Medicine:Bradycardia
| Bradycardia | |
|---|---|
| Other names | Bradyarrhythmia, brachycardia |
 | |
| Sinus bradycardia seen in lead II with a heart rate of about 50BPM | |
| Pronunciation | |
| Specialty | Cardiology |
| Diagnostic method | electrocardiogram |
| Frequency | 15% (males), 7% (females) |
Bradycardia is a medical term used to describe a resting heart rate under 60 beats per minute (BPM).[1] While bradycardia can result from a variety of pathologic processes, it is commonly a physiologic response to cardiovascular conditioning, or due to asymptomatic type 1 atrioventricular block. Resting heart rates less than 50 BPM are often normal during sleep in young and healthy adults, and in athletes.[2] In large population studies of adults without underlying heart disease, resting heart rates of 45-50 BPM appear to be the lower limits of normal, dependent on age and sex.[3][4] Bradycardia is most likely to be discovered in the elderly, as both age and underlying cardiac disease progression contribute to its development.[5]
Bradycardia may be associated with symptoms of fatigue, dyspnea, dizziness, confusion, and frank syncope due to reduced forward blood flow to the brain, lungs, and skeletal muscle.[6] The types of symptoms often depend on the etiology of the slow heart rate, classified by the anatomic location of a dysfunction within the cardiac conduction system.[7] Generally, these classifications involve the broad categories of sinus node dysfunction (SND), atrioventricular block, and other conduction tissue disease.[8] However, bradycardia can also result without dysfunction of the native conduction system, arising secondary to medications including beta blockers, calcium channel blockers, antiarrythmics, and other cholinergic drugs. Excess vagus nerve activity or carotid sinus hypersensitivity are neurological causes of transient symptomatic bradycardia. Hypothyroidism and metabolic derangements are other common extrinsic causes of bradycardia.[6]
The management of a bradycardia is generally reserved for patients with symptoms, regardless of minimum heart rate during sleep or the presence of concomitant heart rhythm abnormalities (See: Sinus pause), which are common with this condition.[6] Untreated SND has been shown to increase the future risk of heart failure and syncope, sometimes warranting definitive treatment with an implanted pacemaker.[9][8] In atrioventricular causes of bradycardia, permanent pacemaker implantation is often required when no reversible causes of disease are found.[6][7] In both SND and atrioventricular blocks, there is little role for medical therapy unless a patient is hemodynamically unstable, which may require the use of medications such as atropine, isoproterenol, and interventions such as transcutaenous pacing, until such time that an appropriate workup can be undertaken and long term treatment selected.[7] While asymptomatic bradycardias rarely require treatment, consultation with a physician is recommended, especially in the elderly.[citation needed]
The term "relative bradycardia" can refer to a heart rate lower than that expected in a particular disease state, often a febrile illness.[10] "Chronotropic incompetence" (CI) refers to an inadequate rise in heart rate during periods of increased demand, often due to exercise, and is an important sign of SND and indication for pacemaker implantation.[8][7]
The word "bradycardia" is from the Greek βραδύς bradys "slow", and καρδία kardia "heart".[11]
Normal cardiac conduction
The heart is a type of specialized muscle containing repeating units of cardiomyocytes, or heart muscle cells. Like most cells, cardiomyocytes maintain a highly regulated negative voltage at rest, and are capable of propagating action potentials, much like neurons.[12] While at rest, the negative cellular voltage of a cardiomyocyte can be raised above a certain threshold (so called depolarization) by an incoming action potential, causing the myocyte to contract. When these contractions occur in a coordinated fashion, the atria and ventricles of the heart will pump, delivering blood to the rest of the body.[12]
Normally, the origination of the action potential causing cardiomyocyte contraction originates from the sinoatrial node (SA node). This collection of specialized conduction tissue is located in the right atrium, near the entrance of the superior vena cava.[13] The SA node contains pacemaker cells that demonstrate "automaticity" and are capable of generating impulses that travel through the heart and create a steady heart beat.[13]
In the beginning of the cardiac cycle, the SA node generates an electrical action potential which spreads across the right and left atria, causing the atrial contraction of the cardiac cycle.[13] This electrical impulse carries on to the atrioventricular node (AV node), another specialized grouping of cells located in the base of the right atrium, which is the only anatomically normal electrical connection between the atria and ventricles. Impulses coursing through the AV node are slowed before carrying on to the ventricles,[14] allowing for appropriate filling of the ventricles before contraction. The SA and AV nodes are both closely regulated by fibers of the autonomic nervous system, allowing for adjustment of cardiac output by the central nervous system in times of increased metabolic demand.
