Medicine:Jones fracture
| Jones fracture | |
|---|---|
| Other names | Fracture of the metaphysis of the fifth metatarsal[1] |
 | |
| Jones fracture as seen on Xray | |
| Specialty | Emergency medicine, orthopedics, podiatry |
| Symptoms | Pain near the midportion of the foot on the outside, bruising[2][3] |
| Usual onset | Sudden[4] |
| Duration | 6-12 weeks to heal[5] |
| Causes | Bending the foot inwards when the toes are pointed[6] |
| Diagnostic method | Based on symptoms, X-rays[3] |
| Differential diagnosis | Pseudo-Jones fracture, normal growth plate[3][7] |
| Treatment | Non-weight bearing, cast, surgery[5] |
A Jones fracture is a broken bone in a specific part of the fifth metatarsal of the foot between the base and middle part[8] that is known for its high rate of delayed healing or nonunion.[4] It results in pain near the midportion of the foot on the outside.[2] There may also be bruising and difficulty walking.[3] Onset is generally sudden.[4]
The fracture typically occurs when the toes are pointed and the foot bends inwards.[6][2] This movement may occur when changing direction while the heel is off the ground such in dancing, tennis, or basketball.[9][10] Diagnosis is generally suspected based on symptoms and confirmed with X-rays.[3]
Initial treatment is typically in a cast, without any walking on it, for at least six weeks.[5] If, after this period of time, healing has not occurred, a further six weeks of casting may be recommended.[5] Due to poor blood supply in this area, the break sometimes does not heal and surgery is required.[3] In athletes, or if the pieces of bone are separated, surgery may be considered sooner.[5][8] The fracture was first described in 1902 by orthopedic surgeon Robert Jones, who sustained the injury while dancing.[11][4]
Diagnosis
A person with a Jones fracture may not realize that a fracture has occurred. Diagnosis includes the palpation of an intact fibularis brevis tendon, and demonstration of local tenderness distal to the tuberosity of the fifth metatarsal, and localized over the shaft of the proximal metatarsal.
Diagnostic X-rays include anteroposterior, oblique, and lateral views and should be made with the foot in full flexion.[citation needed]
Differential diagnosis
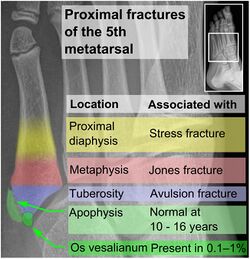
- Proximal diaphysis, typically stress fracture.[12][13]
- Metaphysis: Jones fracture[14]
-Tuberosity: Pseudo-Jones fracture[15] (avulsion fracture).[15]
Normal anatomy:
- Apophysis: Normal at 10 - 16 years.[16]
- Os vesalianum, an accessory bone.[17]
Other proximal fifth metatarsal fractures exist, although they are not as problematic as a Jones fracture. If the fracture enters the intermetatarsal joint, it is a Jones fracture. If, however, it enters the tarsometatarsal joint, then it is likely an avulsion fracture caused by pull from the fibularis brevis tendon. An avulsion fracture at the base of the fifth metatarsal is sometimes called a "dancer's fracture" or a "pseudo Jones fracture", and usually responds readily to non-operative treatment.[18] The X-ray appearance of the developmental "apophysis" in this area may have some resemblance of a fracture, but is not a fracture; it is the secondary ossification center of the metatarsal bone. It is a normal finding that occurs at this site in adolescents.[19] If an injury to that area has occurred, the physician is often able to interpret certain radiographic clues to make the differentiation. An avulsion fracture at this location is typically extra-articular and oriented transversally as compared to the longitudinal orientation of an unfused apophysis.[19]
Treatment
Casting
Initial treatment is typically in a cast, without any weight being placed on it, for at least six weeks.[5] If after this period of time healing has not occurred a further six weeks of casting may be recommended.[5] Up to half, however, may not heal after casting.[2]
Surgery
In athletes or if the pieces of bone are separated by more than 2 mm surgery may be considered.[5][8] In a study of all players who entered the NFL Scouting Combine from 2009 to 2015, the incidence of Jones fracture was 3.2% and all had received surgery to repair the fracture with a metal screw.[20] For persons who are not athletes, surgery might not be recommended unless healing does not occur after a trial of cast treatment.[5]
Prognosis
For several reasons, a Jones fracture may not unite. The diaphyseal bone (zone II), where the fracture occurs, is an area of potentially poor blood supply, existing in a watershed area between two blood supplies. This may compromise healing. In addition, there are various tendons, including the fibularis brevis and fibularis tertius, and two small muscles attached to the bone. These may pull the fracture apart and prevent healing.[citation needed]
Zones I and III have been associated with relatively guaranteed union and this union has taken place with only limited restriction of activity combined with early immobilization. On the other hand, zone II has been associated with either delayed or non-union and, consequently, it has been generally agreed that fractures in this area should be considered for some form of internal immobilization, such as internal screw fixation.[citation needed]
These zones can be identified anatomically and on x-ray adding to the clinical usefulness of this classification.[21] Surgical intervention is not, by itself, a guarantee of cure and has its own complication rate. Other reviews of the literature have concluded that conservative, non-operative, treatment is an acceptable option for the non-athlete.[22]
-
Anatomy of the fifth metatarsal.
-
3 zone description
-
2 zone description
References
- ↑ "5th Metatarsal". Emergency Care Institute, New South Wales. 2017-09-19. https://www.aci.health.nsw.gov.au/networks/eci/clinical/clinical-resources/clinical-tools/orthopaedic-and-musculoskeletal/musculoskeletal-orthopaedic-guide/5th-metatarsal.
