines. When inserted incorrectly, the tip may rest in the respiratory system instead of the stomach or intestines; in this case, the liquid food will enter the lungs, resulting in pneumonia and can, in rare cases, lead to death.[23][30][31]
Complications associated with gastrostomy tubes (inserted through the abdomen and into the stomach or intestines) include leakage of gastric contents (containing hydrochloric acid) around the tube into the abdominal (peritoneal) cavity resulting in peritonitis, a serious complication which will cause death if it is not properly treated. Septic shock is another possible complication.[32] Minor leakage may cause irritation of the skin around the gastrostomy site or stoma. Barrier creams, to protect the skin from the corrosive acid, are used to manage this.[33]
A phenomenon called "tube dependency" has been discussed in the medical literature, in which a child refuses to eat after being on a feeding tube, but it is not recognized as a disorder in the ICD or DSM and its epidemiology is unknown.[34]
Oral and dental complications
Guidelines for dental care for children fed by tube are poorly established. Many dental complications arise due to poor oral health that may result from reluctance or intolerance towards oral hygiene practices by patients and caregivers, abundance of dental plaque and/or tooth decay, and lack of oral simulation.[35] Although many studies on this topic involve a relatively small sample size, the findings are important as they are associated with the development of various oral conditions, dental diseases and even systemic diseases such as aspiration pneumonia.[36][37]
Calculus
Adults fed by tube have previously shown a significantly higher rate and quantity of calculus deposition than adults fed orally. Even with an intensive oral hygiene program in place, adults fed by tube still demonstrate a greater quantity of supra-gingival calculus accumulation,[35] which can be a risk factor for several oral diseases including periodontal diseases and aspiration pneumonia. Although calculus removal may be difficult for caregivers to perform and provide an unpleasant experience for patients with a feeding tube, the implications of calculus in the initiation of aspiration pneumonia make it clear that it poses a serious health risk. Research suggests that the best course of treatment for patients with a gastric tube is periodic professional cleaning, maintained with routine home use of a non-foaming anti-calculus dentifrice (toothpaste).[36]
Caries
Dental caries is a localized disease in which susceptible tooth structure is broken down by bacteria that are able to ferment carbohydrates into acid. Although it has not been extensively studied, researchers speculate that individuals fed by tube may be less prone to the development of caries as they are not exposed to carbohydrates orally. Examination of dental plaque from tube-fed individuals found that it contained fewer caries-associated microorganisms (lactobacilli and streptococcus) and had reduced ability to produce acids, suggesting an overall weaker ability to cause caries. Further, studies with animal subjects found that tube-feeding was not associated with tooth decay, even when combined with reduced salivation.[35] Thus, tube-feeding alone does not necessarily directly promote the development of caries.
Periodontal diseases
To date, no published studies have been conducted on periodontal disease indicators (including clinical attachment loss, pocket depth, or periodontal indices) among tube-fed individuals. However, since tube feeding is correlated with calculus build-up, which is known to be a risk factor in the development of periodontal diseases, further investigation is critical to determine what role tube-feeding might have in the development of periodontal disease.[35]
Dental erosion
Dental erosion is the dissolution of the tooth's hard structures (enamel, dentin & cementum) by exposure to acids not caused by bacteria. In the case of individuals fed by gastric tube, acid may enter the oral cavity through reflux of gastric contents. Gastroesophageal reflux (GER) affects up to 67% of children and young adults with central nervous system dysfunction, a condition which in itself is normally an indicator for tube feeding. The effects of gastric acid on the teeth may sometimes be masked or minimized by the abundance of calculus. Tube feeding may either resolve, exacerbate or introduce the issue of GER in individuals.[35]
Aspiration pneumonia
Individuals fed by tube are susceptible to aspiration through a multitude of factors. Firstly, undisturbed plaque is known to shift towards the type of bacteria (Gram-negative anaerobic) implicated in aspiration pneumonia. Additionally, tube-fed patients are commonly affected by gastroesophageal reflux and a breakdown in the airway protection reflex (breathing while swallowing). This results in the inadvertent inhalation of bacteria-containing gastric juices as they are re-swallowed, leading to the development of aspiration pneumonia.[35]
Oral hypersensitivity
While a child undergoes a period of tube-feeding, there is a lack of oral stimulation that can lead to the development of oral hypersensitivity. This can complicate the delivery of dental care and serve as a barrier for the child's return to oral feeding. This can also lead to dysphagia (difficulty swallowing), muscle weakness and improper airway protection, resulting in longer periods of tube-feeding and increased risk of dental complications. A dentist may prescribe a "desensitization program", which involves routine stimulation of intra-oral and extra-oral structures, and encourage oral hygiene procedures to be performed at home.[35]
History
While enemas were previously used for supplemental enteral nutrition, the practice of surgically inserting feeding tubes emerged in the mid to late 1800s. Initially, these procedures were largely unsuccessful, but they quickly improved with advancements in technique.[38]
Originally, the nasogastric tube (NGT) was described by John Hunter in the 18th century as a combination of eelskin and whalebone. It was initially utilized to provide liquid nutrition to the ill.[39]
See also
- Bioethics
- Force-feeding for tube feeding against an individual's will or as torture
- Nutrient enema
- Nasogastric tube
- Medical food
- Intralipid
- Gastrostomy
- Percutaneous endoscopic gastrostomy
- Jejunostomy
References
- ↑ "Tube feeding". 2019-05-09. https://www.stjude.org/treatment/patient-resources/caregiver-resources/patient-family-education-sheets/nutrition-dietary/tube-feeding.html.