Following slowed conduction through the atrioventricular node, the action potential originally produced at the SA node now flows through the His-purkinje system. The bundle of His originates in the AV node and rapidly splits into a left and right branch, each destined for a different ventricle. Finally, these bundle branches terminate in the small Purkinje fibers that innervate myocardial tissue. The His-purkinje system conducts action potentials much faster than can be propagated between myocardial cells, which allows the entire ventricular myocardium to contract in a smaller length of time, improving pump function.[13]
Classification
Most pathological causes of bradycardia result from damage to this normal cardiac conduction system at various levels: the sinoatrial node, the atrioventricular node, or from damage to conduction tissue between or after these nodes.
Sinus node
Bradycardia caused by the alterations of sinus node activity is divided into three types.
Sinus bradycardia
Sinus is a sinus rhythm of less than 50 BPM.[15] Cardiac action potentials are generated from the SA node, propagated through an otherwise normal conduction system, but occur at a slow rate. It is a common condition found in both healthy individuals and those considered well-conditioned athletes.[1] Studies have found that 50–85% of conditioned athletes have benign sinus bradycardia, as compared to 23% of the general population studied.[16] The heart muscle of athletes has a higher stroke volume, and so requires fewer contractions to circulate the same volume of blood.[17] Asymptomatic sinus bradycardia decreases in prevalence with age.
Sinus arrhythmia
Sinus arrhythmias are heart rhythm abnormalities characterized by variations in the cardiac cycle length in excess of 120 milliseconds (longest cycle - shortest cycle).[7] These are the most common type of arrhythmia in the general population, and are usually without significant consequence. They typically occur in the young, athletes, or after administration of medications such as morphine. The types of sinus arrhythmia are separated into the respiratory and non-respiratory categories.[7]
Respiratory sinus arrhythmia
Respiratory sinus arrhythmia refers to the physiologically normal variation in heart rate due to breathing. During inspiration, vagus nerve activity decreases, reducing parasympathetic innervation of the sinoatrial node, causing an increase in heart rate. During expiration, heart rates fall due to the converse occurring.[7]
Non-respiratory sinus arrhythmia
Non-respiratory causes of sinus arrhythmia include sinus pause, sinus arrest, and sinoatrial exit block. Sinus pause and arrest involve slowing or arrest of automatic impulse generation from the sinus node. This can lead to asystole, or cardiac arrest, if ventricular escape rhythms do not engage to create backup sources of cardiac action potentials.[7]
Sinoatrial exit block is a similar non-respiratory phenomenon of temporarily lost sinoatrial impulses. However, in contrast to a sinus pause, the action potential is still generated at the SA node, but is either unable to leave or delayed from leaving the node, preventing or delaying atrial depolariziation and subsequent ventricular systole. Therefore, the length of the pause in heart beats is usually a multiple of the P-P interval as seen on electrocardiography. Like a sinus pause, sinoatrial exit block can be symptomatic, especially with prolonged pause length.[7]
Sinus node dysfunction
A syndrome of intrinsic disease of the sinus node, referred to as sick sinus syndrome or sinus node dysfunction, covers conditions that include symptomatic sinus bradycardia or persistent chronotropic incompetence, sinoatrial block, sinus arrest, and tachycardia-bradycardia syndrome.[7] These conditions can be caused by damage to the native sinus node itself, and are frequently accompanied by damaged AV node conduction and reduced backup pacemaker activity.[18] The condition can also be caused dysfunction of the autonomic nervous system that regulates the node, and is commonly exacerbated by medications.[7]
Atrioventricular node
Bradycardia can also result to due to inhibition of the flow of action potentials through the atrioventricular (AV) node. While this can be normal in young patients due to excessive vagus nerve tone, symptomatic bradycardia due to AV node dysfunction in older people is commonly due to structural heart disease, myocardial ischemia, or age related fibrosis.[19]
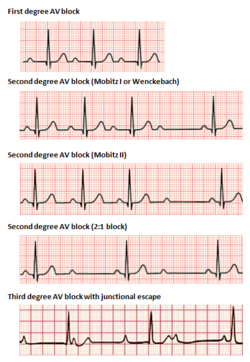
Atrioventricular block