- ↑ 2.0 2.1 2.2 2.3 Eltorai, Adam E. M.; Eberson, Craig P.; Daniels, Alan H. (2017) (in en). Orthopedic Surgery Clerkship: A Quick Reference Guide for Senior Medical Students. Springer. pp. 395–397. ISBN 9783319525679. https://books.google.com/books?id=Y2AwDwAAQBAJ&pg=PA395.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 "Toe and Forefoot Fractures". June 2016. http://orthoinfo.aaos.org/topic.cfm?topic=a00165.
- ↑ 4.0 4.1 4.2 4.3 Valderrabano, Victor; Easley, Mark (2017) (in en). Foot and Ankle Sports Orthopaedics. Springer. p. 430. ISBN 9783319157351. https://books.google.com/books?id=uqsZDgAAQBAJ&pg=PA430.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 "Diagnosis and Management of Common Foot Fractures". American Family Physician 93 (3): 183–91. February 2016. PMID 26926612.
- ↑ 6.0 6.1 Dähnert, Wolfgang (2011) (in en). Radiology Review Manual. Lippincott Williams & Wilkins. p. 96. ISBN 9781609139438. https://books.google.com/books?id=uYREa2bKNW8C&pg=PA96.
- ↑ Conaghan, Philip G.; O'Connor, Philip; Isenberg, David A. (2010) (in en). Musculoskeletal Imaging. OUP Oxford. p. 231. ISBN 9780191575273. https://books.google.com/books?id=Si9oAgAAQBAJ&pg=PA231.
- ↑ 8.0 8.1 8.2 Joel A. DeLisa; Bruce M. Gans; Nicholas E. Walsh (2005). Physical Medicine and Rehabilitation: Principles and Practice. Lippincott Williams & Wilkins. pp. 881–. ISBN 978-0-7817-4130-9. https://books.google.com/books?id=1sWk1GYCvKoC&pg=PA881.
- ↑ Mattu, Amal; Chanmugam, Arjun S.; Swadron, Stuart P.; Tibbles, Carrie; Woolridge, Dale; Marcucci, Lisa (2012) (in en). Avoiding Common Errors in the Emergency Department. Lippincott Williams & Wilkins. p. 790. ISBN 9781451152852. https://books.google.com/books?id=Uu7BtlkzUSYC&pg=PA790.
- ↑ Lee, Edward (2017) (in en). Pediatric Radiology: Practical Imaging Evaluation of Infants and Children. Lippincott Williams & Wilkins. p. Chapter 24. ISBN 9781496380272. https://books.google.com/books?id=1f0wDwAAQBAJ&pg=PT4138.
- ↑ "I. Fracture of the Base of the Fifth Metatarsal Bone by Indirect Violence". Annals of Surgery 35 (6): 697–700.2. June 1902. PMID 17861128.
- ↑ "Diagnosis and Management of Common Foot Fractures". American Family Physician 93 (3): 183–91. February 2016. PMID 26926612. https://pubmed.ncbi.nlm.nih.gov/26926612.
- ↑ "5th Metatarsal". 2017-09-19. https://www.aci.health.nsw.gov.au/networks/eci/clinical/clinical-resources/clinical-tools/orthopaedic-and-musculoskeletal/musculoskeletal-orthopaedic-guide/5th-metatarsal.
- ↑ "Toe and Forefoot Fractures". June 2016. http://orthoinfo.aaos.org/topic.cfm?topic=a00165.
- ↑ 15.0 15.1 Silbergleit, Robert. "Foot Fracture". Medscape.com. http://emedicine.medscape.com/article/825060-overview.
- ↑ "Traction apophysitis of the fifth metatarsal base in a child: Iselin's disease". BMJ Case Reports 2014 (may14 4): bcr2014204687. May 2014. doi:10.1136/bcr-2014-204687. PMID 24832713.
- ↑ "Sesamoids and accessory ossicles of the foot: anatomical variability and related pathology". Insights into Imaging 4 (5): 581–93. October 2013. doi:10.1007/s13244-013-0277-1. PMID 24006205.
- ↑ "Toe and Forefoot Fractures/Fifth Metatarsal Fractures". American Academy of Orthopedic Surgeons. https://orthoinfo.aaos.org/en/diseases--conditions/toe-and-forefoot-fractures.
- ↑ 19.0 19.1 Saber, Mohamed; Sharma, Rohit (March 26, 2021). "Apophysis of the proximal 5th metatarsal". Radiopedia.org. https://radiopaedia.org/articles/apophysis-of-the-proximal-5th-metatarsal?lang=us.
- ↑ Spang, Robert C. (August 2018). "Jones Fractures Identified at the National Football League Scouting Combine: Assessment of Prognostic Factors, Computed Tomography Findings, and Initial Career Performance". Orthopaedic Journal of Sports Medicine 6 (8). doi:10.1177/2325967118790740. ISSN 2325-9671. PMID 30182027.
- ↑ "Acute fractures to the proximal fifth metatarsal bone: development of classification and treatment recommendations based on the current evidence". Injury 43 (10): 1626–32. October 2012. doi:10.1016/j.injury.2012.03.010. PMID 22465516.
- ↑ "The jones fracture classification, management, outcome, and complications: a systematic review". Foot & Ankle Specialist 5 (4): 256–9. August 2012. doi:10.1177/1938640012444730. PMID 22547534.
External links
| Classification | |
|---|---|
| External resources |
 |