- ↑ Yasuda, Hideto; Kondo, Natsuki; Yamamoto, Ryohei; Asami, Sadaharu; Abe, Takayuki; Tsujimoto, Hiraku; Tsujimoto, Yasushi; Kataoka, Yuki (2021-09-27). "Monitoring of gastric residual volume during enteral nutrition". The Cochrane Database of Systematic Reviews 2021 (9): CD013335. doi:10.1002/14651858.CD013335.pub2. ISSN 1469-493X. PMID 34596901.
- ↑ Hannah, E; John, RM (November 2013). "Everything the nurse practitioner should know about pediatric feeding tubes.". Journal of the American Association of Nurse Practitioners 25 (11): 567–77. doi:10.1002/2327-6924.12075. PMID 24170530.

- ↑ Craig, GM (December 2013). "Psychosocial aspects of feeding children with neurodisability.". European Journal of Clinical Nutrition 67 (Suppl 2): S17–20. doi:10.1038/ejcn.2013.226. PMID 24301004.

- ↑ 5.0 5.1 5.2 American Academy of Hospice and Palliative Medicine, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Hospice and Palliative Medicine), http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-hospice-palliative-medicine/, retrieved 1 August 2013
- ↑ Murray, A; Mulkerrin, S; O'Keeffe, ST (2019). "The perils of 'risk feeding'". Age and Ageing 48 (4): 478–481. doi:10.1093/ageing/afz027. PMID 30939597.
- ↑ Hanson, L. C.; Ersek, M.; Gilliam, R.; Carey, T. S. (2011). "Oral Feeding Options for People with Dementia: A Systematic Review". Journal of the American Geriatrics Society 59 (3): 463–472. doi:10.1111/j.1532-5415.2011.03320.x. PMID 21391936.
- ↑ Kuo, S.; Rhodes, R. L.; Mitchell, S. L.; Mor, V.; Teno, J. M. (2009). "Natural History of Feeding-Tube Use in Nursing Home Residents with Advanced Dementia". Journal of the American Medical Directors Association 10 (4): 264–270. doi:10.1016/j.jamda.2008.10.010. PMID 19426943.
- ↑ *Sampson, E. L.; Candy, B.; Jones, L. (2009). Sampson, Elizabeth L. ed. "Enteral tube feeding for older people with advanced dementia". The Cochrane Database of Systematic Reviews 2009 (2): CD007209. doi:10.1002/14651858.CD007209.pub2. PMID 19370678.
- ↑ Schlein, K (August 2016). "Gastric Versus Small Bowel Feeding in Critically Ill Adults.". Nutrition in Clinical Practice 31 (4): 514–22. doi:10.1177/0884533616629633. PMID 26920643.
- ↑ Bishop, S; Reed, WM (December 2015). "The provision of enteral nutritional support during definitive chemoradiotherapy in head and neck cancer patients.". Journal of Medical Radiation Sciences 62 (4): 267–76. doi:10.1002/jmrs.132. PMID 27512573.