Atrioventricular blocks are divided into 3 categories, ranked by severity. AV block is diagnosed via surface ECG, which is usually sufficient to locate the causal lesion of the block, without the need of an invasive electrophysiology study.[7]
In 1st degree AV block, electrical impulses originating in the SA node (or other ectopic focus above the ventricles) are conducted with significant delay through the AV node. This condition is diagnosed via ECG, with PR intervals in excess of 200 milliseconds.[7] The PR interval represents the length of time between the start of atrial depolarization and start of ventricular depolarization, representing the flow of electrical impulses between the SA and AV nodes. Despite the term "block", no impulses are actually fully lost in this conduction, but are merely delayed. The location of the causal lesion can be anywhere between the AV node and the His-Purkinje system, but is most commonly found in the AV node itself.[20] Generally, isolated PR prolongation in 1st degree AV block is not associated with increased mortality or hospitalization.[21]
2nd degree AV block is characterized by intermittently lost conduction of impulses between the SA node and the ventricles. 2nd degree block, is classified into two types. Mobitz type 1 block, otherwise known by the eponym Wenckebach, classically demonstrates grouped patterns of heart beats on ECG. Over the course of the group, the PR interval gradually lengthens, until there is a dropped conduction, resulting in no QRS complex seen on surface ECG following the last P wave. After a delay, the grouping repeats, with the PR interval shortening again to baseline.[22] Type 1 2nd degree AV block due to disease in the AV node (as opposed to in the His-purkinje system) rarely needs intervention with pacemaker implantation.[22]
2nd degree, Mobitz type 2 AV block is another phenomenon of intermittently dropped QRS complexes after characteristic groupings of beats seen on surface ECG. In this condition, the PR and RR intervals are consistent, followed by a sudden AV block and dropped QRS complex.[22] Because type 2 blocks are typically due to lesions below the AV node, the ability for ventricular escape rhythms to maintain cardiac output is compromised. Permanent pacemaker implantation is often required.[19]
Junctional rhythms
An AV-junctional rhythm, or atrioventricular nodal bradycardia, is usually caused by the absence of the electrical impulse from the sinus node. This usually appears on an electrocardiogram with a normal QRS complex accompanied with an inverted P wave either before, during, or after the QRS complex.[17]
An AV-junctional escape beat is a delayed heartbeat originating from an ectopic focus somewhere in the AV junction. It occurs when the rate of depolarization of the SA node falls below the rate of the AV node.[17] This dysrhythmia also may occur when the electrical impulses from the SA node fail to reach the AV node because of SA or AV block.[23] This is a protective mechanism for the heart to compensate for an SA node that is no longer handling the pacemaking activity and is one of a series of backup sites that can take over pacemaker function when the SA node fails to do so. This would present with a longer PR interval. An AV-junctional escape complex is a normal response that may result from excessive vagal tone on the SA node. Pathological causes include sinus bradycardia, sinus arrest, sinus exit block, or AV block.[17]
Ventricular
Idioventricular rhythm, also known as atrioventricular bradycardia or ventricular escape rhythm, is a heart rate of less than 50 BPM. This is a safety mechanism when a lack of electrical impulse or stimuli from the atrium occurs.[17] Impulses originating within or below the bundle of His in the AV node will produce a wide QRS complex with heart rates between 20 and 40 BPM. Those above the bundle of His, also known as junctional, will typically range between 40 and 60 BPM with a narrow QRS complex.[24][25] In a third-degree heart block, about 61% take place at the bundle branch-Purkinje system, 21% at the AV node, and 15% at the bundle of His.[25] AV block may be ruled out with an ECG indicating "a 1:1 relationship between P waves and QRS complexes."[24] Ventricular bradycardias occurs with sinus bradycardia, sinus arrest, and AV block. Treatment often consists of the administration of atropine and cardiac pacing.[17]
Infantile
