Medicine:ST elevation

ST elevation refers to a finding on an electrocardiogram wherein the trace in the ST segment is abnormally high above the baseline.
Electrophysiology
The ST segment starts from the J point (termination of QRS complex and the beginning of ST segment) and ends with the T wave. The ST segment is the plateau phase, in which the majority of the myocardial cells had gone through depolarization but not repolarization. The ST segment is the isoelectric line because there is no voltage difference across cardiac muscle cell membrane during this state. Any distortion in the shape, duration, or height of the cardiac action potential can distort the ST segment.[1]
Abnormalities

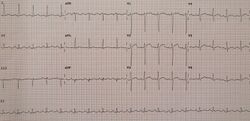
An ST elevation is considered significant if the vertical distance inside the ECG trace and the baseline at a point 0.04 seconds after the J-point is at least 0.1 mV (usually representing 1 mm or 1 small square) in a limb lead or 0.2 mV (2 mm or 2 small squares) in a precordial lead.[2] The baseline is either the PR interval or the TP interval.[3] This measure has a false positive rate of 15–20% (which is slightly higher in women than men) and a false negative rate of 20–30%.[4]
Myocardial infarction

When there is a blockage of the coronary artery, there will be lack of oxygen supply to all three layers of cardiac muscle (transmural ischemia). The leads facing the injured cardiac muscle cells will record the action potential as ST elevation during systole while during diastole, there will be depression of the PR segment and the PT segment. Since PR and PT interval are regarded as baseline, ST segment elevation is regarded as a sign of myocardial ischemia. The opposing leads (such as V3 and V4 versus posterior leads V7–V9) always show reciprocal ST segment changes (ST elevation in one lead is followed by ST depression in the opposing lead). This is highly specific for myocardial infarction. An upsloping, convex ST segment is highly predictive of a myocardial infarction (Pardee sign) while a concave ST elevation is less suggestive and can be found in other non-ischaemic causes.[1] Following infarction, ventricular aneurysm can develop, which leads to persistent ST elevation, loss of S wave, and T wave inversion.[1]
Weakening of the electrical activity of the cardiac muscles causes the decrease in height of the R wave in those leads facing it. In opposing leads, it manifests as Q wave. However, Q waves may be found in healthy individuals at lead I, aVL, V5 and V6 due to left to right depolarisation.[1]
Myocarditis/pericarditis
In these conditions, there will mostly be concave ST elevations in almost all the leads except for aVR and V1. These two leads, ST depression will be seen because they are the opposing leads of the cardiac axis. PR segment depression is highly suggestive of pericarditis. R wave in most cases will be unaltered. In two weeks after pericarditis, there will be upward concave ST elevation, positive T wave, and PR depression. After several more weeks, PR and ST segments normalised with flattened T wave. At last, there will be T wave inversion which will take weeks or months to vanish.[1]
Associated conditions
The topology and distribution of the affected areas depend on the underlying condition. Thus, ST elevation may be present on all or some leads of ECG.[citation needed]
It can be associated with:
- Myocardial infarction (see also ECG in myocardial infarction). ST elevation in select leads is more common with myocardial infarction. ST elevation only occurs in full thickness infarction
- Prinzmetal's angina[5]
- Acute pericarditis[6][7] ST elevation in all leads (diffuse ST elevation) is more common with acute pericarditis.
- Left ventricular aneurysm[8]
- Blunt trauma to the chest resulting in a cardiac contusion[9]
- Hyperkalemia[5]
- Acute myocarditis[5]
- Pulmonary embolism[5]
- Brugada syndrome[5]
- Hypothermia[5]
- J-point elevation[5]
- Early repolarization[citation needed]
- Subarachnoid hemorrhage[citation needed]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Erwin Christian, de Bliek (17 February 2018). "ST elevation: Differential diagnosis and caveats. A comprehensive review to help distinguish ST elevation myocardial infarction from nonischemic etiologies of ST elevation". Turkish Journal of Emergency Medicine 18 (1): 1–10. doi:10.1016/j.tjem.2018.01.008. PMID 29942875.
- ↑ Family Practice Notebook > ST Elevation Retrieved November 2010
- ↑ Khandpur, R.S. (2003). Handbook of biomedical instrumentation (2nd ed.). New Delhi: Tata McGraw-Hill. p. 255. ISBN 978-0-07-047355-3. https://books.google.com/books?id=C-rbT_c69oUC&pg=PA255.
- ↑ Sabatine MS (2000). Pocket Medicine (이소연). Lippincott Williams & Wilkins. ISBN 978-0-7817-1649-9.[page needed]
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Thaler, Malcolm (2009). The only EKG book you'll ever need. Lippincott Williams & Wilkins. ISBN 978-1-60547-140-2. https://books.google.com/books?id=wQfzn-2UIaoC&q=the+only+ecg.[page needed]
- ↑ "Acute pericarditis". American Family Physician 76 (10): 1509–1514. November 2007. PMID 18052017. http://www.aafp.org/link_out?pmid=18052017.
- ↑ "Electrocardiographical case. ST elevation: is this an infarct? Pericarditis". Singapore Medical Journal 46 (11): 656–660. November 2005. PMID 16228101. http://www.sma.org.sg/smj/4611/4611me2.pdf.
- ↑ Victor F. Froelicher; Jonathan Myers (2006). Exercise and the heart. Elsevier Health Sciences. pp. 138–. ISBN 978-1-4160-0311-3. https://books.google.com/books?id=HXw-Tsr1c8AC&pg=PA138. Retrieved 10 October 2010.
- ↑ "Electrocardiographic ST-segment elevation in the trauma patient: acute myocardial infarction vs myocardial contusion". The American Journal of Emergency Medicine 23 (4): 510–516. July 2005. doi:10.1016/j.ajem.2004.03.014. PMID 16032622.
 |