- ↑ Canadian Agency for Drugs and Technologies in Health (13 August 2014). "Nasogastric Feeding Tubes versus Percutaneous Endoscopic Gastrostomy for Patients with Head or Neck Cancer: A Review of Clinical Effectiveness and Guidelines". Rapid Response Reports. CADTH Rapid Response Reports. PMID 25411678. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0070223/.
- ↑ Sarosiek, I; Davis, B; Eichler, E; McCallum, RW (March 2015). "Surgical approaches to treatment of gastroparesis: gastric electrical stimulation, pyloroplasty, total gastrectomy and enteral feeding tubes.". Gastroenterology Clinics of North America 44 (1): 151–67. doi:10.1016/j.gtc.2014.11.012. PMID 25667030.
- ↑ Greenwood, DI (June 2013). "Nutrition management of amyotrophic lateral sclerosis.". Nutrition in Clinical Practice 28 (3): 392–9. doi:10.1177/0884533613476554. PMID 23466470.
- ↑ Lai, L; Ali, SF (September 2015). "Percutaneous Endoscopic Gastrostomy and Open Gastrostomy.". Atlas of the Oral and Maxillofacial Surgery Clinics of North America 23 (2): 165–8. doi:10.1016/j.cxom.2015.05.001. PMID 26333904.
- ↑ 16.0 16.1 16.2 Wang, L; Tian, Z; Liu, Y (January 2017). "Nasoenteric tube versus jejunostomy for enteral nutrition feeding following major upper gastrointestinal operations: a meta-analysis.". Asia Pacific Journal of Clinical Nutrition 26 (1): 20–26. doi:10.6133/apjcn.112015.05. PMID 28049257. http://apjcn.nhri.org.tw/server/APJCN/26/1/20.pdf.
- ↑ Affairs, Office of Regulatory (2019-02-09). "Medical Foods Guidance Documents & Regulatory Information". https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/MedicalFoods/default.htm.
- ↑ Nutrition, Center for Food Safety and Applied. "Medical Foods - Guidance for Industry: Frequently Asked Questions About Medical Foods; Second Edition". https://www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/MedicalFoods/ucm054048.htm.
- ↑ Guenter, Peggi (2001). "Enteral Feeding Access Devices". in Guenter, Peggi; Silkroski, Marcia. Tube Feeding: Practical Guidelines and Nursing Protocols. Gaithersburg: Aspen Publishers. pp. 51–67. ISBN 978-0-8342-1939-7. https://books.google.com/books?id=dhCmKKpNcK0C&pg=PA51.
- ↑ "Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition". NICE. August 2017. https://www.nice.org.uk/guidance/cg32/chapter/1-Guidance.
- ↑ "Dysphagia Treatment". NHS Choices. 19 January 2015. https://www.nhs.uk/conditions/swallowing-problems-dysphagia/treatment/.
- ↑ 22.0 22.1 "Avanos Medical Recalls Cortrak*2 Enteral Access System for Risk of Misplaced Enteral Tubes Could Cause Patient Harm". fda.gov. 16 May 2022. https://www.fda.gov/medical-devices/medical-device-recalls/avanos-medical-recalls-cortrak2-enteral-access-system-risk-misplaced-enteral-tubes-could-cause.
- ↑ 23.0 23.1 Tiancha, H; Jiyong, J; Min, Y (July 2015). "How to Promote Bedside Placement of the Postpyloric Feeding Tube: A Network Meta-Analysis of Randomized Controlled Trials.". Journal of Parenteral and Enteral Nutrition 39 (5): 521–30. doi:10.1177/0148607114546166. PMID 25146431.
- ↑ Thaker, AM; Sedarat, A (September 2016). "Laparoscopic-Assisted Percutaneous Endoscopic Gastrostomy.". Current Gastroenterology Reports 18 (9): 46. doi:10.1007/s11894-016-0520-2. PMID 27422123.
- ↑ 25.0 25.1 Alkhawaja, Sana; Martin, Claudio; Butler, Ronald J.; Gwadry-Sridhar, Femida (2015-08-04). "Post-pyloric versus gastric tube feeding for preventing pneumonia and improving nutritional outcomes in critically ill adults". The Cochrane Database of Systematic Reviews 2018 (8): CD008875. doi:10.1002/14651858.CD008875.pub2. ISSN 1469-493X. PMID 26241698.