For infants, bradycardia is defined as a heart rate less than 100 BPM (normal is around 120–160 BPM). Premature babies are more likely than full-term babies to have apnea and bradycardia spells; their cause is not clearly understood. The spells may be related to centers inside the brain that regulate breathing which may not be fully developed. Touching the baby gently or rocking the incubator slightly will almost always get the baby to start breathing again, which increasing the heart rate. Neonatal intensive-care unit standard practice is to electronically monitor the heart and lungs.[citation needed]
Causes
Bradycardia arrhythmia may have many causes, both cardiac and non-cardiac.
Non-cardiac causes are usually secondary, and can involve recreational drug use or abuse, metabolic or endocrine issues, especially hypothyroidism, an electrolyte imbalance, neurological factors, autonomic reflexes, situational factors, such as prolonged bed rest, and autoimmunity.[26] At rest, although tachycardia is more commonly seen in fatty acid oxidation disorders, more rarely acute bradycardia can occur.[27]
Cardiac causes include acute or chronic ischemic heart disease, vascular heart disease, valvular heart disease, or degenerative primary electrical disease. Ultimately, the causes act by three mechanisms: depressed automaticity of the heart, conduction block, or escape pacemakers and rhythms.[28]
In general, two types of problems result in bradycardias: disorders of the SA node, and disorders of the AV node.[29]
With SA node dysfunction (sometimes called sick sinus syndrome), there may be disordered automaticity or impaired conduction of the impulse from the SA node into the surrounding atrial tissue (an "exit block"). Second-degree sinoatrial blocks can be detected only by use of a 12-lead ECG.[30] It is difficult and sometimes impossible to assign a mechanism to any particular bradycardia, but the underlying mechanism is not clinically relevant to treatment, which is the same in both cases of sick sinus syndrome: a permanent pacemaker.[28]
AV conduction disturbances (AV block; primary AV block, secondary type I AV block, secondary type II AV block, tertiary AV block) may result from impaired conduction in the AV node, or anywhere below it, such as in the bundle of His. The clinical relevance pertaining to AV blocks is greater than that of SA blocks.[30]
Beta blocker medicines also can slow the heart rate and decrease how forcefully the heart contracts. Beta-blockers may slow the heart rate to a dangerous level if prescribed with calcium channel blocker-type medications.[31] Bradycardia is also part of the mammalian diving reflex.[32]
Diagnosis
A diagnosis of bradycardia in adults is based on a heart rate less than 60 BPM,[1] although some studies use a heart rate of less than 50 BPM.[33] This is determined usually either by palpation or ECG.[1] If symptoms occur, a determination of electrolytes may be helpful in determining the underlying cause.[31]
Management
The treatment of bradycardia is dependent on whether or not the person is stable or unstable.[1][33]
Stable
Emergency treatment is not needed if the person is asymptomatic or minimally symptomatic.[33]
Unstable
If a person is unstable, the initial recommended treatment is intravenous atropine.[33] Doses less than 0.5 mg should not be used, as this may further decrease the rate.[33] If this is not effective, intravenous inotrope infusion (dopamine, epinephrine) or transcutaneous pacing should be used.[33] Transvenous pacing may be required if the cause of the bradycardia is not rapidly reversible.[33]
In children, giving oxygen, supporting their breathing, and chest compressions are recommended.[34][35]
Epidemiology
In clinical practice, elderly people over age 65 and young athletes of both sexes may have sinus bradycardia.[1] The US Centers for Disease Control and Prevention reported in 2011 that 15.2% of adult males and 6.9% of adult females had clinically-defined bradycardia (a resting pulse rate below 60 BPM).[36]
Society and culture
Records
- Daniel Green holds the world record for the slowest heartbeat in a healthy human, with a heart rate measured in 2014 of 26 BPM.[37]
- Martin Brady holds the Guinness world record for the slowest heart rate with a certified rate over a minute duration of 27 BPM.[38]
- Professional cyclist Miguel Indurain had, during his career, a resting heart rate of 28 BPM.[39]
See also
- Biology:Bezold–Jarisch reflex – Processes which cause hypopnea
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Hafeez, Yamama; Grossman, Shamai A. (2021-08-09). "Sinus bradycardia". StatPearls, NCBI Bookshelf, US National Institutes of Health. https://www.ncbi.nlm.nih.gov/books/NBK493201/.
