Medicine:Rhizomelic chondrodysplasia punctata
| Rhizomelic chondrodysplasia punctata | |
|---|---|
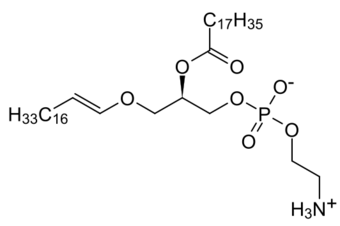 | |
| Low levels of plasmalogens is a characteristic of rhizomelic chondrodysplasia punctata. | |
| Symptoms | Alopecia, flat face[1] |
| Causes | PEX7 gene, GNPAT gene and AGPS gene mutations[2] |
| Diagnostic method | Clinical and radiologic finding[3] |
| Treatment | Physical therapy[4] |
Rhizomelic chondrodysplasia punctata is a rare developmental brain disorder characterized by abnormally short arms and legs (rhizomelia), seizures, recurrent respiratory tract infections and congenital cataracts.
The cause is a genetic mutation that results in low levels of plasmalogens, which are a type of lipid found in cell membranes throughout the body, but whose function is not known.[2]
Signs and symptoms
Rhizomelic chondrodysplasia punctata has the following symptoms:[4][1]
- Bilateral shortening of the femur, resulting in short legs
- Post-natal growth problems (deficiency)
- Cataracts
- Intellectual disability
- Possible seizures
- Possible infections of respiratory tract
Genetics
This condition is a consequence of mutations in the PEX7 gene, the GNPAT gene (which is located on chromosome 1) or the AGPS gene. The condition is acquired in an autosomal recessive manner.[2]
Pathophysiology
The mechanism of rhizomelic chondrodysplasia punctata in the case of type 1 of this condition involves a defect in PEX7, whose product is involved in peroxisome assembly. There are 3 pathways that depend on peroxisomal biogenesis factor 7 activities, including:[4][5][verification needed]
- AGPS (catalyzes plasmalogen biosynthesis)
- PhYH (catalyzes catabolism of phytanic acid)
- ACAA1 (catalyzes beta-oxidation of VLCFA - straight)
Diagnosis

The diagnosis of rhizomelic chondrodysplasia punctata can be based on genetic testing[6] as well as radiography results, plus a physical examination of the individual.[3]
Types
- Type 1 (RCDP1) is associated with PEX7 mutations; these are peroxisome biogenesis disorders where proper assembly of peroxisomes is impaired.[4]
- Type 2 (RCDP2) is associated with DHAPAT mutations.[7]
- Type 3 (RCDP3) is associated with AGPS mutations.[8]
Treatment
Management of rhizomelic chondrodysplasia punctata can include physical therapy; additionally orthopedic procedures improved function sometimes in affected people.[4]
Prognosis
The prognosis is poor in this condition,[3] and most children die before the age of 10.[4] However, some survive to adulthood, especially if they have a non-classical (mild) form of RCDP.[4]
Children with classical, or severe, RCDP1 have severe developmental disabilities. Most of them achieve early developmental skills, such as smiling, but they will not develop skills expected from a baby older than six months (such as feeding themselves or walking).[4] By contrast, children with non-classical mild RCDP1 often learn to walk and talk.[4]
See also
References
- ↑ 1.0 1.1 "Rhizomelic chondrodysplasia punctata type 1". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. US National Library of Medicine. https://rarediseases.info.nih.gov/diseases/6049/rhizomelic-chondrodysplasia-punctata-type-1.
- ↑ 2.0 2.1 2.2 Reference, Genetics Home. "rhizomelic chondrodysplasia punctata". https://ghr.nlm.nih.gov/condition/rhizomelic-chondrodysplasia-punctata.
- ↑ 3.0 3.1 3.2 "Rhizomelic chondrodysplasia punctata". Orphanet. http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=177.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Braverman, Nancy E.; Moser, Ann B.; Steinberg, Steven J. (2020). "Rhizomelic Chondrodysplasia Punctata Type 1". GeneReviews. NBK1270. PMID 20301447. https://www.ncbi.nlm.nih.gov/books/NBK1270/.
- ↑ Brodsky, Michael C. (2016-06-28) (in en). Pediatric Neuro-Ophthalmology. Springer. pp. 620. ISBN 9781493933846. https://books.google.com/books?id=f_mODAAAQBAJ&q=rhizomelic+chondrodysplasia+punctata+mechanism&pg=PA620.
- ↑ "Rhizomelic chondrodysplasia punctata type 1". Genetics Testing Laboratory (GTR): Conditions. US National Library of Medicine. https://www.ncbi.nlm.nih.gov/gtr/conditions/C1859133/.
- ↑ Online Mendelian Inheritance in Man (OMIM) Rhizomelic Chondrodysplasia Punctata, Type 2; RCDP2 -222765
- ↑ Online Mendelian Inheritance in Man (OMIM) Rhizomelic Chondrodysplasia Punctata, Type 3; RCDP3 -600121
Further reading
- Benacerraf, Beryl (2007). Ultrasound of fetal syndromes (2nd ed.). Philadelphia: Churchill Livingstone / Elsevier. ISBN 978-0443066412. https://books.google.com/books?id=1MHFF0UOKAUC&q=rhizomelic+chondrodysplasia+punctata&pg=PA267. Retrieved 23 January 2017.
- Ashwal, Stephen; Ferriero, Donna M.; Schor, Nina F. (2012). Swaiman, Kenneth F.. ed. Swaiman's pediatric neurology principles and practice (5th ed.). [Edinburgh]: Elsevier Saunders. ISBN 978-0323089111. https://books.google.com/books?id=bonlLHarTFAC&q=rhizomelic+chondrodysplasia+punctata&pg=PA477. Retrieved 23 January 2017.
- "Rhizomelic Chondrodysplasia Punctata Type 1". GeneReviews® [Internet] (University of Washington). 2020. NBK1270. PMID 20301447. https://www.ncbi.nlm.nih.gov/books/NBK1270/.
- "Chondrodysplasia Punctata 1, X-Linked". GeneReviews® [Internet] (University of Washington). 2020. PMID 20301713. https://www.ncbi.nlm.nih.gov/books//.
- "Chondrodysplasia Punctata 2, X-Linked". GeneReviews® [Internet] (University of Washington). 2020. NBK55062. PMID 21634086. https://www.ncbi.nlm.nih.gov/books/NBK55062/.
External links
| Classification | |
|---|---|
| External resources |
 |