- ↑ Siamak Milanchi; Matthew T Wilson (January–March 2008). "Malposition of percutaneous endoscopic-guided gastrostomy: Guideline and management". J Minim Access Surg 4 (1): 1–4. doi:10.4103/0972-9941.40989. PMID 19547728.
- ↑ Costa, G; Ruscelli, P; Balducci, G; Buccoliero, F; Lorenzon, L; Frezza, B; Chirletti, P; Stagnitti, F et al. (2016). "Clinical strategies for the management of intestinal obstruction and pseudo-obstruction. A Delphi Consensus study of SICUT (Società Italiana di Chirurgia d'Urgenza e del Trauma).". Annali Italiani di Chirurgia 87: 105–17. PMID 27179226.
- ↑ Mulholland, Michael W.; Doherty, Gerard M. (2011) (in en). Complications in Surgery. Lippincott Williams & Wilkins. p. 270. ISBN 978-1-60547-530-1. https://books.google.com/books?id=MQX59bsB3CwC&pg=PA270.
- ↑ Gershman, George; Ament, Marvin (2008) (in en). Practical Pediatric Gastrointestinal Endoscopy. John Wiley & Sons. p. 126. ISBN 978-0-470-98731-5. https://books.google.com/books?id=bAAUI9f04jIC&pg=PA126.
- ↑ Santos, SC; Woith, W; Freitas, MI; Zeferino, EB (September 2016). "Methods to determine the internal length of nasogastric feeding tubes: An integrative review.". International Journal of Nursing Studies 61: 95–103. doi:10.1016/j.ijnurstu.2016.06.004. PMID 27328376.
- ↑ Metheny, NA; Meert, KL (May 2014). "Effectiveness of an electromagnetic feeding tube placement device in detecting inadvertent respiratory placement.". American Journal of Critical Care 23 (3): 240–7; quiz 248. doi:10.4037/ajcc2014954. PMID 24786813.

- ↑ "Bowel necrosis associated with early jejunal tube feeding: A complication of postoperative enteral nutrition". Arch Surg 141 (7): 701–4. July 2006. doi:10.1001/archsurg.141.7.701. PMID 16847244.
- ↑ Townley, A; Wincentak, J; Krog, K; Schippke, J; Kingsnorth, S (2018). "Pediatric gastrostomy stoma complications and treatments: A rapid scoping review.". Journal of Clinical Nursing 27 (7–8): 1369–1380. doi:10.1111/jocn.14233. PMID 29266535.
- ↑ Krom, H; de Winter, JP; Kindermann, A (June 2017). "Development, prevention, and treatment of feeding tube dependency.". European Journal of Pediatrics 176 (6): 683–688. doi:10.1007/s00431-017-2908-x. PMID 28409284.
- ↑ 35.0 35.1 35.2 35.3 35.4 35.5 35.6 Dyment, Heather A.; Casas, Michael J. (1999). "Dental care for children fed by tube: a critical review" (in en). Special Care in Dentistry 19 (5): 220–224. doi:10.1111/j.1754-4505.1999.tb01389.x. ISSN 1754-4505. PMID 10765889.
- ↑ 36.0 36.1 Brown, Laurie M.; Casamassimo, Paul S.; Griffen, Ann; Tatakis, Dimitris (Sep–Oct 2006). "Supragingival calculus in children with gastrostomy feeding: significant reduction with a caregiver-applied tartar-control dentifrice". Pediatric Dentistry 28 (5): 410–414. ISSN 0164-1263. PMID 17036705.
- ↑ Cardona‐Soria, Sandra; Cahuana‐Cárdenas, Abel; Rivera‐Baró, Alejandro; Miranda‐Rius, Jaume; Martín de Carpi, Javier; Brunet‐Llobet, Lluís (2019-11-07). "Oral health status in pediatric patients with cerebral palsy fed by oral versus enteral route" (in en). Special Care in Dentistry 40 (1): 35–40. doi:10.1111/scd.12429. ISSN 0275-1879. PMID 31697430. https://onlinelibrary.wiley.com/doi/abs/10.1111/scd.12429.
- ↑ Minard, Gayle (December 2006). "The history of surgically placed feeding tubes". Nutrition in Clinical Practice 21 (6): 626–633. doi:10.1177/0115426506021006626. ISSN 0884-5336. PMID 17119170.
- ↑ "Nasogastric Tube". https://www.sciencedirect.com/topics/nursing-and-health-professions/nasogastric-tube.
External links
 |