- ↑ Patterson, Kirsten K.; Olgin, Jeffrey E. (2022). "Bradyarrhythmias and Atrioventricular Block" (in English). Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine (12th ed.). Philadelphia, PA: Elsevier. pp. 1312–1320. ISBN 978-0-323-82467-5.
- ↑ Rijnbeek, Peter R.; van Herpen, Gerard; Bots, Michiel L. et al. (2014). "Normal values of the electrocardiogram for ages 16-90 years". Journal of Electrocardiology 47 (6): 914–921. doi:10.1016/j.jelectrocard.2014.07.022. ISSN 1532-8430. PMID 25194872.
- ↑ Rijnbeek, Peter R. (2012). "Normal ECG values". http://www.normalecg.org/index.php/adult/standard.
- ↑ Kusumoto, Fred M.; Schoenfeld, Mark H.; Barrett, Coletta et al. (2019-08-20). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society" (in en). Circulation 140 (8): e382–e482. doi:10.1161/CIR.0000000000000628. ISSN 0009-7322. PMID 30586772.
- ↑ 6.0 6.1 6.2 6.3 Sidhu, Sunjeet; Marine, Joseph E. (July 2020). "Evaluating and managing bradycardia" (in en). Trends in Cardiovascular Medicine 30 (5): 265–272. doi:10.1016/j.tcm.2019.07.001. PMID 31311698.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 Patterson, Kirsten K.; Olgin, Jeffrey E. (2022). "Bradyarrhythmias and Atrioventricular Block" (in English). Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine (12th ed.). Philadelphia, PA: Elsevier. pp. 1312–1320. ISBN 978-0-323-82467-5.
- ↑ 8.0 8.1 8.2 Kusumoto, Fred M.; Schoenfeld, Mark H.; Barrett, Coletta et al. (2019-08-20). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society" (in en). Circulation 140 (8): e382–e482. doi:10.1161/CIR.0000000000000628. ISSN 0009-7322. PMID 30586772.
- ↑ Menozzi, Carlo; Brignole, Michele; Alboni, Paolo; Boni, Luca; Paparella, Nelly; Gaggioli, Germano; Lolli, Gino (November 1998). "The natural course of untreated sick sinus syndrome and identification of the variables predictive of unfavorable outcome". The American Journal of Cardiology 82 (10): 1205–1209. doi:10.1016/s0002-9149(98)00605-5. ISSN 0002-9149. PMID 9832095. https://doi.org/10.1016/S0002-9149(98)00605-5.
- ↑ Ye, Fan; Hatahet, Mohamad; Youniss, Mohamed A.; Toklu, Hale Z.; Mazza, Joseph J.; Yale, Steven (June 2018). "The Clinical Significance of Relative Bradycardia". WMJ 117 (2): 73–78. ISSN 1098-1861. PMID 30048576. https://pubmed.ncbi.nlm.nih.gov/30048576.
- ↑ Prutchi, David (2005). Design and Development of Medical Electronic Instrumentation. John Wiley & Sons. pp. 371. ISBN 9780471681830. https://books.google.com/books?id=Wtp5lg6UVygC&pg=PA371.
- ↑ 12.0 12.1 Loscalzo, Joseph; Keaney, John F.; MacRae, Calum A. (2022). "Basic Biology of the Cardiovascular System". Harrison's Principles of Internal Medicine (21st ed.). McGraw Hill.
- ↑ 13.0 13.1 13.2 13.3 Sauer, William H.; Koplan, Bruce A.; Zei, Paul C. (2022). "Principles of Clinical Cardiac Electrophysiology". Harrison's Principles of Internal Medicine (21st ed.). McGraw Hill.
- ↑ Kurian, Thomas; Ambrosi, Christina; Hucker, William; Fedorov, Vadim V.; Efimov, Igor R. (2010-02-18). "Anatomy and Electrophysiology of the Human AV Node: FUNCTIONAL ANATOMY OF AV NODE" (in en). Pacing and Clinical Electrophysiology 33 (6): 754–762. doi:10.1111/j.1540-8159.2010.02699.x. PMID 20180918.
- ↑ Kusumoto, Fred M.; Schoenfeld, Mark H.; Barrett, Coletta et al. (2019-08-20). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society" (in en). Circulation 140 (8): e382–e482. doi:10.1161/CIR.0000000000000628. ISSN 0009-7322. PMID 30586772.
- ↑ Bryan, Greg; Ward, Ann; Rippe, James M. (1992). "Athletic Heart Syndrome". Clinics in Sports Medicine (Elsevier) 11 (2): 259–272. doi:10.1016/S0278-5919(20)30529-9. PMID 1591784.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 Allan B. Wolfson, ed (2005). Harwood-Nuss' Clinical Practice of Emergency Medicine (4th ed.). Lippincott Williams & Wilkins. p. 260. ISBN 978-0-7817-5125-4.
- ↑ John, Roy M.; Kumar, Saurabh (2016-05-10). "Sinus Node and Atrial Arrhythmias" (in en). Circulation 133 (19): 1892–1900. doi:10.1161/CIRCULATIONAHA.116.018011. ISSN 0009-7322. PMID 27166347.
- ↑ 19.0 19.1 Sauer, William H.; Koplan, Bruce A. (2022). "The Bradyarrhythmias: Disorders of the Atrioventricular Node". Harrison's Principles of Internal Medicine (21st ed.). McGraw Hill.
- ↑ Clark, Bradley A.; Prystowsky, Eric N. (2021-12-01). "Electrocardiography of Atrioventricular Block" (in en). Cardiac Electrophysiology Clinics 13 (4): 599–605. doi:10.1016/j.ccep.2021.07.001. PMID 34689889. https://linkinghub.elsevier.com/retrieve/pii/S1877918221000800.
- ↑ Aro, A. L.; Anttonen, O.; Kerola, T.; Junttila, M. J.; Tikkanen, J. T.; Rissanen, H. A.; Reunanen, A.; Huikuri, H. V. (2014-01-02). "Prognostic significance of prolonged PR interval in the general population" (in en). European Heart Journal 35 (2): 123–129. doi:10.1093/eurheartj/eht176. ISSN 0195-668X. PMID 23677846.
- ↑ 22.0 22.1 22.2 Clark, Bradley A.; Prystowsky, Eric N. (December 2021). "Electrocardiography of Atrioventricular Block" (in en). Cardiac Electrophysiology Clinics 13 (4): 599–605. doi:10.1016/j.ccep.2021.07.001. PMID 34689889. https://linkinghub.elsevier.com/retrieve/pii/S1877918221000800.
- ↑ "AV Junctional Rhythm Disturbances (for Professionals)". American Heart Association. 4 December 2008. http://www.americanheart.org/presenter.jhtml?identifier=746.
- ↑ 24.0 24.1 "Arrhythmias and Conduction Disorders". The Merck Manuals: Online Medical Library. Merck Sharp and Dohme Corp. January 2008. http://www.merck.com/mmpe/sec07/ch075/ch075a.html.
- ↑ 25.0 25.1 "Ventricular escape rhythms". American Journal of Critical Care 12 (5): 477–8. September 2003. doi:10.4037/ajcc2003.12.5.477. PMID 14503433.
- ↑ Ye, Fan; Hatahet, Mohamad; Youniss, Mohamed A.; Toklu, Hale Z.; Mazza, Joseph J.; Yale, Steven (June 2018). "The Clinical Significance of Relative Bradycardia". WMJ 117 (2): 73–78. ISSN 1098-1861. PMID 30048576.
- ↑ Bonnet, D.; Martin, D.; Pascale De Lonlay, null; Villain, E.; Jouvet, P.; Rabier, D.; Brivet, M.; Saudubray, J. M. (1999-11-30). "Arrhythmias and conduction defects as presenting symptoms of fatty acid oxidation disorders in children". Circulation 100 (22): 2248–2253. doi:10.1161/01.cir.100.22.2248. ISSN 1524-4539. PMID 10577999.
- ↑ 28.0 28.1 "What is Bradycardia?". https://www.webmd.com/heart-disease/atrial-fibrillation/bradycardia.
- ↑ "Bradyarrhythmias". https://www.lecturio.com/concepts/bradyarrhythmias/.
- ↑ 30.0 30.1 Ufberg, JW; Clark, JS (February 2006). "Bradydysrhythmias and atrioventricular conduction blocks". Emerg. Med. Clin. North Am. 24 (1): 1–9, v. doi:10.1016/j.emc.2005.08.006. PMID 16308110.
- ↑ 31.0 31.1 "What is Bradycardia?". https://www.webmd.com/heart-disease/atrial-fibrillation/bradycardia.
- ↑ Michael Panneton, W. (2013). "The Mammalian Diving Response: An Enigmatic Reflex to Preserve Life?". Physiology 28 (5): 284–297. doi:10.1152/physiol.00020.2013. ISSN 1548-9213. PMID 23997188.
- ↑ 33.0 33.1 33.2 33.3 33.4 33.5 33.6 "Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation 122 (18 Suppl 3): S729–67. November 2010. doi:10.1161/CIRCULATIONAHA.110.970988. PMID 20956224.
- ↑ de Caen, AR; Berg, MD; Chameides, L et al. (3 November 2015). "Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.". Circulation 132 (18 Suppl 2): S526–42. doi:10.1161/cir.0000000000000266. PMID 26473000.
- ↑ Atkins, DL; Berger, S; Duff, JP et al. (3 November 2015). "Part 11: Pediatric Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.". Circulation 132 (18 Suppl 2): S519–25. doi:10.1161/cir.0000000000000265. PMID 26472999.
- ↑ Yechiam Ostchega (24 August 2011). "Resting Pulse Rate Reference Data for Children, Adolescents, and Adults: United States, 1999–2008". National Health Statistics Reports. Centers for Disease Control. https://www.cdc.gov/nchs/data/nhsr/nhsr041.pdf.
- ↑ "Slowest heart rate: Daniel Green breaks Guinness World Records record". World Record Academy. 29 November 2014. http://www.worldrecordacademy.com/medical/slowest_heart_rate_Daniel_Green_breaks_Guinness_World_Records_record_214157.html.
- ↑ "Lowest heart rate". Guinness World Records. 11 August 2005. http://www.guinnessworldrecords.com/world-records/lowest-heart-rate.
- ↑ Lovgren, Stefan (20 August 2004). "Olympic Gold Begins With Good Genes, Experts Say". National Geographic News. http://news.nationalgeographic.com/news/2004/08/0820_040820_olympics_athletes.html.
| Classification |
|---|
 |
